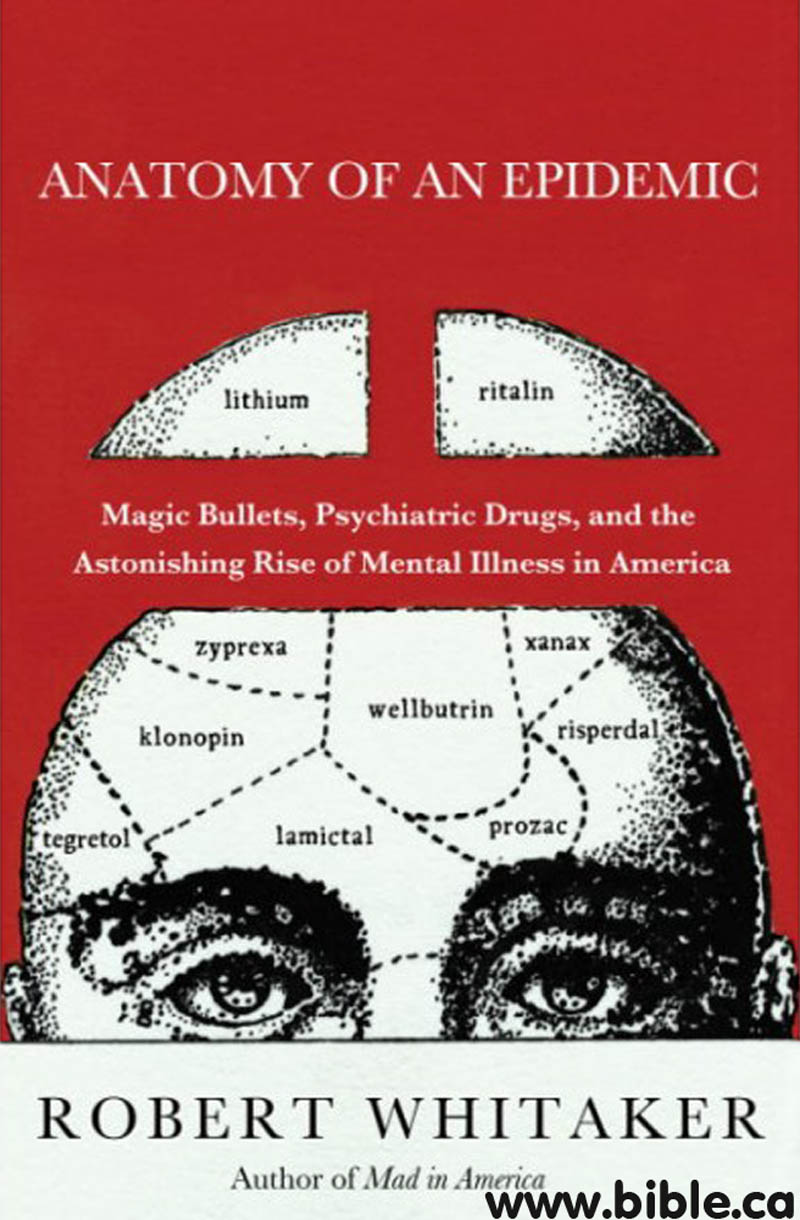
Anatomy of an Epidemic
Robert
Whitaker
2010 AD
|
|
Review:
- The author had blindly accepted that chemical imbalances were a proved testable measurable fact of science. When he first heard someone suggest biochemical imbalances of brain neurotransmitters was a myth, he dismissed it as ridiculous. Then came the anonymous envelope of information that changes his view and motivated him to write this amazing must read book.
- A reporter, Robert Whitaker, publishes a story on how well a new psychiatric drug works only to have an anonymous envelope sent to him with the stunning truth that told the opposite untold story.
- This fabulous book is written like a spy movie except it is non-fiction.
- It shows that psychiatric drugs do not work, cause devastating physical side effects and debilitating withdrawal effects when you try to escape and become drug free.
- If you are on neuroleptic drugs or any drug prescribed by any doctor for anxiety, depression, schizophrenia etc., you must buy this book.... it may save your life.
- We highly recommend this book.
(Anatomy of an Epidemic, Robert Whitaker, 2010 AD)
“ (Anatomy of an Epidemic, Robert Whitaker
Perhaps the one telltale sign that the meeting was for people diagnosed with a mental illness was that a fair number were overweight. People diagnosed with bipolar disorder are often prescribed an atypical antipsychotic, such as Zyprexa, and those drugs regularly cause people to put on the pounds.” (Anatomy of an Epidemic, Robert Whitaker, p13
Perhaps the one telltale sign that the meeting was for people diagnosed with a mental illness was that a fair number were overweight. People diagnosed with bipolar disorder are often prescribed an atypical antipsychotic, such as Zyprexa, and those drugs regularly cause people to put on the pounds.” (Anatomy of an Epidemic, Robert Whitaker, 2010 AD, p13
Psychiatry now has three classes of medications it uses to treat affective disorders—antidepressants, mood stabilizers, and atypical antipsychotics—but for whatever reason, an ever greater number of people are showing up at DBSA meetings around the country, telling of their persistent and enduring struggles with depression or mania or both. ” (Anatomy of an Epidemic, Robert Whitaker, p15
“The meds isolate you. They interfere with your empathy. There is a flatness to you, and so you are uncomfortable with people all the time. They make it hard for you to get along. The drugs may take care of aggression and anxiety and some paranoia, those sorts of symptoms, but they don't help with the empathy that helps you get along with people.”, Quoting Cathy Levin.” (Anatomy of an Epidemic, Robert Whitaker, p19
He began tonguing the antipsychotic medication and spitting it out when the staff weren't looking. “I could think again,” he says. “The antipsychotic drugs weren't letting me think. I was like a vegetable, and I couldn't do anything. I had no emotions. I sat there and watched television. But now I felt more in control. And it felt great to feel alive again.”, quoting George Badillo.” (Anatomy of an Epidemic, Robert Whitaker, p 23
in 2003 she [Dorea Vierling-Clausen] stumbled across some literature that raised questions about Zyprexa's longterm safety and the merits of antipsychotic drugs. That led her to wean herself from that drug, and while that process was “pure hell”—she suffered terrible anxiety, severe panic attacks, paranoia, and horrible tremors—she eventually did get off that medication. She then decided to see if she could get off the benzodiazepine she was taking, Klonopin, and that turned into another horrible withdrawal experience, as she suffered such severe headaches she'd be in bed by noon. Still, she was gradually undoing her drug cocktail, and that caused her to question her bipolar diagnosis. She had first seen a therapist because she cried too much. There had been no mania—her sleeplessness and agitation hadn't arisen until after she had been placed on an antidepressant. Could she just have been a moody teenager who had some growing up to do? .” (Anatomy of an Epidemic, Robert Whitaker, p 29
“When I was 'bipolar,' I had an excuse for any unpredictable or unstable behavior. I had permission to behave in that way, but now I am holding myself to the same behavioral standards as everyone else, and it turns out I can meet them. This is not to say that I don't have bad days. I do, and I may still worry more than the average Joe, but not that much more.” (Anatomy of an Epidemic, Robert Whitaker, quoting Dorea Vierling-Clausen, p 30
U.S. psychiatrists dubbed chlorpromazine, which was marketed in the United States as Thorazine, as a “major tranquilizer.” Back in France, Delay and Deniker coined a more precise scientific term: This new drug was a “neuroleptic,” meaning it took hold of the nervous system. Chlorpromazine, they concluded, induced deficits similar to those seen in patients ill with encephalitis lethargica. “In fact,” Deniker wrote, “it would be possible to cause true encephalitis epidemics with the new drugs. Symptoms progressed from reversible somnolence to all types of dyskinesia and hyperkinesia, and finally to parkinsonism.”6 Physicians in the United States similarly understood that this new drug was not fixing any known pathology. “We have to remember that we are not treating diseases with this drug,” said psychiatrist E. H. Parsons, at a 1955 meeting in Philadelphia on chlorpromazine. “We are using a neuropharmacologic agent to produce a specific effect.” Fn 7[Symposium proceedings, Chlorpromazine and Mental Health (Philadelphia: Lea and Fabiger, 1955), 132.], p50
psychiatry-harms-damages-society-anti-psychotic-drugs-cause-brain-damage-chlorpromazine-thorazine-1950ad.htm
psychiatry-harms-damages-society-anti-psychotic-drugs-cause-brain-damage-meprobamate-miltown-happy-pills-1953ad.htm
The brain is a machine that consists of sparks and soups.
During the 1960s, scientists at the NIMH and elsewhere figured out how iproniazid and imipramine worked. The transmission of signals from the “presynaptic” neuron to the “postsynaptic” neuron needs to be lightning fast and sharp, and in order for the signal to be terminated, the chemical messenger must be removed from the synapse. This is done in one of two ways. Either the chemical is metabolized by an enzyme and shuttled off as waste, or else it flows back into the presynaptic neuron. Researchers discovered that iproniazid thwarts the first process. It blocks an enzyme, known as monoamine oxidase, that metabolizes norepinephrine and serotonin. As a result, the two chemical messengers remain in the synapse longer than normal. Imipramine inhibits the second process. It blocks the “reuptake” of norepinephrine and serotonin by the presynaptic neuron, and thus, once again, the two chemicals remain in the synapse longer than normal. Both drugs produce a similar end result, although they do so by different means. .” (Anatomy of an Epidemic, Robert Whitaker, p62
All of this physiology—the 100 billion neurons, the 150 trillion synapses, the various neurotransmitter pathways—tell of a brain that is almost infinitely complex. Yet the chemical imbalance theory of mental disorders boiled this complexity down to a simple disease mechanism, one easy to grasp. In depression, the problem was that the serotonergic neurons released too little serotonin into the synaptic gap, and thus the serotonergic pathways in the brain were “underactive.” Antidepressants brought serotonin levels in the synaptic gap up to normal, and that allowed these pathways to transmit messages at a proper pace. Meanwhile, the hallucinations and voices that characterized schizophrenia resulted from overactive dopaminergic pathways. Either the presynaptic neurons pumped out too much dopamine into the synapse or the target neurons had an abnormally high density of dopamine receptors. Antipsychotics put a brake on this system, and this allowed the dopaminergic pathways to function in a more normal manner.
That was the chemical imbalance theory put forth by Schildkraut and Jacques Van Rossum, and the very research that had led Schildkraut to his hypothesis also provided investigators with a method for testing it. The studies of iproniazid and imipramine had shown that neurotransmitters were removed from the synapse in one of two ways. Either the chemical was taken back up into the presynaptic neuron and restored for later use, or it was metabolized by an enzyme and carted off as waste. Serotonin is metabolized into 5-hydroxyindole acetic acid (5-HIAA); dopamine is turned into homovanillic acid (HVA). Researchers could comb the cerebrospinal fluid for these metabolites, and the amounts found would serve as an indirect gauge of the synaptic levels of the neurotransmitters. Since low serotonin was theorized to cause depression, anyone in that emotional state should have lower-than-normal levels of 5-HIAA in his or her cerebrospinal fluid. Similarly, since an overactive dopamine system was theorized to cause schizophrenia, people who heard voices or were paranoid should have abnormally high cerebrospinal levels of HVA. .” (Anatomy of an Epidemic, Robert Whitaker , p 70
“contrary to expectations, no relationships between cerebrospinal 5-HIAA and response to amitriptyline were found.” Fn 10. Moreover, he and the other NIMH researchers discovered—just as Asberg had—that 5-HIAA levels varied widely in depressed patients. Some had high levels of serotonin metabolites in their cerebrospinal fluid, while others had low levels. The NIMH scientists drew the only possible conclusion: “Elevations or decrements in the functioning of serotonergic systems per se are not likely to be associated with depression.” Fn 10[J. Maas, “Pretreatment neurotransmitter metabolite levels and response to tricyclic antidepressant drugs,” American Journal of Psychiatry 141 (1984): 1159-71.], p 74
“I spent the first several years of my career doing full-time research on brain serotonin metabolism, but I never saw any convincing evidence that any psychiatric disorder, including depression, results from a deficiency of brain serotonin,” said Stanford psychiatrist David Burns in 2003. Fn 11 [J. Lacasse, “Serotonin and depression: a disconnect between the advertisements and the scientific literature,” PloS Medicine 2 (2005): 1211-16.], p 74
“There is no scientific evidence whatsoever that clinical depression is due to any kind of biological deficit state,” wrote Colin Ross, an associate professor of psychiatry at Southwest Medical Center in Dallas, in his 1995 book, Pseudoscience in Biological Psychiatry. Fn 12 [C. Ross, Pseudoscience in Biological Psychiatry (New York: John Wiley & Sons, 1995), 111.], p 74
Contemporary neuroscience research has failed to confirm any serotonergic lesion in any mental disorder, and has in fact provided significant counterevidence to the explanation of a simple neurotransmitter deficiency. Modern neuroscience has instead shown that the brain is vastly complex and poorly understood. While neuroscience is a rapidly advancing field, to propose that researchers can objectively identify a “chemical imbalance” at the molecular level is not compatible with the extant science. In fact, there is no scientifically established ideal “chemical balance” of serotonin, let alone an identifiable pathological imbalance. To equate the impressive recent achievements of neuroscience with support for the serotonin hypothesis is a mistake. … Yet, as previously mentioned, there is no such thing as a scientifically established correct “balance” of serotonin. The take-home message for consumers viewing SSRI advertisements is probably that SSRIs work by normalizing neurotransmitters that have gone awry. This was a hopeful notion 30 years ago, but is not an accurate reflection of present-day scientific evidence. … Consider the medical textbook, Essential Psychopharmacology, which states, “So far, there is no clear and convincing evidence that monoamine deficiency accounts for depression; that is, there is no ‘real’ monoamine deficit” (Serotonin and Depression: A Disconnect between the Advertisements and the Scientific Literature, Jeffrey R. Lacasse, Jonathan Leo, PloS Medicine 2, 2005 AD)
“The serotonin theory of depression,” he wrote, with evident exasperation, “is comparable to the masturbatory theory of insanity.” Fn 14 [David Healy, “Ads for SSRI antidepressants are misleading,” PloS Medicine news release, November 2005], p 74
In 1978, Philip Seeman at the University of Toronto announced in Nature that this was indeed the case. At autopsy, the brains of twenty schizophrenics had 70 percent more D2 receptors than normal. At first glance, it seemed that the cause of schizophrenia had been found, but Seeman cautioned that all of the patients had been on neuroleptics prior to their deaths. “Although these results are apparently compatible with the dopamine hypothesis of schizophrenia in general,” he wrote, the increase in D2 receptors might “have resulted from the long-term administration of neuroleptics.” T. Lee, “Binding of 31-1-neuroleptics and 3H-apomorphine in schizophrenic brains,” Nature 374 (1978): 897-900.Fn 20
A variety of studies quickly proved that the drugs were indeed the culprit. When rats were fed neuroleptics, their D2 receptors quickly increased in number. D. Burt, “Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain,” Science 196 (1977): 326-27.Fn 21
If rats were given a drug that blocked D, receptors, that receptor subtype increased in density. M. Porceddu, “[3H]SCH 23390 binding sites increase after chronic blockade of d-1 dopamine receptors,” European Journal of Pharmacology 118 (1985): 367-70.Fn 22
, In each instance, the increase was evidence of the brain trying to compensate for the drug's blocking of its signals. Then, in 1982, Angus MacKay and his British colleagues reported that when they examined brain tissue from forty-eight deceased schizophrenics, “the increases in [D2] receptors were seen only in patients in whom neuroleptic medication had been maintained until the time of death, indicating that they were entirely iatrogenic [drug-caused].” A. MacKay, “Increased brain dopamine and dopamine receptors in schizophrenia,” Archives of General Psychiatry 39 (1982): 991-97.Fn 23
A few years later, German investigators reported the same results from their autopsy studies. J. Kornhuber, “3H-spiperone binding sites in post-mortem brains from schizophrenic patients,” Journal of Neural Transmission 75 (1989): 1-10.Fn 24
Finally, investigators in France, Sweden, and Finland used positron emission topography to study D2-receptor densities in living patients who had never been exposed to neuroleptics, and all reported “no significant differences” between the schizophrenics and “normal controls.” Fn 25 [J. Martinot, “Striatal D2 dopaminergic receptors assessed with positron emission tomography and bromospiperone in untreated schizophrenic patients,” American Journal of Psychiatry 147 (1990): 44-50; L. Farde, “D2 dopamine receptors in neuroleptic-naive schizophrenic patients,” Archives of General Psychiatry 47 (1990): 213-19; J. Hietala, “Striatal D2 dopamine receptor characteristics in neurolepticnaïve schizophrenic patients studied with positron emission tomography,” Archives of General Psychiatry 51 (1994): 116-23.] p76
“The dopaminergic theory of schizophrenia retains little credibility for psychiatrists,” observed Pierre Deniker in 1990.26 Four years later, John Kane, a well-known psychiatrist at Long Island Jewish Medical Center, echoed the sentiment, noting that there was “no good evidence for any perturbation of the dopamine function in schizophrenia.” J. Kane, “Towards more effective antipsychotic treatment,” British Journal of Psy-chiatry 165, suppl. 25 (1994): 22-31. Fn 27
, Molecular Neuropharmacology, was moved to once again remind readers of the truth. “There is no compelling evidence that a lesion in the dopamine system is a primary cause of schizophrenia,” he wrote. E. Nestler and S. Hyman, Molecular Neuropharmacology (New York: McGraw Hill, 2002), 392Fn 28
The low-serotonin hypothesis of depression and the high-dopamine hypothesis of schizophrenia had always been the twin pillars of the chemical-imbalance theory of mental disorders, and by the late 1980s, both had been found wanting. Other mental disorders have also been touted to the public as diseases caused by chemical imbalances, but there was never any evidence to support those claims.” (Anatomy of an Epidemic, Robert Whitaker p 77
In 1990, Deniker said that the same was true of the dopamine hypothesis of schizophrenia. When psychiatric researchers recast the drugs as “antischizophrenic” agents, he noted, they had gone “a bit far . . . one can say that neuroleptics diminish certain phenomena of schizophrenia, but [the drugs] do not pretend to be an etiological treatment of these psychoses.” fn 30 P. Deniker, “The neuroleptics: a historical survey,” Acta Psychiatrica Scandinavica 82, suppl. 358(1990): 83-87. Also: “From chlorpromazine to tardive dyskinesia,” Psychiatric Journal of the University of Ottawa 14 (1989): 253-59., p78
“The evidence does not support any of the biochemical theories of mental illness,” concluded Elliot Valenstein, a professor of neuroscience at the University of Michigan, in his 1998 book Blaming the Brain. E. Valenstein, Blaming the Brain (New York: The Free Press, 1998), 96.fn 32
Even U.S. surgeon general David Satcher, in his 1999 report Mental Health, confessed that “the precise causes [etiologies] of mental disorders are not known.” U.S. Department of Health and Human Services, Mental Health: A Report of the Surgeon General (1999), 3, 68, 78.fn 33
In Prozac Backlash, Joseph Glenmullen, an instructor of psychiatry at Harvard Medical School, noted that “in every instance where such an imbalance was thought to be found, it was later proved to be false.” J. Glenmullen, Prozac Backlash (New York: Simon & Schuster, 2000), 196.fn 34
But the medicine clearly doesn't fix a chemical imbalance in the brain. Instead, it does precisely the opposite. Prior to being medicated, a depressed person has no known chemical imbalance. Fluoxetine then gums up the normal removal of serotonin from the synapse, and that triggers a cascade of changes, and several weeks later the serotonergic pathway is operating in a decidedly abnormal manner. The presynaptic neuron is putting out more serotonin than usual. Its serotonin reuptake channels are blocked by the drug. The system's feedback loop is partially disabled. The postsynaptic neurons are “desensitized” to serotonin. Mechanically speaking, the serotonergic system is now rather mucked up. Eli Lilly's scientists were well aware that this was so.” (Anatomy of an Epidemic, Robert Whitaker, p81
In 1991, in a paper published in the Journal of Clinical Psychiatry, Princeton neuroscientist Barry Jacobs made this very point about SSRIs. He wrote:
These drugs “alter the level of synaptic transmission beyond the physiologic range achieved under [normal] environmental/biological conditions. Thus, any behavioral or physiologic change produced under these conditions might more appropriately be considered pathologic, rather than reflective of the normal biological role of 5-HT [serotonin.] “ B. Jacobs, “Serotonin and behavior,” Journal of Clinical Psychiatry 52, suppl. (1991): 151-62. fn 44
Thorazine and other standard antipsychotics block 70 to 90 percent of all D2 receptors in the brain. In response, the presynaptic neurons begin pumping out more dopamine and the postsynaptic neurons increase the density of their D2 receptors by 30 percent or more. In this manner, the brain is trying to “compensate” for the drug's effects so that it can maintain the transmission of messages along its dopaminergic pathways. However, after about three weeks, the pathway's feedback mechanism begins to fail, and the presynaptic neurons begin to fire in irregular patterns or turn quiescent. It is this “inactivation” of dopaminergic pathways that “may be the basis for the antipsychotic action,” explains the American Psychiatric Association's Textbook of Psychopharmacology. fn 45 Schatzberg, Textbook of Psychopharmacology, 619., p82
Here's the data. In a study conducted by the NIMH, 62 percent of first-episode psychotic patients admitted to Warren State Hospital in Pennsylvania from 1946 to 1950 were discharged within twelve months. At the end of three years, 73 percent were out of the hospital. fn 4 J. Cole, editor, Psychopharmacology (Washington, DC: National Academy of Sciences, 1959), 142. p 92
A study of 216 schizophrenia patients admitted to Delaware State Hospital from 1948 to 1950 produced similar results. Eighty-five percent were discharged within five years, and on January 1, 1956—six years or more after initial hospitalization- 70 percent were successfully living in the community. fn 5J. Cole, editor, Psychopharmacology (Washington, DC: National Academy of Sciences, 1959), 386-87., p92
Meanwhile, Hillside Hospital in Queens, New York, tracked 87 schizophrenia patients discharged in 1950 and determined that slightly more than half never relapsed in the next four years. fn 6 N. Lehrman, “Follow-up of brief and prolonged psychiatric hospitalization,” Com-prehensive Psychiatry 2 (1961): 227-40. p 92
During this period, outcomes studies in England, where schizophrenia was more narrowly defined, painted a similarly encouraging picture: Thirty-three percent of the patients enjoyed a “complete recovery,” and another 20 percent a “social recovery,” which meant they could support themselves and live independently. fn 7 R. Warner, Recovery from Schizophrenia (Boston: Routledge & Kegan Paul, 1985), 74., p92
It is also important to note that the arrival of Thorazine did not improve discharge rates in the 1950s for people newly diagnosed with schizophrenia, nor did its arrival trigger the release of chronic patients. In 1961, the California Department of Mental Hygiene reported on discharge rates for all 1,413 first-episode schizophrenia patients hospitalized in 1956, and it found that 88 percent of those who weren't prescribed a neuroleptic were discharged within eighteen months. Those treated with a neuroleptic—about half of the 1,413 patients—had a lower discharge rate; only 74 percent were discharged within eighteen months. This is the only large-scale study from the 1950s that compared discharge rates for first-episode patients treated with. and without drugs, and the investigators concluded that “drug-treated patients tend to have longer periods of hospitalization. . . . The untreated patients consistently show a somewhat lower retention rate.” fn 8 L. Epstein, “An approach to the effect of ataraxic drugs on hospital release rates,” American Journal of Psychiatry 119 (1962): 246-61.
, p93
“patients who received placebo treatment [in the six-week trial] were less likely to be rehospitalized than those who received any of the three active phenothiazines.” N. Schooler, “One year after discharge,” American Journal of Psychiatry 123 (1967): 986-95.fn 20
“Relapse was found to be significantly related to the dose of the tranquilizing medication the patient was receiving before he was put on placebo--the higher the dose, the greater the probability of relapse,” the researchers wrote. fn 21 R. Prien, “Discontinuation of chemotherapy for chronic schizophrenics,” Hospital and Community Psychiatry 22 (1971): 20-23., p 99.
“revolving door syndrome.” Even when patients reliably took their medications, relapse was common, and researchers observed that “relapse is greater in severity during drug administration than when no drugs are given.” G. Gardos and J. Cole, “Maintenance antipsychotic therapy: is the cure worse than the disease?” American Journal of Psychiatry 133 (1977): 32-36.fn 22
“Our findings suggest that antipsychotic medication is not the treatment of choice, at least for certain patients, if one is interested in long-term clinical improvement,” Rappaport wrote. “Many unmedicated-while-in-hospital patients showed greater long-term improvement, less pathology at follow-up, fewer hospitalizations, and better overall functioning in the community thatn patients who were given chlorpromazine while in the hospital. fn 26 M. Rappaport, “Are there schizophrenics for whom drugs may be unnecessary or contraindicated?” International Pharmacopsychiatry 13 (1978): 100-11., p102
Rappaport's Study:Three-Year Schizophrenia Outcomes
|
Medication Use (In hospital/ after discharge) |
Number of Patients |
Severity Illness Scale (1=best outcome; 7=worst outcome) |
Rehospitalization |
|
Placebo/off |
24 |
1.70 |
8% |
|
Antipsychotic/off |
17 |
2.79 |
47% |
|
Placebo/on |
17 |
3.54 |
53% |
|
Antipsychotic/on |
22 |
3.51 |
73% |
In this study, patients were grouped according to both their in-hospital care (placebo or drug) and whether they used antipsychotics after they were discharged. Thus, 24 of the 41 patients treated with placebo in the hospital remained off the drugs during the follow-up period. This never-exposed group had the best outcomes by far. Rappaport, M. “Are there schizophrenics for whom drugs may be unnecessary or contraindicated!' International Pharmacopsychiatry 13 (1978): 100-11.
All of this required psychiatry to recalculate the risks and benefits of antipsychotics, and in 1977 Jonathan Cole did so in an article provocatively titled “Is the Cure Worse Than the Disease?” He reviewed all of the long-term harm the drugs could cause and observed that studies had shown that at least 50 percent of all schizophrenia patients could fare well without the drugs. There was only one moral thing for psychiatry to do: “Every schizophrenic outpatient maintained on antipsychotic medication should have the benefit of an adequate trial without drugs.” This, he explained, would save many “from the dangers of tardive dyskinesia as well as the financial and social burdens of prolonged drug therapy.” Gardos and Cole, “Maintenance antipsychotic therapy.” fn 32
A simple metaphor can help us better understand this drug-induced biological vulnerability to psychosis and why it flares up when the drug is withdrawn. Neuroleptics put a brake on dopamine transmission, and in response the brain puts down the dopamine accelerator (the extra D2 receptors). If the drug is abruptly withdrawn, the brake on dopamine is suddenly released while the accelerator is still pressed to the floor. The system is now wildly out of balance, and just as a car might careen out of control, so too the dopaminergic pathways in the brain. The dopaminergic neurons in the basal ganglia may fire so rapidly that the patient withdrawing from the drugs suffers weird tics, agitation, and other motor abnormalities. The same out-of-control firing is happening with the dopaminergic pathway to the limbic region, and that may lead to “psychotic relapse or deterioration,” Chouinard and Jones wrote. G. Chouinard, “Neuroleptic-induced supersensitivity psychosis: Clinical and phar-macologic characteristics,” American Journal of Psychiatry 137 (1980): 16-20. fn 35
(he reported that for every month of exposure, it took two months for renormalization to occur), at some point the increase in receptors became irreversible. P. Muller, “Dopaminergic supersensitivity after neuroleptics,” Psychopharmacology 60 (1978): 1-11. fn 38
It was Chouinard and Jones who explicitly connected all the dots, and for a time, their work did stir up a hornet's nest within psychiatry. One physician, at a meeting where the two McGill University doctors spoke, asked in astonishment: “I put my patients on neuroleptics because they're psychotic. Now you're saying that the same drug that controls their schizophrenia also causes a psychosis?” P. Breggin, Brain Disabling Treatments in Psychiatry (New York: Springer Publishing Company, 1997), 60. fn 40
The Vermont longitudinal study
In the late 1950s and early 1960s, Vermont State Hospital discharged 269 chronic schizophrenics, most of whom were middle-aged, into the community. Twenty years later, Courtenay Harding interviewed 168 patients from this cohort (those who were still alive), and found that 34 percent were recovered, which meant they were “asymptomatic and living independently, had close relationships, were employed or otherwise productive citizens, were able to care for themselves, and led full lives in general.” C. Harding, “The Vermont longitudinal study of persons with severe mental ill-ness,” American Journal of Psychiatry 144 (1987): 727-34; C. Harding, “The Vermont longitudinal study of persons with severe mental illness, II,” American Journal of Psychiatry 144 (1987): 727-35.42
This was a startling good long-term outcome for patients who had been seen as hopeless in the 1950s, and those who had recovered, Harding told the APA Monitor, had one thing in common: They all “had long since stopped taking medications. “ P. McGuire, “New hope for people with schizophrenia,” APA Monitor 31 (February 2000).
fn 43
She concluded that it was a “myth” that schizophrenia patients “must be on medication all their lives,” and that, in fact, “it may be a small percentage who need medication indefinitely.” C. Harding, “Empirical correction of seven myths about schizophrenia with implications for treatment,” Acta Psychiatrica Scandinavica 384, suppl. (1994): 14-16.fn 44
The World Health Organization cross-cultural studies
In 1969, the World Health Organization launched an effort to track schizophrenia outcomes in nine countries. At the end of five years, the patients in the three “developing” countries—India, Nigeria, and Colombia—had a “considerably better course and outcome” than patients in the United States and five other “developed countries.” They were much more likely to be asymptomatic during the follow-up period, and even more important, they enjoyed “an exceptionally good social outcome.”
These findings stung the psychiatric community in the United States and Europe, which protested that there must have been a design flaw in the study. Perhaps the patients in India, Nigeria, and Colombia had not really been schizophrenic. In response, WHO launched a ten-country study in 1978, and this time they primarily enrolled patients suffering from a first episode of schizophrenia, all of whom were diagnosed by Western criteria. Once again, the results were much the same. At the end of two years, nearly two-thirds of the patients in the “developing countries” had had good outcomes, and slightly more than one-third had become chronically ill. In the rich countries, only 37 percent of the patients had good outcomes, and 59 percent became chronically ill. “The findings of a better outcome of patients in developing countries was confirmed,” the WHO scientists wrote. “Being in a developed country was a strong predictor of not attaining a complete remission.” A. Jablensky, “Schizophrenia: manifestations, incidence and course in different cultures,” Psychological Medicine 20, monograph (1992): 1-95. fn 45
Although the WHO investigators
didn't identify a reason for the stark disparity in outcomes, they had tracked
antipsychotic usage in the second study, having hypothesized that perhaps
patients in the poor countries fared better because they more reliably took
their medication. However, they found the opposite to be true. Only 16 percent
of the patients in the poor countries were regularly maintained on
antipsychotics, versus 61 percent of the patients in the rich countries.
Moreover, in Agra, India, where patients arguably fared the best, only 3
percent of the patients were kept on an
antipsychotic. Medication usage was highest in Moscow, and that
city had the highest percentage of patients who were constantly ill. fn 46 A. Jablensky, “Schizophrenia: manifestations, incidence and course in
different cultures,” Psychological Medicine 20, monograph
(1992): 1-95. See tables on page 60 for medication usage by individual centers;
see table on page 64 for medication usage by developing and developed
countries.
MRI studies
The invention of magnetic resonance imaging technology provided researchers with the opportunity to measure volumes of brain structures in people diagnosed with schizophrenia, and while they hoped to identify abnormalities that might characterize the illness, they ended up documenting instead the effect of antipsychotics on brain volumes. In a series of studies from 1994 to 1998, investigators reported that the drugs caused basal ganglion structures and the thalamus to swell, and the frontal lobes to shrink, with these changes in volumes “dose related.” 51. M. Chakos, “Increase in caudate nuclei volumes of first-episode schizophrenic pa-tients taking antipsychotic drugs,” American Journal of Psychiatry 151 (1994): 1430-36; A. Madsen, “Neuroleptics in progressive structural brain abnormalities in psychiatric illness,” Lancet 352 (1998): 784-85; R. Gur, “A follow-up of magnetic resonance imaging study of schizophrenia,” Archives of General Psychiatry 55 (1998): 145-52. fn 51
Then, in 1998, Raquel Gur at the University of Pennsylvania Medical Center reported that the swelling of the basal ganglia and thalamus was “associated with greater severity of both negative and positive symptoms.” H. Wisniewski, “Neiirofibrillary pathology in brains of elderly schizophrenics treated with neuroleptics,” Alzheimer Disease and Associated Disorders 8 (1994): 211-27. fn 52
This last study provided a very clear picture of an iatrogenic process. The antipsychotic causes a change in brain volumes, and as this occurs, the patient becomes more psychotic (known as the “positive symptoms” of schizophrenia) and more emotionally disengaged (“negative symptoms”). The MRI studies showed that antipsychotics worsen the very symptoms they are supposed to treat, and that this worsening begins to occur during the first three years that patients are on the drugs.
In 2005, Philip Seeman reported that all of these psychotic triggers cause an increase in D2 receptors in the brain that have a “HIGH affinity” for dopamine, and by that, he meant that the receptors bound quite easily with the neurotransmitter. These “results imply that there may be many pathways to psychosis, including multiple gene mutations, drug abuse, or brain injury, all of which may converge via D2 HIGH to elicit psychotic symptoms,” he wrote.” P. Seeman, “Dopamine supersensitivity correlates with D2 HIGH states, implying many paths to psychosis,” Proceedings of the National Academy of Science 102 (2005): 3513-18. fn 53
Seeman reasoned that this is why antipsychotics work: They block D2 receptors. But in his research, he also found that these drugs, including the newer ones like Zyprexa and Risperdal, double the density of “high affinity” D2 receptors. They induce the same abnormality that angel dust does, and thus this research confirms what Lars Martensson observed in 1984: Taking a neuroleptic is like having a “psychosis inducing agent built into the brain.”
But other researchers conducting MRI studies had found that the shrinkage of the frontal lobes was drug-related, and in a 2008 interview with the New York Times, Andreasen conceded that the “more drugs you've been given, the more brain tissue you lose.” The shrinkage of the frontal lobes may be part of a disease process, which the drugs then exacerbate. “What exactly do these drugs do?” Andreasen said. “They block basal ganglia activity. The prefrontal cortex doesn't get the input it needs and is being shut down by drugs. That reduces the psychotic symptoms. It also causes the prefrontal cortex to slowly atrophy.” C. Dreifus, “Using imaging to look at changes in the brain,” New York Times,
September 16,2008. fn 56
Once again, Andreasen's investigations revealed an iatrogenic process at work. The drugs block dopamine activity in the brain and this leads to brain shrinkage, which in turn correlates with a worsening of negative symptoms and cognitive impairment.
“In the short term, acute D2 [receptor] blockade detaches salience and the patient's investment in positive symptoms. In the long term, chronic D2 blockade dampens salience for all events in everyday life, inducing a chemical anhedonia that is sometimes labeled postpsychotic depression or neuroleptic dysphoria. . . . Do we free patients from the asylum with D2 blocking agents only to block incentive, engagement with the world, and the joie de vivre of everyday life? Medication can be lifesaving in a crisis, but it may render the patient more psychosis-prone should it be stopped and more deficit-ridden should it be maintained.” T. McGlashan, “Rationale and parameters for medication-free research in psy-chosis,” Schizophrenia Bulletin 32 (2006): 300-302. fn 57
I attended the 2008 meeting of the American Psychiatric Association for a number of reasons, but the person I most wanted to hear speak was Martin Harrow, who is a psychologist at the University of Illinois College of Medicine. From 1975 to 1983, he enrolled sixty-four young schizophrenics in a long-term study funded by the NIMH, recruiting the patients from two Chicago hospitals. One was private and the other public, as this ensured that the group would be economically diverse. .” (Anatomy of an Epidemic, Robert Whitaker p115
Here is Harrow's data. In 2007, he published a report on the patients' fifteen-year outcomes in the Journal of Nervous and Mental Disease, and he further updated that review in his presentation at the APA's 2008 meeting. M. Harrow, “Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications,” Journal of Nervous and Mental Disease 195 fn 58
Source: Harrow, M. “Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications!' The Journal of Nervous and Mental Disease, 195 (2007): 406-14.
Journal of Nervous & Mental Disease:
May 2007 - Volume 195 - Issue 5 - pp 406-414
doi: 10.1097/01.nmd.0000253783.32338.6e
Original Article
In 1977, researchers discovered that benzodiazepines affect a neurotransmitter in the brain known as GABA. Unlike dopamine and serotonin, which transmit an “excitatory” message telling a neuron to fire, GABA (gamma-aminobutyric acid) inhibits neuronal activity. A neuron receiving the GABA message either fires at a slower rate or stops firing for a period of time. A majority of neurons in the brain have GABA receptors, which means that this neurotransmitter acts as the brain's brake on neuronal activity. A benzodiazepine binds to the GABA receptor and, in so doing, amplifies GABA's inhibitory effects. It pushes down on the GABA brake, so to speak, and as a result, it suppresses central nervous system activity. In response, the brain decreases its output of GABA and decreases the density of its GABA receptors. It is trying to “restore normal GABA transmission,” British scientists explained in 1982. P. Cowen, “Abstinence symptoms after withdrawal of tranquillising drugs,” Lancet 2, 8294 (1982): 360-62. fn 32
However, as a result of these adaptive changes, the brain's braking system is now in a physiologically impaired state. Its braking fluid is low (GABA output), and its brake pads are worn (GABA receptors). As a result, when the benzodiazepine is withdrawn, the brain is no longer able to properly inhibit neuronal activity, and its neurons may begin firing at a helter-skelter pace. This overactivity, Heather Ashton concluded, may “account for many of the effects of withdrawal.” H. Ashton, “Benzodiazepine withdrawal,” British Medical Journal 288 (1984): 1135-40.fn 33
The anxiety, the insomnia, the sensation of insects crawling across the skin, the paranoia, the derealization, the seizures—all of these vexing symptoms may arise from neuronal hyperactivity. .” (Anatomy of an Epidemic, Robert Whitaker p135
David Knott, a physician at the University of Tennessee, to warn in 1976 that “I am very convinced that Valium, Librium and other drugs of that class cause damage to the brain. I have seen damage to the cerebral cortex that I believe is due to the use of these drugs, and I am beginning to wonder if the damage is permanent.” Hughes, The Tranquilizing of America, 17.fn 41, p137
Over the next twenty-five years, reports of cognitive impairment in long-term benzodiazepine users regularly appeared in scientific journals. These studies told of people who were having trouble focusing, remembering things, learning new material, and solving problems. However, the patients “are not aware of their reduced ability,” Lader wrote, evidence that their self-insight was impaired as well. S. Golombok, “Cognitive impairment in long-term benzodiazepine users,” Psycho-logical Medicine 18 (1988): 365-74.fn 42, p137
In 2004, a group of Australian scientists, after reviewing the relevant literature, concluded that “long-term benzodiazepine users were consistently more impaired than controls across all cognitive categories,” with these deficits “moderate to large” in magnitude. The studies showed the “higher the intake, dose and period of use [of a benzodiazepine], the greater the risk of impairment.” M. Barker, “Cognitive effects of long-term benzodiazepine use,” CNS Drugs 18 (2004): 37-48.fn 43, p137
Increased anxiety, increased depression, and cognitive impairment—all of these factors contribute to a decline in a person's ability to function in society.
In 1983, the World Health Organization noted a “striking deterioration in personal care and social interactions” in long-term benzodiazepine users.” WHO Review Group, “Use and abuse of benzodiazepines,” Bulletin of the World Health Organization 61 (1983): 551-62. fn 44
In a study funded by Hoffmann-La Roche, the manufacturer of Valium, University of Michigan investigators determined that taking this drug was “associated with poor quality of life, poor performance in work and personal life, low social support, perceived lack of internal control, poor perceived health and high levels of stress.” R. Caplan, “Social effects of diazepam use,” Social Science & Medicine 21 (1985): 887-98. fn 46
Ashton determined that long-term use led to “malaise, ill-health, and elevated scores for neuroticism.” H. Ashton, “Tranquillisers,” British Journal of Addiction 84 (1989): 541-46.fn 47
Benzodiazepines, she said, contribute to “job loss, unemployment, and loss of work through illness.” Ashton, Benzodiazepines, 12. fn 48
To test this hypothesis, investigators conducted at least seven studies in which they compared a tricyclic to an “active” placebo, rather than an inert one. (An active placebo is a chemical that produces an unpleasant side effect of some kind, like dry mouth.) In six of the seven, there was no difference in outcomes. R. Thomson, “Side effects and placebo amplification,” British Journal of Psychiatry 140 (1982): 64-68. fn 21, p 154
A group of European psychiatrists affiliated with the World Health Organization conducted their own review of Paxil's clinical data and concluded that “among adults with moderate to severe major depression,” this popular SSRI “was not superior to placebo in terms of overall treatment effectiveness and acceptability.” C. Barbui, “Effectiveness of paroxetine in the treatment of acute major depression in adults,” Canadian Medical Association Journal 178 (2008): 296-305. fn 27, p 156
But then the NIH funded a second trial of Saint-John's-wort that had a design that complicated matters for any researcher who wanted to play favorites. It compared Saint-John's-wort to both Zoloft and a placebo. Since the herb causes side effects, such as dry mouth, it would act at the very least as an active placebo. As such, this truly was a blinded trial, the psychiatrists unable to rely on side effects as a clue to which patients were getting what, and here were the results: Twenty-four percent of the patients treated with Saint John's-wort had a “full response,” 25 percent of the Zoloft patients, and 32 percent of the placebo group. “This study fails to support the efficacy of H perforatum in moderately severe depression,” the investigators concluded, glossing over the fact that their drug had failed this test too. Hypericum Trial Study Group, “Effect of Hypericum perforatum in major depressive disorder,” Journal of the American Medical Association 287 (2002): 1807-14. fn 29, p156
“Within the field of psychopharmacology, practitioners have been cautious, if not fearful, of opening a debate on whether the treatment is more damaging [than helpful]. . . . I wonder if the time has come for debating and initiating research into the likelihood that psychotropic drugs actually worsen, at least in some cases, the progression of the illness which they are supposed to treat.” G. Fava, “Do antidepressant and antianxiety drugs increase chronicity in affective disorders?” Psychotherapy and Psychosomatics 61 (1994): 125-31. fn 38 (1994 that an Italian psychiatrist, Giovanni Fava, from the University of Bologna, 1994 editorial in Psychotherapy and Psychosomatics)
“processes that oppose the initial acute effects of a drug. . . . When drug treatment ends, these processes may operate unopposed, resulting in appearance of withdrawal symptoms and increased vulnerability to relapse,” he wrote. G. Fava, “Can long-term treatment with antidepressant drugs worsen the course of depression?” Journal of Clinical Psychiatry 64 (2003): 123-33. fn 39
Moreover, Fava noted, pointing to Baldessarini's findings, it was evident that the longer one stayed on antidepressants, the worse the problem. “Whether one treats a depressed patient for three months, or three years, it does not matter when one stops the drugs. A statistical trend suggested that the longer the drug treatment, the higher the likelihood of relapse.” G. Fava, “Can long-term treatment with antidepressant drugs worsen the course of depression?” Journal of Clinical Psychiatry 64 (2003): 123-33. fn 40
“Antidepressant drugs in depression might be beneficial in the short term, but worsen the progression of the disease in the long term, by increasing the biochemical vulnerability to depression. . . . Use of antidepressant drugs may propel the illness to a more malignant and treatment unresponsive course.” G. Fava, “Holding on: depression, sensitization by antidepressant drugs, and the prodigal experts,” Psychotherapy and Psychosomatics 64 (1995): 57-61; G. Fava, “Potential sensitizing effects of antidepressant drugs on depression,” CNS Drugs 12 fn 41
Three physicians from the University of Louisville School of Medicine echoed the sentiment. “Long-term antidepressant use may be depressogenic,” they wrote, in a 1998 letter to the Journal of Clinical Psychiatry. “It is possible that antidepressant agents modify the hardwiring of neuronal synapses [which] not only render antidepressants ineffective but also induce a resident, refractory depressive state.” R. EI-Mallakh, “Can long-term antidepressant use be depressogenic?” Journal of Clinical Psychiatry 60 (1999): 263. fn 43
One-Year Outcomes in WHO Screening Study for Depression
The WHO investigators reported that a higher percentage of the unmedicated group recovered, and that”continuing depression”was highest in those treated with an antidepressant. Source: Goldberg, D. “The effects of detection and treatment of major depression in primary care.”British Journal of General Practice 48 (1998): 1840-44.
The Risk of Disability for Depressed Patients
This was a study of 1,281 employees in Canada who went on short-term disability due to depression. Those who took an antidepressant were more than twice as likely to go on to longterm disability. Source: Dewa, C. “Pattern of antidepressant use and duration of depression-related absence from work:' British Journal of Psychiatry 183 (2003): 507-13.
NIMH's Study of Untreated Depression
In this study, the NIMH investigated the naturalistic outcomes of people diagnosed with major depression who got treatment and those who did not. At the end of six years, the treated patients were much more likely to have stopped functioning in their usual societal roles and to have become incapacitated. Source: Coryell, W.”Characteristics and significance of untreated major depressive disorder.” American Journal of Psychiatry 152 (1995): 1124-29.
There is one final study we need to review. In 2006, Michael Posternak, a psychiatrist at Brown University, confessed that “unfortunately, we have little direct knowledge regarding the untreated course of major depression.” The poor long-term outcomes detailed in APA textbooks and the NIMH studies told the story of medicated depression, which might be a very different beast. To study what untreated depression might be like in modern times, Posternak and his collaborators identified eighty-four patients enrolled in the NIMH's Psychobiology of Depression program who, after recovering from an initial bout of depression, subsequently relapsed but did not then go back on medication. Although these patients were not a “never-exposed” group, Posternak could still track their “untreated” recovery from this second episode of depression. Here were the results: Twenty-three percent recovered in one month, 67 percent in six months, and 85 percent within a year. Kraepelin, Posternak noted, had said that untreated depressive episodes usually cleared up within six to eight months, and these results provided “perhaps the most methodologically rigorous confirmation of this estimate.” M. Posternak, “The naturalistic course of unipolar major depression in the absence of somatic therapy,” Journal of Nervous and Mental Disease 194 (2006): 324-49. fn 65
“The number of episodes, and it's a very rich literature [documenting this], is associated with more cognitive deficits,” he said. “We are building more episodes, more treatment resistance, more cognitive dysfunction, and there is data showing that if you have four depressive episodes, unipolar or bipolar, it doubles your late-risk of dementia. And guess what? That isn't even the half of . . . In the United States, people with depression, bipolar, and schizophrenia are losing twelve to twenty years in life expectancy impared to people not in the mental health system.” (Antidepressants in Bipolar Disorder: Do antidepressants worsen the long-term course of bipolar disorder?, Fredrick Goodwin, 2008 APA annual meeting)
outcomes literature for this disorder, we need to try to understand this astonishing increase in its prevalence. NIMH, The Numbers Count: Mental Disorders in America, accessed at www.nimh.nih.gov on 3/7/2008. fn 9
This is data that tells of a process that routinely manufactures bipolar patients. “If you create iatrogenically a bipolar patient,” explained Fred Goodwin, in a 2005 interview in Primary Psychiatry, “that patient is likely to have recurrences of bipolar illness even if the offending antidepressant is discontinued. The evidence shows that once a patient has had a manic episode, he or she is more likely to have another one, even without the antidepressant stimulation.” Interview with Fred Goodwin, “Advances in the diagnosis and treatment of bipolar disorder,” Primary Psychiatry, accessed via Internet on 3/6/09 at primarypsychiatry.com.
fn 20, p181
Italy's Giovanni Fava put it this way: “Antidepressant-induced mania is not simply a temporary and fully reversible phenomenon, but may trigger complex biochemical mechanisms of illness deterioration.” G. Fava, “Can long-term treatment with antidepressant drugs worsen the course of depression?” Journal of Clinical Psychiatry 64 (2003): 123-33.
fn 21, p181
“With illegal and legal drugs greasing the road to bipolar illness, it is little wonder that a rare disorder in 1955 has become commonplace today. SSRIs took the country by storm in the 1990s, and from 1996 to 2004, the number of adults diagnosed with bipolar illness rose 56 percent. At the same time, psychiatry's steady expansion of diagnostic boundaries over the past thirty-five years has helped fuel the bipolar boom too. .” (Anatomy of an Epidemic, Robert Whitaker, p 181
As Moncrieff wrote in 1997, summing up lithium's record of efficacy: “There are indications that it is ineffective in the long-term outlook of bipolar disorders, and it is known to be associated with various forms of harm.” J. Moncrieff, “Lithium: evidence reconsidered,” British Journal of Psychiatry 171 (1997): 113-19. fn 37
In a 2000 paper published in the Psychiatric Quarterly, a Harvard Medical School psychiatrist, Carlos Zarate, and a psychiatrist who worked for Eli Lilly, Mauricio Tohen, opened up a new line of concern: Bipolar patients today aren't just much more symptomatic than in the past, they also don't function as well. “In the era prior to pharmacotherapy, poor outcome in mania was considered a relatively rare occurrence,” Zarate and Tohen wrote. “However, modern outcome studies have found that a majority of bipolar patients evidence high rates of functional impairment.” What, they wondered, could explain “these differences”? C. Zarate, “Functional impairment and cognition in bipolar disorder,” Psychiatric Quarterly 71 (2000): 309-29. fn 53, p188
“the more medications the patients received, the greater the psychosocial functioning impairment.” V. Balanza-Martinez, “Persistent cognitive dysfunctions in bipolar I disorder and schizophrenic patients,” Psychotherapy and Psychosomatics 74 (2005): 113-19; A Martinez-Aran, “Functional outcome in bipolar disorder,” Bipolar Disorders 9 (2007): 103-13. fn 62, p190
Finally, English researchers who looked at the daily lives of bipolar patients found that more than two-thirds “rarely or never engaged in social activities with friends,” their social lives nearly as impoverished as those diagnosed with schizophrenia. M. Pope, “Determinants of social functioning in bipolar disorder,” Bipolar Disor-
ders 9 (2007): 38-44. fn 63, p191
Finally, Kupfer threw one more concern into the mix. He detailed all the physical illnesses that now struck bipolar patients—cardiovascular problems, diabetes, obesity, thyroid dysfunction, etc.—and wondered whether “treatment factors such as toxicity from medications” could be causing these devastating ailments, or at least contributing to them. D. Kupfer, “The increasing medical burden in bipolar disorder,” Journal of the American Medical Association 293 (2005): 2528-30. fn 66
“Today, bipolar illness is a far cry from what it once was. Prior to the psychopharmacology era, it had been a rare disorder, affecting perhaps one in ten thousand people. Now it affects one in forty (or by some counts, one in twenty). And even though most patients today—at initial diagnosis—are not nearly as ill as the hospitalized patients of the past, their long-term outcomes are almost incomprehensibly worse. .” (Anatomy of an Epidemic, Robert Whitaker, p192 (good summary statement for book)
The Transformation of Bipolar Disorder in the Modern Era
|
|
Pre-Lithium Bipolar - |
. Medicated Bipolar.Today |
|
Prevalence |
1 in 5,000 to 20,000 |
1 in 20 to 50 |
|
Good long-term functional outcomes |
75% to 90% |
33% |
|
Symptom course |
Time-limited acute episodes of mania and major depression with recovery to euthymia and a fav- orable functional adaptation between episodes |
Slow or incomplete recovery from acute episodes, con-tinued risk of recurrences, and sustained morbidity over time |
|
Cognitive function |
No impairment between epiT sodes or long-term impairment |
Impairment even between episodes; long-term impairment in many cognitive domains; impairment is similar to what is observed in medicated schizophrenia |
This information is drawn from multiple sources. See in particular Huxley, N.”Disability and its treatment in bipolar disorder patients.” Bipolar Disorders 9 (2007): 183-96.
15-Year Outcomes for Schizophrenia and Manic-Depressive Patients
In this graphic, the group labeled “manic depressive” consisted of psychotic patients with bipolar illness, unipolar depression, and milder psychotic disorders. Source: Harrow, M.”Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications!' The Journal of Nervous and Mental Disease, 195 (2007): 406-14.
In 1994, seeking relief from the mood swings that plagued him, he [Steve Lappen] began taking psychiatric medications regularly. He cycled through an endless number of antidepressants and mood stabilizers, none of which worked for long. Those drug failures led to fourteen electroshock treatments, which in turn left his memory so impaired that when he returned to his job as a financial planner, “I could no longer recognize my best client. .” (Anatomy of an Epidemic, Robert Whitaker, p199
“The next five years passed pretty much as his psychiatrists had predicted. Although Greg entered Worcester Polytechnic Institute (WPI) in Massachusetts, he was so heavily medicated that, he says, “I was living in a haze most of the time. Your mind is just a bag of sand. And so I did really poorly in school. I rarely even left my room, and I was kind of out of touch with reality.” … He [Greg] went for a medical checkup, thinking this would be a first step toward reducing his medications, only to be informed that he needed to stop taking Depakote and Geodon right away, as his liver was shutting down. The abrupt withdrawal induced such physical pain—”sweats, joint and muscle pain, nausea, dizziness,” he says—that he didn't even pay attention to whether his paranoia was coming back. But in very short order, he was off all of his psychiatric drugs, except for occasional use of a stimulant, and he had also stopped smoking marijuana. “Honestly, it felt like I was waking up for the first time in five years,” he says. “It felt like I had been turned off all those years and had just been rolling through life and I was being pushed around in a wheelchair and finally I had woken up and had gotten back to being myself again. I felt like the drugs took away everything that was me, and then when I went off the drugs, my brain woke up and started working again. .” (Anatomy of an Epidemic, Robert Whitaker, p 202
“With psychiatric medications, you solve one
problem for a period of time, but the next thing you
know you end up with two problems. The treatment
turns a period of crisis into a chronic mental illness.”
-AMY UPHAM (2009 fn 1) Paraphrase it and use this quote without refererncing it
Prior to 1955, history tells us, the state mental hospitals Were bulging with raving lunatics. But then researchers discovered an antipsychotic medication, Thorazine, and that drug made it possible for the states to close their decrepit hospitals and to treat schizophrenics in the community. Next, psychiatric researchers discovered anti-anxiety agents, antidepressants, and a magic bullet—lithium--for bipolar disorder. Science then proved that the drugs worked: In clinical trials, the drugs were found to ameliorate a target symptom over the short term better than placebo. Finally, psychiatrists regularly saw that their drugs were effective. They gave them to their distressed patients, and their symptoms often abated. If their patients stopped taking the drugs, their symptoms frequently returned. This clinical course—initial symptom reduction and relapse upon drug withdrawal—also gave patients reason to say: “I need my medication. I can't do well without it.” (Anatomy of an Epidemic, Robert Whitaker, p 206
Just for a moment, before we examine whether we have solved the puzzle that we set forth in the opening of this book, here is a quick way to see the old-hag picture a bit more clearly. Imagine that a virus suddenly appears in our society that makes people sleep twelve, fourteen hours a day. Those infected with it move about somewhat slowly and seem emotionally disengaged. Many gain huge amounts of weight—twenty, forty, sixty, and even one hundred pounds. Often, their blood sugar levels soar, and so do their cholesterol levels. A number of those struck by the mysterious illness—including young children and teenagers—become diabetic in fairly short order. Reports of patients occasionally dying from pancreatitis appear in the medical literature. Newspapers and magazines fill their pages with accounts of this new scourge, which is dubbed metabolic dysfunction illness, and parents are in a panic over the thought that their children might contract this horrible disease. The federal government gives hundreds of millions of dollars to scientists at the best universities to decipher the inner workings of this virus, and they report that the reason it causes such global dysfunction is that it blocks a multitude of neurotransmitter receptors in the brain—dopaminergic, serotoninergic, muscarinic, adrenergic, and histaminergic. All of those neuronal pathways in the brain are compromised. Meanwhile, MRI studies find that over a period of several years, the virus shrinks the cerebral cortex, and this shrinkage is tied to cognitive decline. A terrified public clamors for a cure. Now such an illness has in fact hit millions of American children and adults. We have just described the effects of Eli Lilly's bestselling antipsychotic, Zyprexa. .” (Anatomy of an Epidemic, Robert Whitaker, p208
Entitlement trap, expanding diagnostic boundaries, drugs cause debilitation
More than 1.5 million people are on SSI or SSDI because they are disabled by anxiety, depression, or bipolar illness, and, according to the Johns Hopkins data, more than 14 million people who have these diagnoses are “severely impaired” in their ability to function in society. That is the astonishing bottom-line result produced by a medical specialty that has dramatically expanded diagnostic boundaries in the past fifty years and treated its patients with drugs that perturb normal brain function. .” (Anatomy of an Epidemic, Robert Whitaker, p 210
Although the public often hears that research has shown that ADHD is a “brain disease,” the truth is that its etiology remains unknown. “Attempts to define a biological basis for ADHD have been consistently unsuccessful,” wrote pediatric neurologist Gerald Golden in 1991. “The neuroanatomy of the brain, as demonstrated by imaging studies, is normal. No neuropathologic substrate has been demonstrated.” G. Golden, “Role of attention deficit hyperactivity disorder in learning disabilities,” Seminars in Neurology 11 (1991): 35-41. fn 9 p 220
“After years of clinical research and experience with ADHD, our knowledge about the cause or causes of ADHD remains largely speculative.” NIH Consensus Development Conference statement, “Diagnosis and treatment of attention deficit hyperactivity disorder,” November 16-18,1998. fn 10
American Psychiatric Press's 1997 Textbook of Neuropsychiatry confessed, “efforts to identify a selective neurochemical imbalance [in ADHD children] have been disappointing.” P. Breggin, Talking Back to Ritalin (Cambridge, MA: Perseus Publishing, 2001), 180. fn 11
The child's brain is now operating, as Steven Hyman said, in a manner that is “qualitatively as well as quantitatively different from the normal state.” S. Hyman, “Initiation and adaptation: a paradigm for understanding psychotropic drug action,” American Journal of Psychiatry 153 (1996): 151-61. fn 12
“Children who were retrospectively confirmed to have been on active drug treatment appeared, at the times of evaluation, distinctly more bland or “flat” emotionally, lacking both the age-typical variety and frequency of emotional expression. They responded less, exhibited little or no initiative or spontaneity, offered little indication of either interest or aversion, showed virtually no curiosity, surprise, or pleasure, and seemed devoid of humor. Jocular comments and humorous situations passed unnoticed. In short, while on active drug treatment, the children were relatively but unmistakably affectless, humorless, and apathetic. H. Rie, “Effects of methylphenidate on underachieving children,” Journal of Con-sulting and Clinical Psychology 44 (1976): 250-60. fn 14 (. In a 1978 double-blind study, Ohio State University psychologist Herbert Rie studied twenty-eight “hyperactive” children for three months, half of whom were prescribed methylphenidate.)
Children on Ritalin show “a marked drug-related increase in solitary play and a corresponding reduction in their initiation of social interactions,” announced Russell Barkley, a psychologist at the Medical College of Wisconsin, in 1978. C. Cunningham, “The effects of methylphenidate on the mother-child interactions of hyperactive identical twins,” Developmental Medicine & Child Neurology 20 (1978): 634-42.fn 15
This drug, observed Bowling Green State University psychologist Nancy Fiedler, reduced a child's “curiosity about the environment.” N. Fiedler, “The effects of stimulant drugs on curiosity behaviors of hyperactive boys,” Journal of Abnormal Child Psychology 11 (1983): 193-206fn 16
At times, the medicated child “loses his sparkle,” wrote Canadian pediatrician Till Davy in 1989. T. Davy, “Stimulant medication and short attention span,” Journal of Developmental & Behavioral Pediatrics 10 (1989): 313-18.fn 17
Children treated with a stimulant, concluded a team of UCLA psychologists in 1993, often become “passive, submissive” and “socially withdrawn.” D. Granger, “Perceptions of methylphenidate effects on hyperactive children's peer interactions,” Journal of Abnormal Child Psychology 21 (1993): 535-49.fn 18
Some children on the drug “seem zombie-like,” noted psychologist James Swanson, director of an ADHD center at the University of California, Irvine. J. Swanson, “Effects of stimulant medication on learning in children with ADHD,” Journal of Learning Disabilities 24 (1991): 219-30.fn 19
However, none of this tells of drug treatment that benefits the child. Stimulants work for the teacher, but do they help the child?
“we found a pervasive dislike among hyperactive children for taking stimulants. “ E. Sleator, “How do hyperactive children feel about taking stimulants and will they tell the doctor?” Clinical Pediatrics 21 (1982): 474-79. fn 23
Children on Ritalin, University of Texas psychologist Deborah Jacobvitz reported in 1990, rated themselves as “less happy and [less] pleased with themselves and more dysphoric.” When it came to helping a child make friends and sustain friendships, stimulants produced “few significant positive effects and a high incidence of negative effects,” Jacobvitz said. D. Jacobvitz, “Treatment of attentional and hyperactivity problems in children with sympathomimetic drugs,” Journal of the American Academy of Child & Adolescent Psychiatry 29 (1990): 677-88. fn 24
Five years later, Herbert Rie was much more negative. He reported that Ritalin did not produce any benefit on the students' “vocabulary, reading, spelling, or math,” and hindered their ability to solve problems. “The reactions of the children strongly suggest a reduction in commitment of the sort that would seem critical for learning.” Rie, “Effects of methylphenidate.”fn 27
That same year, Russell Barkley at the Medical College of Wisconsin reviewed the relevant scientific literature and concluded “the major effect of stimulants appears to be an improvement in classroom manageability rather than academic performance.” R. Barkley, “Do stimulant drugs improve the academic performance of hyperkinetic children?” Clinical Pediatrics 8 (1978): 137-46. fn 28
Next it was James Swanson's turn to weigh in. The fact that the drugs often left children “isolated, withdrawn and overfocused” could “impair rather than improve learning,” he said. Swanson, “Effects of stimulant medication.” fn 29
Carol Whalen, a psychologist from the University of California at Irvine, noted in 1997 that “especially worrisome has been the suggestion that the unsalutary effects [of Ritalin] occur in the realm of complex, high-order cognitive functions such as flexible problem-solving or divergent thinking.” C. Whalen, “Stimulant pharmacotherapy for attention-deficit hyperactivity disorders,” in S. Fishberg and R. Greenberg, eds., From Placebo to Panacea (New York: John Wiley & Sons, 1997), 329. fn 30
Finally, in 2002, Canadian investigators conducted a meta-analysis of the literature, reviewing fourteen studies involving 1,379 youths that had lasted at least three months, and they determined that there was “little evidence for improved academic performance.” R. Schachar, “Attention-deficit hyperactivity disorder,” Canadian Journal of Psychi-atry 47 (2002): 337-48. fn 31
Controversy has long raged over whether ADHD is a “real” disease, but this study showed that when it comes to using stimulants to treat it, the controversy is moot. Even if ADHD is real, stimulants aren't going to provide long-term help. “We had thought that children medicated longer would have better outcomes. That didn't happen to be the case,” said William Pelham from the State University of New York at Buffalo, who was one of the principal investigators. “There were no beneficial effects, none. In the short term, [medication] will help the child behave better, in the long run it won't. And that information should be made very clear to parents.” C. Miranda, “ADHD drugs could stunt growth,” Daily Telegraph (UK), November 12,2007. fn 41
Ritalin and the other ADHD medications cause a long list of physical, emotional, and psychiatric adverse effects. The physical problems include drowsiness, appetite loss, lethargy, insomnia, headaches, abdominal pain, motor abnormalities, facial and vocal tics, jaw clenching, skin problems, liver disorders, weight loss, growth suppression, hypertension, and sudden cardiac death. The emotional difficulties include depression, apathy, a general dullness, mood swings, crying jags, irritability, anxiety, and a sense of hostility toward the world. The psychiatric problems include obsessive-compulsive symptoms, mania, paranoia, psychotic episodes, and hallucinations. Methylphenidate also reduces blood flow and glucose metabolism in the brain, changes that usually are associated with “neuropathologic states.” Breggin, Talking Back to Ritalin; K. Bolla, “The neuropsychiatry of chronic cocaine abuse,” Journal of Neuropsychiatry and Clinical Neurosciences 10 (1998): 280-89. fn 42 p 228
In the absence of any efficacy benefit, we are now left with the unhappy task of tallying up the harm done by the prescribing of antidepressants to children and teenagers. We can start with the physical problems. SSRIs may cause insomnia, sexual dysfunction, headaches, gastrointestinal problems, dizziness, tremors, nervousness, muscle cramps, muscle weakness, seizures, and a severe inner agitation known as akathisia, which is associated with an increased risk of violence and suicide. The psychiatric problems they can trigger are even more problematic. … Other physicians have told of their SSRI-treated younger patients suffering panic attacks, anxiety, nervousness, and hallucinations.” (Anatomy of an Epidemic, Robert Whitaker, p 231
American Psychiatric Association warns in one of its textbooks—an “apathy syndrome,” which “is characterized by a loss of motivation, increased passivity, and often feelings of lethargy and 'flatness.' “P. Breggin, Brain-Disabling Treatments in Psychiatry (New York: Springer Publishing Company, 2008), 153. fn 57
Although this risk isn't well quantified, Canadian psychiatrists reported in 1999 that nine of ninety-six ADHD children they treated with stimulants for an average of twenty-one months developed “psychotic symptoms.” E. Cherland, "Psychotic side effects of psychostimulants," Canadian Journal of Psychiatry 44 (1999): 811-13. fn 72
The ADHD to Bipolar Pathway
|
Stimulant-drug Induced effects |
Bipolar Diagnotic Symptoms |
||
|
Arousal |
Dysphoric |
Arousal |
Dysphoric |
|
Increased energy Intensified focus Hyperalertness Euphoria Agitation, anxiety Insomnia Irritability Hostility Hypomania Mania Psychosis |
Somnolence Fatigue, lethargy Social withdrawal, isolation Decreased spontaneity Reduced curiosity Constriction of affect Depression Emotional lability |
Increased energy Intensified goal- Decreased need for sleep Severe mood change Irritability Agitation Destructive outbursts Increased talking Distractibility Hypomania Mania |
Sad mood Loss of energy Loss of interest in activities Social isolation Poor comnnuni- cation Feelings of worth- lessness Unexplained crying |
Stimulants used to treat ADHD induce both arousal and dysphoric symptoms. These drug-induced symptoms overlap to a remarkable degree the symptoms said to be characteristic of juvenile bipolar disorder.
In short, every child on a stimulant turns a bit bipolar, and the risk that a child diagnosed with ADHD will move on to a bipolar diagnosis after being treated with a stimulant has even been quantified. Joseph Biederman and his colleagues at Massachusetts General Hospital reported in 1996 that 15 of 140 children (11 percent) diagnosed with ADHD developed bipolar symptoms—which were not present at initial diagnosis—within four years. J. Biederman, "Attention-deficit hyperactivity disorder and juvenile mania," Journal of the American Academy of Child & Adolescent Psychiatry 35 (1996): 997-1008. fn 76 This gives us our first mathematical equation for solving the juvenile bipolar epidemic: If a society prescribes stimulants to 3.5 million children and adolescents, as is the case in the United States today, it should expect that this practice will create 400,000 bipolar youth. .” (Anatomy of an Epidemic, Robert Whitaker p 238
In 1995, Harvard psychiatrists determined that 25 percent of children and adolescents diagnosed with depression convert to bipolar illness within two to four years. “Antidepressant treatment may well induce switching into mania, rapid cycling or affective instability in the young, as it almost certainly does in adults,” they explained.” Washington University's Barbara Geller extended the follow-up period to ten years, and in her study, nearly half of prepubertal children treated for depression ended up bipolar. B. Geller, "Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder," American Journal of Psychiatry 158 (2001): 125-27. fn 82 These findings give us our second mathematical equation for solving the bipolar epidemic: If 2 million children and adolescents are treated with SSRIs for depression, this practice will create 500,000 to 1 million bipolar youth. We now have numbers that tell of an iatrogenic epidemic: 400,000 bipolar children arriving via the ADHD doorway, and at least another half million through the antidepressant doorway. There is also a way that we can double-check that conclusion: When investigators survey juvenile bipolar patients, do they find that most traveled down one of those two iatrogenic paths? ” (Anatomy of an Epidemic, Robert Whitaker p 239
3 charts page 241
In particular, atypical antipsychotics may cause metabolic dysfunction, hormonal abnormalities, diabetes, obesity, emotional blunting, and tardive dyskinesia. Eventually, the drugs will induce cognitive decline, and the child who stays on the cocktails into adulthood can expect to die early as well. That is the long-term course of this iatrogenic illness: A child who may be hyperactive or depressed is treated with a drug that triggers a manic episode or some degree of emotional instability, and then the child is put on a drug cocktail that leads to a lifetime of disability. .” (Anatomy of an Epidemic, Robert Whitaker, p 244
chart page 246
Zyprexa could cause weight gain, hypoglycemia, and diabetes.
“Today, her ambivalence about the medications is such that she wishes she could turn back the clock and try a different tack. “My Andrew is not a circle or a square, he is not even a triangle,” she explains. “He is a rhombus trapezoid, and he will never fit into those other molds. And I do think that if we had never put him on medicine, he would have learned many more coping mechanisms, because he would have had to. And we should be able to help kids like Andrew without making them feel so different, without suppressing their appetite, and without worrying about the long-term effects of the drugs—all the things I am sitting here worrying about. .” (Anatomy of an Epidemic, Robert Whitaker, quoting Andrew Steven’s mother, p 251
“If You're a Ward of the State, You Must Be Bipolar: The medicating of foster children in the United States took off in the late 1990s, and so I thought, in order to gain a perspective on this phenomenon, I would visit with Theresa Gately. She and her husband, Bill, took ninety-six foster children into their Boston home from 1996 to 2000, and thus she personally witnessed this change in how our society treats foster kids. The first children that Social Services sent them weren't medicated, but by the end, “it felt like all of them were on psych drugs,” she says.”” (Anatomy of an Epidemic, Robert Whitaker, p 253
“It was not surprising that medical students accepted
the dogma of biomedical reductionism in psychiatry
uncritically; they had no time to read and analyze the
original literature. What took me a while to understand,
as I moved through my residency, was that psychiatrists
rarely do the critical reading either.”
-COLIN ROSS, CLINICAL ASSOCIATE PROFESSOR OF
PSYCHIATRY AT SOUTHWEST MEDICAL CENTER IN
DALLAS, TEXAS (1995) C. Ross, Pseudoscience in Psychiatry (New York: John Wiley & Sons, 1995).
The first problem that had arisen for psychiatry was an intellectual challenge to its legitimacy, an attack launched in 1961 by Thomas Szasz, a psychiatrist at the State University of New York in Syracuse. In his book The Myth of Mental Illness, he argued that psychiatric disorders weren't medical in kind, but rather labels applied to people who struggled with “problems in living” or simply behaved in socially deviant ways. Psychiatrists, he said, had more in common with ministers and police than they did with physicians. Szasz's criticism rattled the field, since even mainstream publications like the Atlantic and Science found his argument to be both cogent and important, the latter concluding that his treatise was “enormously courageous and highly informative . . . bold and often brilliant.” See blurbs for second edition of The Myth of Mental Illness, published by Harper & Row in 1974. fn 4, p 264
But as critics at the time noted, it was difficult to understand why this manual should be regarded as a great scientific achievement. No scientific discoveries had led to this reconfiguring of psychiatric diagnoses. The biology of mental disorders remained unknown, and the authors of DSM-III even confessed that this was so. Most of the diagnoses, they said, “have not yet been fully validated by data about such important correlates as clinical course, outcome, family history, and treatment response.” Kirk, The Selling of DSM, 115. fn 26
It was also evident that the boundary lines between disease and no disease had been arbitrarily drawn. Why did it require the presence of five of nine symptoms said to be characteristic of depression for a diagnosis of the illness to be made? Why not six such symptoms? Or four? DSM-III, wrote Theodore Blau, president of the American Psychological Association, was more of “a political position paper for the American Psychiatric Association than a scientifically-based classification system.” M. Sabshin, "Report of the medical director" (1980), 1308. fn 27 None of that mattered, however. With the publication of DSMIII, psychiatry had publicly donned a white coat. The Freudians had been vanquished, the concept of neurosis basically tossed into the trash bin, and everyone in the profession was now expected to embrace the medical model., p 270
“Biopsychiatry” “molecular psychiatry”
Twenty-five years later, that breakthrough moment still lies in the future. The biological underpinnings of schizophrenia, depression, and bipolar disorder remain unknown. But the public has long since been convinced otherwise, and we can see now the marketing process that got this delusion under way. At the start of the 1980s, psychiatry was worried about its future. .” (Anatomy of an Epidemic, Robert Whitaker, p 275
The final group to participate in this storytelling campaign was the National Alliance for the Mentally Ill. Founded in 1979 by two Wisconsin women, Beverly Young and Harriet Shelter, it arose as a grassroots protest to Freudian theories that blamed schizophrenia on “aloof, uncaring mothers and preoccupied mothers who were unable to bond with their infants,” a NAMI historian observed. E. Foulks, "Advocating for persons who are mentally ill," Administration and Policy in Mental Health and Mental Health Services Research 27 (2000): 353-67. fn 59 NAMI was eager to embrace an ideology of a different kind, and the message it sought to spread, said former NAMI president Agnes Hatfield in 1991, was that “mental illness is not a mental health problem; it is a biological illness. There is considerable clarity on the part of families that they are focusing on a physical disease.” A. Hatfield, "The National Alliance for the Mentally Ill," Community Mental Health Journal 27 (1991): 95-103. fn 60, p 279
In short, a powerful quartet of voices came together during the 1980s eager to inform the public that mental disorders were brain diseases. Pharmaceutical companies provided the financial muscle. The APA and psychiatrists at top medical schools conferred intellectual legitimacy upon the enterprise. The NIMH put the government's stamp of approval on the story. NAMI provided a moral authority. This was a coalition that could convince American society of almost anything, and even better for the coalition, there was one other voice on the scene that, in its own way, helped make the story bulletproof in society's eyes.” (Anatomy of an Epidemic, Robert Whitaker p 280 (great summary verse for book)
At that moment, Eli Lilly and all of psychiatry had achieved a public relations victory of lasting importance. The wonder-drug aura around Prozac had been restored, and the public and the media had been conditioned to associate criticism of psychiatric drugs with Scientology. The debate over the merits of these drugs now seemed to feature the nation's top scientists and doctors on one side and religious kooks on the other, and if that were so, the public could be certain where the truth lay. ” (Anatomy of an Epidemic, Robert Whitaker, p 294
The Xanax Study
In Upjohn's study of Xanax, patients were treated with the drug or placebo for eight weeks. Then this treatment was slowly withdrawn (weeks 9 through 12), and during the last two weeks patients didn't receive any treatment.The Xanax patients fared better during the first four weeks, which is the result that the Upjohn investigators focused on in their journal articles. However, once the Xanax patients began withdrawing from the the drug, they suffered many more panic attacks than the placebo patients, and at the end of the study were much more symptomatic. Source: Ballenger, C.”Alprazolam in panic disorder and agoraphobieArchives of General Psychiatry 45 (1988): 413-22. Pecknold, C.”Alprazolam in panic disorder and agoraphobia:' Archives of General Psychiatry 45 (1988): 429-36.
Chart page 297
In London, Isaac Marks and several of his colleagues at the Institute of Psychiatry subsequently pointed out how transparently ridiculous this all was. In a letter to the Archives of General Psychiatry, they observed that since the alprazolam patients “were in a worse state than patients receiving placebo” at the end of the study, the finding by the Upjohn investigators that the drug was effective and well tolerated could only be seen as “biased and arguable.”51 The entire affair, Marks subsequently wrote, “is a classic demonstration of the hazards of research funded by industry.” I. Marks, "Reply to comment on the London/Toronto study," British Journal of Psychiatry 162 (1993): 790-94. fn 52
A study by the U.S. Department of Veterans Affairs came to a similar conclusion about the relative merits of atypicals and the older drugs, and then, in 2007, British psychiatrists reported that schizophrenia patients, if anything, had a better “quality of life” on the old drugs than on the new ones. fn 75 All of this led two prominent psychiatrists to write in the Lancet that the story of the atypicals as breakthrough medications could now be “regarded as invention only,” a tale concocted “by the drug industry for marketing purposes and only now being exposed.” Yet, they wondered, “how is it that for nearly two decades we have, as some have put it, 'been beguiled' into thinking they were superior?” P. Tyrer, "The spurious advance of antipsychotic drug therapy," Lancet 373 (2009): 4-5. fn 76, p 303
Hiding the Evidence
The third aspect to the storytelling process that has led to our societal delusion about the merits of psychiatric drugs is easy to document. Imagine what our beliefs would be today if, over the past twenty years, we had opened our newspapers and read about the following findings, which represent but a sampling of the outcome -studies we reviewed earlier in the book:
1990: In a large, national depression study, the eighteen-month stay-well rate was highest for those treated with psychotherapy (30 percent) and lowest for those treated with an antidepressant (19 percent). (NIMH)
1992: Schizophrenia outcomes are much better in poor countries like India and Nigeria, where only 16 percent of patients are regularly maintained on antipsychotics, than in the United States and other rich countries, where continual drug usage is the standard of care. (World Health Organization)
1995: In a six-year study of 547 depressed patients, those who were treated for the disorder were nearly seven times more likely to become incapacitated than those who weren't, and three times more likely to suffer a “cessation” of their “principal social role.” (NIMH)
1998: Antipsychotic drugs cause morphological changes in the brain that are associated with a worsening of schizophrenia symptoms. (University of Pennsylvania)
1998: In a World Health Organization study of the merits of screening for depression, those diagnosed and treated with psychiatric medications fared worse—in terms of their depressive symptoms and their general health—over a one-year period than those who weren't exposed to the drugs. (WHO)
1999: When long-term benzodiazepine users withdraw from the drugs, they become “more alert, more relaxed, and less anxious.” (University of Pennsylvania)
2000: Epidemiological studies show that long-term outcomes for bipolar patients today are dramatically worse than they were in the pre-drug era, with this deterioration in modern outcomes likely due to the harmful effects of antidepressants and antipsychotics. (Eli Lilly; Harvard Medical School)
2001: In a study of 1,281 Canadians who went on short-term disability for depression, 19 percent of those who took an antidepressant ended up on long-term disability, versus 9 percent of those who didn't take the medication. (Canadian investigators)
2001: In the pre-drug era, bipolar patients did not suffer cognitive decline over the long term, but today they end up almost as cognitively impaired as schizophrenia patients. (Sheppard Pratt Health System in Baltimore)
2004: Long-term benzodiazepine users suffer cognitive deficits “moderate to large” in magnitude. (Australian scientists)
2005: Angel dust, amphetamines, and other drugs that induce psychosis all increase D2 HIGH receptors in the brain; antipsychotics cause this same change in the brain. (University of Toronto)
2005: In a five-year study of 9,508 depressed patients, those who took an antidepressant were, on average, symptomatic nineteen weeks a year, versus eleven weeks for those who didn't take any medication. (University of Calgary)
2007: In a fifteen-year study, 40 percent of schizophrenia patients off antipsychotics recovered, versus 5 percent of the medicated patients. (University of Illinois)
2007: Long-term users of benzodiazepines end up “markedly ill to extremely ill” and regularly suffer from symptoms of depression and anxiety. (French scientists)
2007: In a large study of children diagnosed with ADHD, by the end of the third year “medication use was a significant marker not of beneficial outcome, but of deterioration.” The medicated children were also more likely to engage in delinquent behavior; they ended up slightly shorter, too. (NIMH)
2008: In a national study of bipolar patients, the major predictor of a poor outcome was exposure to an antidepressant. Those who took an antidepressant were nearly four times as likely to become rapid cyclers, which is associated with poor long-term outcome. (NIMH)
Finally, the entire outcomes history documented in this book is missing from the 2008 edition of the APA's Textbook of Psychiatry, which means that medical students training to be psychiatrists are kept in the dark about this history.” The book does not discuss “supersensitivity psychosis.” It does not mention that antidepressants may be depressogenic agents over the long term. It does not report that bipolar outcomes are much worse today than they were forty years ago. There is no discussion of rising disability rates. There is no talk about the cognitive impairment that is seen in longtime users of psychotropic drugs. The textbook authors are clearly familiar with many of the sixteen studies listed above, but, if they do mention them, they don't discuss the relevant facts about medication usage. The long-running study by Harrow, the textbook states, reveals that there are some schizophrenia patients who “are able to function without the benefit of continuous antipsychotic treatment.” The authors of that sentence didn't mention the stunning difference in recovery rates for the unmedicated and medicated groups; instead they crafted a sentence that told of the benefit of continuous antipsychotic treatment. In a similar vein, while the textbook briefly discusses the WHO study on the better outcomes of schizophrenia patients in poor countries like India and Nigeria, it does not mention that patients in those countries weren't regularly maintained on antipsychotics. In a section on benzodiazepines, the authors acknowledge that there are concerns about their addictive properties, but then state that long-term outcomes for those who stay on benzodiazepines are generally good, as most patients “maintain their therapeutic gains.”
There is a story that psychiatry doesn't dare tell, which shows that our societal delusion about the benefits of psychiatric drugs isn't entirely an innocent one. In order to sell our society on the soundness of this form of care, psychiatry has had to grossly exaggerate the value of its new drugs, silence critics, and keep the story of poor long-term outcomes hidden. That is a willful, conscious process, and the very fact that psychiatry has had to employ such storytelling methods reveals a great deal about the merits of this paradigm of care, much more than a single study ever could. ” (Anatomy of an Epidemic, Robert Whitaker, p 312
As we saw earlier, during the late 1970s psychiatry was worried about its survival. The public viewed its therapies as “low in efficacy,” and sales of psychiatric drugs were in decline. Then, in what might be called a “rebranding” effort, psychiatry published DSMIII and began telling the public that mental disorders were “real” diseases, just like diabetes and cancer, and that their drugs were chemical antidotes to those diseases, just like “insulin for diabetes.” That story, while it may have been false in kind, created a powerful conceptual framework for selling psychiatric medications of all types. Everyone could understand the chemical-imbalance metaphor, and once the public came to understand that notion, it became relatively simple for pharmaceutical companies and their storytelling allies to build markets for psychiatric drugs of various types. They ran “educational” campaigns to make the public more “aware” of the various disorders the drugs were approved to treat, and, at the same time, they expanded the diagnostic boundaries of mental disorders. ” (Anatomy of an Epidemic, Robert Whitaker, p 316
|
This is a medical success that has been decades in the making, and it began in 1969 when Yrjo Alanen, a Finnish psychiatrist who had psychoanalytic training, arrived at the psychiatric hospital in Turku, a port city in southwest Finland. At that time, few psychiatrists in the country thought that psychotherapy could help schizophrenics. However, Alanen believed that the hallucinations and paranoid utterances of schizophrenic patients, when carefully parsed, told meaningful stories. Hospital psychiatrists, nurses, and staff needed to listen to the patients. “It's almost impossible for anyone meeting with these patients' families to not understand that they have difficulties in life,” Alanen explained in an interview at the psychiatric hospital in Turku. They are “not ready” to be adults, and “we can help with this development.r10 Over the next fifteen years, Alanen and a handful of other Turku psychiatrists, most notably Jukka Aaltonen and Viljo Rakkolainen, created what they called the “need-adapted” treatment of psychotic patients. Since psychotic patients are a very heterogeneous group, they decided that treatment needed to be “case specific.” Some first-episode patients would need to be hospitalized, and others would not. Some would benefit from low doses of psychiatric medications (either benzos or neuroleptics), and others would not. Most important, the Turku psychiatrists settled on group family therapy—of a particularly collaborative type—as the core treatment. Psychiatrists, psychologists, nurses, and others trained in family therapy all served on two- and three-member “psychosis teams,” which would meet regularly with the patient and his or her family. Decisions about the patient's treatment were made jointly at those meetings. In those sessions, the therapists did not worry about getting the patient's psychotic symptoms to abate. Instead, they focused the conversation on the patient's past successes and achievements, with the thought that this would help strengthen his or her “grip on life.” The hope, said Rakkolainen, “is that they haven't lost the idea that they can be like others.” The patient might also receive individual 338 • ANATOMY OF AN EPIDEMIC psychotherapy to help this process along, and eventually the patient would be encouraged to construct a new “self-narrative” for going forward, the patient imagining a future where he or she was integrated into society, rather than isolated from it. “With the biological conception of psychosis, you can't see the past achievements” or the future possibilities, Aaltonen said. During the 1970s and 1980s, the outcomes for psychotic patients in the Turku system steadily improved. Many chronic patients were discharged from the hospital, and a study of first-episode schizophrenic-type patients treated from 1983 to 1984 found that 61 percent were asymptomatic at the end of five years and only 18 percent were on disability. This was a very good result, and from 1981 to 1987, Alanen coordinated the Finnish National Schizophrenia Project, which determined that the need-adapted model of care developed in Turku could be successfully introduced into other cities. Two decades after Alanen and the others had initiated their Turku project, Finland had decided that psychotherapy could indeed help psychotic patients. However, the question of the best use of antipsychotics remained, and in 1992, Finland mounted a study of first-episode patients to answer it. All six sites in the study provided the newly diagnosed patients with need-adapted treatment, but in three of the centers, the patients were not put on antipsychotics during the first three weeks (benzos could be used), with drug therapy initiated only if the patient hadn't improved during this period. At the end of two years, 43 percent of the patients from the three “experimental” sites had never been exposed to neuroleptics, and overall outcomes at the experimental sites were “somewhat better” than they were at the centers where nearly all of the patients had been exposed to the drugs. Furthermore, among the patients at the three experimental sites, those who had never been exposed to neuroleptics had the best outcomes.11 “I would advise case-specific use [of the drugs],” Itakkolainen said. “Try without antipsychotics. You can treat them better without medication. They become more interactive. They become themselves.” Added Aaltonen: “If you can postpone medication, that's important.” BLUEPRINTS FOR REFORM • 339 It might seem that Finnish psychiatry, given the outcomes of the study, would have then embraced—on a national level—this “no immediate use of neuroleptics” model of care. Instead, Alanen and the other creators of need-adapted treatment retired, and during the 1990s, Finland's treatment of psychosis became much more “biologically” oriented. Even in Turku, first-episode patients are regularly treated with antipsychotics today, and Finnish guidelines now call for the patients to be kept on the drugs for at least five years after a first episode. “I am a bit disappointed,” Alanen confessed at the end of our interview. Fortunately, one of the three “experimental” sites in the 19921993 study did take the results to heart. And that site was Tornio, in western Lapland.
|
Treated with Open-Dialogue Therapy
|
Patients (N=75) |
|
|
Schizophrenia (N=30) Other psychotic disorders (N=45) |
|
|
Antipsychotic use |
|
|
Never exposed to antipsychotics Occasional use during five years Ongoing use at end of five years |
67% |
|
Psychotic symptoms |
|
|
Never relapsed during five years Asymptomatic at five-year follow-up |
67% |
|
Functional outcomes at five years |
|
|
Working or in school Unemployed On disability |
73% 7% 20% |
Source: Seikkula, J. “Five-year experience of first-episode nonaffective psychosis in open-dialogue approach:' Psychotherapy Research 16 (2006): 214-28.
With most of the staff in the district trained in family therapy, the system is able to respond quickly to a psychotic crisis. Whoever is first contacted—by a parent, a patient seeking help, or perhaps a school administrator—is responsible for organizing a meeting within twenty-four hours, with the family and patient deciding where the meeting should be held. The patient's home is the preferred place. There must be at least two staff members present at the meeting, and preferably three, and this becomes a “team” that ideally will stay together during the patient's treatment. Everyone goes to that first meeting aware that they “know nothing,” said nurse Mia Kurtti. Their job is to promote an “open dialogue” in which everybody's thoughts can become known, with the family members (and friends) viewed as coworkers. “We are specialists in saying that we are not specialists,” Birgitta Alakare said.
The therapists consider themselves guests in the patient's home, and if an agitated patient runs off to his or her room, they simply ask the patient to leave the door open, so that he or she can listen to the conversation. “They hear voices; we meet them, and we try to reassure them,” Salo said. “They are psychotic, but they are not violent at all.” Indeed, most patients want to tell their story, and when they speak of hallucinations and paranoid thoughts, the therapists simply listen and reflect upon what they've heard. “I think [psychotic symptoms] are very interesting,” Kurtti said. “What's the difference between voices and thoughts? We are having a conversation.”
A Natural Antidepressant
In the early 1800s, Americans regularly turned to a book written by Scottish physician William Buchan for medical advice. In Domestic Medicine, Buchan prescribed this pithy remedy for melancholy:
“The patient ought to take as much exercise in the open air as he can bear ... A plan of this kind, with a strict attention to diet, is a much more rational method of cure, than confining the patient within doors, and plying him with medicines. W. Buchan, Domestic Medicine (Boston: Otis, Broaders, and Co., 1846), 307. fn 17
Today, general practitioners in the UK may write a prescription for exercise. “The evidence base for exercise as a treatment for depression is quite good,” said Andrew McCulloch, executive director of the Mental Health Foundation, a London-based charity that has been promoting this alternative. “It also reduces anxiety. It's good for self-esteem, control of obesity, et cetera. It has a broad-spectrum effect.” Interview with Andrew McCulloch in London, September 3,2009. fn 19
In terms of its short-term efficacy as an antidepressant, studies have shown that exercise produces a “substantial improvement” within six weeks, that its effect size is “large,' and that 70 percent of all depressed patients respond to an exercise program. “These success rates are quite remarkable,” German investigators wrote in 2008. F. Dimeo, "Benefits from aerobic exercise in patients with major depression," British Journal of Sports Medicine 35 (2001): 114-17; K. Knubben, "A randomized, controlled study on the effects of a short-term endurance training programme in patients with major depression," British Journal of Sports Medicine 41 (2007): 29-33; A. Strohle, "Physical activity, exercise, depression and anxiety disorders," Journal of Neural Transmission 116 (2009): 777-84. 20 In addition, over time, exercise produces a multitude of “side benefits.” It enhances cardiovascular function, increases muscle strength, lowers blood pressure, and improves cognitive function. People sleep better, they function better sexually, and they also tend to become more socially engaged.
The Long-Term Benefit of Exercise for Depression
|
Treatment During |
Percentage of Patients in Remission at End of Four Months |
Percentage of Remitted Patients Who Relapsed in Six-Month Follow-up |
Percentage of Patients Depressed at End ofTen Months |
|
Zoloft alone |
69% |
38% |
52% |
|
Zoloft plus exercise therapy |
66% |
31% |
55% |
|
Exercise therapy alone |
60% |
8% |
30% |
In this study by Duke researchers, older patients with depression were treated for 16 weeks in one of three ways, and then followed for another six months. Patients treated with exercise alone had the lowest rates of relapse during the following six months, and as a group, they were much less likely to be suffering from depressive symptoms at the end of ten months. Source: Babyak, M. “Exercise treatment for major depression “Psychosomatic Medicine 62 (2000): 633-38. 100-11.
When a child enters Seneca Center's residential program, Stanton does not ask “what's wrong” with the child, but rather “what happened to them.” He gets the department of social services, schools, and other agencies to send him all of the records they have on the child, and then he spends eight to ten hours constructing a “life chart.” As might be expected, the charts regularly tell of children who have been sexually abused, physically abused, and horribly neglected. ” (Anatomy of an Epidemic, Robert Whitaker, p 349
Having become versed in the scientific literature, the Alaska Supreme Court gave PsychRights a stunning legal victory in 2006. “Psychotropic medication can have profound and lasting negative effects on a patient's mind and body,” the court wrote. These drugs “are known to cause a number of potentially devastating side effects.” As such, it ruled in Myers v. Alaska Psychiatric Institute that a psychiatric patient could be forcibly medicated only if a court “expressly finds by clear and convincing evidence that the proposed treatment is in the patient's best interest and that no less intrusive alternative is available.” Myers v. Alaska Psychiatric Institute, Alaska Supreme Court No. S-11021. fn 28 In Alaska case law, antipsychotics are no longer viewed as treatment that will necessarily help psychotic people.
It's never easy to hold a belief that is out of sync with what the rest of society believes, and in this instance, it's particularly difficult because the story of progress is told by figures of scientific authority—the APA, the NIMH, and psychiatrists at prestigious universities such as Harvard Medical School. Disagree with the common wisdom on this topic, and it seems that you must be a card-carrying member of the flat-Earth society. ” (Anatomy of an Epidemic, Robert Whitaker, p 361
To read many of the source documents listed here, go to madinamerica.com or robertwhitaker.org
-------------------------------------------
Raw book
To Lindsay
May you sing "Seasons of Love" again
and be filled with joy
Copyright 2010 by Robert Whitaker
All rights reserved.
Published in the United States by Crown Publishers, an imprint of the Crown Publishing Group, a division of Random House, Inc., New York.
www.crownpublishing.com
CROWN and the Crown colophon are registered trademarks of Random House, Inc.
Library of Congress Cataloging-in-Publication Data
Whitaker, Robert.
Anatomy of an epidemic : magic bullets, psychiatric drugs, and the astonishing rise of mental illness in America / Robert Whitaker.
p. ; cm.
Includes bibliographical references and index.
1. Mental. illness—United States. 2. Psychotropic drugs—Prescribing—United States. 3. Psychiatry—United States. I. Title.
[DNLM: 1. Psychiatry—ethics--United States. 2. Psychiatry—history—United States. 3. Mental Disorders—drug therapy—United States. 4. Mental Disordersepidemiology—United States. WM 11 AA1 W578a 2010]
RC443.W437 2010
616.89—dc22 2009049467
ISBN 978-0-307-45241-2
Printed in the United States of America
Illustrations by Hadel Studio, Westbury NY
10 9 8 7 6 5 4 3 2 1 First Edition
ANECDOTAL THOUGHTS • 13
Anecdotal Thoughts
"If we value the pursuit of knowledge, we must be free to follow wherever that search may lead us."
-ADLAI STEVENSON (1952)'
McLean Hospital in Belmont, Massachusetts, is one of the oldest mental hospitals in the United States, as it was founded in 1817, when a type of care known as moral therapy was being popularized by Quakers. Their belief was that a retreat for the mentally ill should be built in a pastoral setting, and even today the McLean campus, with its handsome brick buildings and shaded lawns, feels like an oasis. On the evening in August 2008 that I came there, in order to attend a meeting of the Depression and Bipolar Support Alliance, that sense of tranquility was heightened by the weather. It was one of the most gorgeous nights of the summer, and as I approached the cafeteria where the meeting was to be held, I figured that attendance that night would be sparse. It was just too nice of a night to be inside. This was a meeting for people living in the community, which meant they would have to leave their homes and apartments to come here, and given that the McLean group met five times a week—there was an afternoon session every Monday, Thursday, Friday, and Saturday, and an evening meeting every Wednesday—I reasoned that most people attached to the group would skip this one.
I was wrong.
There were a hundred or so people filling the cafeteria, a scene
that, in a small way, bore witness to the epidemic of disabling mental illness that has erupted in our country over the past twenty years. The Depression and Bipolar Support Alliance (DBSA) was founded in 1985 (known initially as the Depressive and Manic-Depressive Association), with this group at McLean starting up shortly after that, and today the organization counts nearly one thousand of its support groups nationwide. There are seven such groups in the Greater Boston area alone, and most—like the group that meets at McLean—offer people a chance to get together and talk several times a week. The DBSA has grown in lockstep with the epidemic.
The first hour of the meeting was given over to a talk about "flotation therapy," and at first glance, the audience was really not identifiable—at least not by an outsider such as myself—as a patient group. The people here ranged widely in age, the youngest in their late teens and the oldest in their sixties; and although the women outnumbered the men, this gender disparity might have been expected, given that depression affects more women than men. Most in the audience were white, which perhaps reflected the fact that Belmont is an affluent town. Perhaps the one telltale sign that the meeting was for people diagnosed with a mental illness was that a fair number were overweight. People diagnosed with bipolar disorder are often prescribed an atypical antipsychotic, such as Zyprexa, and those drugs regularly cause people to put on the pounds., p13
After the talk ended, Steve Lappen, one of the DBSA leaders in Boston, listed the various groups that would now meet. There was one for "newcomers," another for "family and friends," a third for "young adults," a fourth for "maintaining stability," and so on, with the last of the eight choices an "observer's group," which Steve had organized for me.
There were nine in our group (excluding myself), and by way of introduction, everyone briefly spoke about how he or she had been doing lately—"I've been having a hard time" was a common refrain—and told of his or her specific diagnosis. The man to my right was a former executive who had lost his job because of his recurring depression, and as we went around the room, such life stories spilled out. A younger woman told of a troubled marriage to
14 • ANATOMY OF AN EPIDEMIC
a Chinese man who, because of his culture, didn't like to talk about mental illness. Next to her, a former prosecuting attorney spoke of how he'd lost his wife two years ago, and since then "I don't feel like I know who I am." A woman who was an adjunct professor at an area college told of how difficult her work was at the moment, and finally, a nurse who had been recently hospitalized at McLean for depression explained what drove her to that dark place: She had the stress of caring for an ailing father, the stress of her job, and years of living with "an abusive husband."
The one lighter moment in this round of introductions came from the oldest member of the group. He had been doing pretty well lately, and his explanation for his relative happiness was one that Sein field's George Costanza would have appreciated. "Usually the summer is a hard time for me because everybody seems so happy. But with all the rain we have been having, that hasn't been so much the case this summer," he said.
Over the course of the next hour, the talk jumped from topic to topic. There was a discussion of the stigma that the mentally ill face in our society, particularly in the workplace, and talk too of how family and friends, after a time, lose their empathy. This was clearly why many in the group had come—they found the shared understanding to be helpful. The issue of medication came up, and on this topic, opinions and experiences varied widely. The former executive, while still regularly suffering from depression, said that his medication did "wonders" for him and that his greatest fear was that it would "stop working." Others told of having tried one medication after another before finding a drug regimen that provided some relief. Steve Lappen said that medications had never worked for him, while Dennis Hagler, the other DBSA leader in the meeting (who also agreed to be identified), said that a high dose of an antidepressant has made all the difference in the world in his life. The nurse told of having responded very badly to antidepressants during her recent hospitalization.
"I had an allergic reaction to five different drugs," she said. "I am now trying one of the new atypicals [antipsychotics]. I'm hoping that will work."
After the group sessions ended, people gathered in the cafeteria in
ANECDOTAL THOUGHTS • 15
clutches of two and three, sharing small talk. That made for a pleasant moment; there was a feeling of social warmth in that room, and you could see that the evening had lifted the spirits of many. It was all so ordinary that this easily could have been the wrap-up moment to a PTA meeting or a church social, and as I walked to the car, it was that ordinariness that struck me most. In the observer's group, there had been a businessman, an engineer, a historian, an attorney, a college professor, a social worker, and a nurse (the other two in the group hadn't spoken of their work histories). Yet, as far as I could tell, only the college professor was currently employed. And that was the puzzle: The people in the observer's group were well educated and they were all taking psychotropic medications, and yet many were so plagued by persistent depression and bipolar symptoms that they couldn't work.
Earlier, Steve had told me that about half of the DBSA members receive either an SSI or SSDI check because they are, in the government's eyes, disabled by their mental illness. This is the patient type that has been swelling the SSI and SSDI rolls for the past fifteen years, while the DBSA has grown into the largest mental health patient organization in the country during that time. Psychiatry now has three classes of medications it uses to treat affective disorders—antidepressants, mood stabilizers, and atypical antipsychotics—but for whatever reason, an ever greater number of people are showing up at DBSA meetings around the country, telling of their persistent and enduring struggles with depression or mania or both., p15
Four Stories
In medicine, the personal stories of patients diagnosed with a disease are known as "case studies," and it is understood that these anecdotal accounts, while they might provide insight into a disease and the treatments for it, cannot prove whether a treatment works. Only scientific studies that look at outcomes in the aggregate can do that, and even then the picture that emerges is often a cloudy one. The reason that anecdotal accounts can't provide such proof is that
• ANATOMY OF AN EPIDEMIC
coat, which you have been wearing even though it's a beautiful spring day, and suddenly feeling so much better, freer, nicer." The problem was that off the drugs, she would "start to decompensate and become disorganized."
In early 1994, she was hospitalized for the fifteenth time. She was seen as chronically mentally ill, occasionally heard voices now, had a new diagnosis (schizoaffective), and was on a cocktail of drugs: Haldol, Ativan, Tegretol, Halcion, and Cogentin, the last drug an antidote to Haldol's nasty side effects. But after she was released that spring, a psychiatrist told her to try Risperdal, a new anti-psychotic that had just been approved by the FDA. "Three weeks later, my mind was much clearer," she says. "The voices were going away. I got off the other meds and took only this one drug. I got better. I could start to plan. I wasn't talking to the devil anymore. Jesus and God weren't battling it out in my head." Her father put it this way: "Cathy is back."
Although several studies funded by the NIMH and the British government have found that patients, on the whole, don't do any better on Risperdal and the other atypicals than on the older anti-psychotics, Cathy clearly responded very well to this new agent. She went back to school and earned a degree in radio, film, and television from the University of Maryland. In 1998, she began dating the man she lives with today, Jonathan. In 2005, she took a part-time job as editor of Voices for Change, a newsletter published by M-Power, a consumer group in Massachusetts, a position she held for three years. In the spring of 2008, she helped lead an M-Power campaign to get the Massachusetts legislature to pass a law that would protect the rights of psychiatric patients in emergency rooms. Still, she remains on SSDI—"I am a kept woman," she jokes—and although there are many reasons for that, she believes that Risperdal, the very drug that has helped her so much, nevertheless has proven to be a barrier to full-time work. Although she is usually en-ergetic by the early afternoon, Risperdal makes her so sleepy that she has trouble getting up in the morning. The other problem is that she has always had trouble getting along with other people, and Risperdal exacerbates that problem, she says. "The meds isolate you. They interfere with your empathy. There is a flatness to you, and so you are uncomfortable with people all the time. They make it hard for you to get along. The drugs may take care of aggression and anxiety and some paranoia, those sorts of symptoms, but they don't help with the empathy that helps you get along with people.", Quoting Cathy Levin, p19
Risperdal has also taken a physical toll. Cathy is five feet, two inches tall, with curly brown hair, and although she is fairly physically fit, she is probably sixty pounds heavier than what would be considered ideal. She has also developed some of the metabolic problems, such as high cholesterol, that the atypical antipsychotics regularly cause. "I can go toe-to-toe with an old lady with a recital of my physical problems," she says. "My feet, my bladder, my heart, my sinuses, the weight gain—I have it all." Even more alarming, in 2006 her tongue began rolling over in her mouth, a sign that she may be developing tardive dyskinesia. When this side effect appears, it means that the basal ganglia, the part of the brain that controls motor movement, is becoming permanently dysfunctional, having been damaged by years of drug treatment. But she can't do well without Risperdal, and in the summer of 2008, this led to a moment of deep despair. "I will, of course, look pretty creepy in a few years, with the involuntary mouth movements," she says.
Such has been her life's course on medications. Sixteen terrible years, followed by fourteen pretty good years on Risperdal. She believes that this drug is essential to her mental health today, and indeed, she could be seen as a local poster child for promoting the wonders of that drug. Still, if you look at the long-term course of her illness, and you go all the way back to her first hospitalization at age eighteen, you have to ask: Is hers a story of a life made better by our drug-based paradigm of care for mental disorders, or a story of a life made worse? How might her life have unfolded if when she suffered her first manic episode in the fall of 1978, she had not been immediately placed on lithium and Haldol, the doctors instead trying other means—rest, psychological therapies, etc.—to restore her sanity? Or if, once she had been stabilized on those medications, she had been encouraged to wean herself from the drugs? Would she have spent sixteen years cycling through hospitals? Would she have gone on SSDI and remained on it ever since? What would her physical health be like now? What would her subjective experience
22 • ANATOMY OF AN EPIDEMIC
her. His grandmother took Madelyne to Puerto Rico, and George ended up divorced and living in a home for the disabled. There he met and married a woman also diagnosed with paranoid schizophrenia, and after a series of adventures and misadventures in San Francisco, they, too, got divorced. Despondent and paranoid once again, in early 1991 George landed in Kings Park Psychiatric Center, a run-down state hospital on Long Island.
Now came his descent into total hopelessness. After he tried to have a pistol smuggled into the hospital so that he could kill himself, he was given a two-year sentence in the locked facility. Then, as Christmas neared that year, he grew upset when several of his fellow patients weren't allowed to go home for the holiday, and so he helped them escape, breaking a window in his room and tying sheets together so they could clamber to the ground. The hospital responded by moving him to a ward for people who had been insti-tutionalized for decades. "Now I am on a ward with people urinating on themselves," he recalls. "I'm a danger to society and drugged out. You sit down all day and watch television. You can't even go outside. I thought my life was over."
George spent eight months on that ward for the hopelessly mentally ill, lost in a haze of drags. However, at last he was moved to a unit where he could go outside, and suddenly there was blue sky to be seen and fresh air to breathe. He felt a spark of hope, and then he took a very risky step: He began tonguing the antipsychotic medication and spitting it out when the staff weren't looking. "I could think again," he says. "The antipsychotic drugs weren't letting me think. I was like a vegetable, and I couldn't do anything. I had no emotions. I sat there and watched television. But now I felt more in control. And it felt great to feel alive again.", quoting George Badillo, p 23
Luckily, George didn't experience a return of psychotic symptoms, and with his body no longer slowed by drugs, he began to jog and lift weights. He fell in love with another patient in the hospital, Tara McBride, and in 1995, after they were both discharged from the hospital to a nearby community residence, she gave birth to Brandon. George, who had never completely lost touch with his daughter, Madelyne, now had a new goal in life. "I realize I have a second chance. I want to be a good parent."
ANECDOTAL THOUGHTS • 23
At first, it didn't go well. Like Madelyne, Brandon had been born with health problems—he had an intestinal abnormality that required surgery—and Tara broke down from that stress and was rehospitalized. Since George was still living in a residence for the mentally ill, the state did not deem him fit to care for Brandon and he was given to Tara's sister to raise. However, in 1998 George began working part-time as a peer specialist for the New York State Office of Mental Health, counseling hospitalized patients about their rights, and three years later, he was able to present himself in court as someone who could be a good father to Brandon. "My sister Madeline and I got custody," he says. "That was the best feeling. I was just jumping for joy. It was like the first time that someone in the system got custody of their kids."
The following year, one of George's sisters bought him the house he lives in today. Although he still receives SSDI, he does contract work for the federal Substance Abuse and Mental Services Health Administration and does volunteer work with hospitalized youth in Long Island. His is a life filled with meaning, and as Brandon's success in school will attest, he is proving to be the good father he dreamed of becoming. Madelyne, meanwhile, is unabashedly proud of him. "He wanted'to have Brandon and me in his life," she says. "That made him want to turn around his situation. He wanted to be a father to us. He is proof that someone can recover from mental illness."
Although George's story is clearly an inspiring one, it doesn't prove anything one way or another about the overall merits of antipsychotics. But it does prompt a clinical question: Given that his recovery began when he stopped taking antipsychotics, is it possible that some people ill with a serious mental disorder, like schizophrenia or bipolar illness, might recover in the absence of medication? Is his story an anomaly, or does it provide insight into what could be a fairly common path to recovery? George, who today occasionally takes Ambien or a low dose of Seroquel to sleep at night, believes that, at least in his case, getting off the drugs was what enabled him to get well. "If I had stayed on those drugs, I wouldn't be where I am today. I would be stuck in an adult home somewhere, or in the hospital. But I'm recovered. I still have some strange ideas, but now
24 • ANATOMY OF AN EPIDEMIC
I keep them to myself. And I weather whatever emotional stress
comes up. It stays with me for a few weeks and then it goes away."
Monica Briggs
Monica Briggs is a tall, intense woman and, like so many people active in the "peer recovery" movement, immensely likeable. On the day that I have lunch with her, at a restaurant in South Boston, she comes hobbling over to the booth leaning on a cane, as she recently injured herself, and when I ask how she traveled here, she smiles, slightly pleased with herself. "On my bike," she says.
Monica, who was born in 1967, is from Wellesley, Massachusetts, and as a teenager growing up in that affluent community, she seemed like the last person who might have a life of mental illness awaiting her. She came from an accomplished family—her mother was a professor at Wellesley, while her father taught at several Boston-area colleges—and Monica was a child who excelled at whatever she chose to do. She was a good athlete, earned top grades, and showed a particular talent for art and writing. Upon graduating from high school, she received several scholarship awards, and when she entered Middlebury College in Vermont in the fall of 1985, she believed that her life would follow a very conventional path. "I thought I'd go to school, marry, have a chocolate Labrador, and a home in the suburbs, with the SUV. . . . I thought it would all happen like that."
A month into her freshman year at Middlebury, Monica was blindsided by a severe depressive episode that seemed to have no cause. She'd never had emotional problems before, nothing bad had happened at Middlebury, and yet the depression hit her with such force that she had to leave school and return home. "I was someone who had never quit anything before," she says. "I thought my life was over. I thought this was a failure I could never recover from."
A few months later, she returned to Middlebury. She was taking an antidepressant (desipramine), and as spring neared, her spirits began to lift. However, they didn't just rise to a "normal" level. Instead, they soared beyond to what seemed a much better place. She now had energy to burn. She took long runs and threw herself into
ANECDOTAL THOUGHTS • 25
her art, dashing off accomplished self-portraits in charcoals and pastels. She had so little need for sleep that she started a T-shirt business. "It was fantastic, great," she says. "I am not thinking that I am God, or anything, but I am thinking I am pretty close to God at that point. This goes on for several weeks, and then I crash for what seems like forever."
This was the start of Monica's long battle with bipolar disorder. Depression had given way to mania followed by worse depression. Although she managed to complete her freshman year, with an A-minus average, she began cycling through depressive and manic episodes, and in May of her sophomore year, she gulped down handfuls of sleeping spills, intending to kill herself. Over the next fifteen years, she was hospitalized thirty times. While lithium kept her mania in check, the suicidal depression always came back, her doctors prescribing one antidepressant after another in an attempt to find the magic pill that would help her stay well.
There were times, between the hospitalizations, when she was fairly stable, and she made the most of them. In 1994, she earned a bachelor's degree from Massachusetts College of Art and Design, and after that she worked for various advertising agencies and publishing houses. She became active in the Depressive and Manic-Depressive Association and developed its logo, the "bipolar bear." But in 2001, after she was fired from her job for having stayed home for a week due to her depression, her suicidal impulses returned with a vengeance. She bought a gun, only to have it misfire six times when she tried to shoot herself. She spent three nights on a bridge that crossed a highway, desperately wanting to fling herself onto the roadway below, but refraining from doing so because she thought she might cause a crash that would hurt others. She was hospitalized several times, and then, in 2002, her mother died from pancreatic cancer, and her mental struggles took an even worse turn. "I am psychotic, hallucinating, seeing things. I think I have super powers and can change the way time flows. I think I have ten-feet wings and that I can fly."
That was the year she went on SSDI. Seventeen years after her initial manic episode, she had officially become disabled by bipolar disorder. "I hate it," she says. "I am a Wellesley girl on welfare, and
26 • ANATOMY OF AN EPIDEMIC
that's not what Wellesley girls are supposed to do. It is so corrosive to your self-esteem."
As might be guessed, given that she arrived at the diner on a bicycle, having pedaled there during her lunch break at work, Monica's life eventually took a turn for the better. In 2006, she stopped taking an antidepressant, and that triggered a "dramatic change." Her depression lifted, and she began working part-time at the Transformation Center, a Boston peer-run organization that helps people with psychiatric diagnoses. Although the lithium she has continued to take has its drawbacks—"my ability to create artwork is gone," she says—it hasn't exacted too great a physical toll. While she has a thyroid problem and suffers from tremors, her kidneys are fine. "I'm in recovery now," she says, and as we get up to leave the diner, she makes it clear that she would like to secure a full-time job and get off SSDI. "Being on welfare is a phase in my life," she says emphatically, "not an end."
Such has been the long arc of her illness. As a clinical study, her story appears to tell simply of the benefits of lithium. That drug apparently kept her mania in check for decades, and as a monotherapy, it has helped keep her stable since 2006. Still, after years of drug treatment, she ended up on SSDI, and as such, her story illustrates one of the core mysteries of this disability epidemic. How did someone so smart and accomplished end up on that governmental program? And if we wind the clock back to the spring of 1986, a perplexing question appears: Did she suffer her first manic episode because she was "bipolar," or did the antidepressant induce the mania? Is it possible that the drug converted her from someone who had suffered a depressive episode into a bipolar patient, and thus put her onto a path of chronic illness? And did the subsequent use of antidepressants alter the course of her "bipolar illness," for one reason or another, for the worse?
To put it another way, in the world of people who attend DBSA meetings, how often do they tell of becoming bipolar after initial treatment with an antidepressant?
ANECDOTAL THOUGHTS • 27
Dorea Vierling-Clausen
If you had met Dorea Vierling-Clausen in 2002, when she was twenty-five years old, she would have told you that she was "bipolar." She'd been so diagnosed in 1998, her psychiatrist explaining that she suffered from a chemical imbalance in the brain, and by 2002 she was on a cocktail of drugs that included an antipsychotic, Zyprexa. But by the fall of 2008, she was off all psychiatric medications (and had been for two years), she was thriving in a life that revolved around marriage, motherhood, and postdoctoral research at Massachusetts General Hospital, and she was convinced that her "bipolar" years had all been a big mistake. She believes that she was one of the millions of Americans caught up in a frenzy to diagnose the disorder, and it very nearly ended with her becoming a mental patient for life.
"I escaped by the skin of my teeth," she says.
Dorea tells me her story while sitting in the kitchen of her condominium in Cambridge, Massachusetts. Her spouse, Angela, is here, and their two-year-old daughter is sleeping in the next room. With her freckles and slightly frizzy hair, and evident zest for life, Dorea seems like someone who might have been a bit of a mischievous child, and to a certain extent, that is how she remembers herself. "I was extremely smart, at the far end of that spectrum, and so I was the geeky kid. But I had friends. I was skillful at social navigation—I was also the funny kid." If there was one thing amiss in her life as a child, it was that she was overly emotional, prone to "angry outbursts" and "crying" jags. "Delightful, but odd" is how she sums up her seven-year-old self.
Like many bright "odd" kids, Dorea found pursuits she excelled at. She developed a passion for the trumpet and became an accomplished musician. A top student, she had a particular talent for mathematics. In high school, she ran on the track team and had many friends. However, she remained quite emotional—that part of her personality did not go away—and there was a very real source of distress in her life: She was coming to understand that she was a lesbian. Her parents were "extremely conservative Christians," and while she loved them and deeply admired their devotion to social
28 • ANATOMY OF AN EPIDEMIC
justice—her father, a physician, volunteered half of his time to work in a clinic he'd founded in Denver's tough "Five Points" neighborhood—she feared that because of their religious beliefs, they wouldn't accept her deviant sex. After Dorea's freshman year at Peabody Institute, a prestigious music conservatory in Baltimore, she took a deep breath and told them her secret. "It went pretty much as awfully as could be expected," she says. "There were tears, a gnashing of teeth. It was so desperately ingrained in their religious thinking."
Dorea barely spoke to her parents for the next two years. She dropped out of Peabody and fell in with a punk crowd that lived in downtown Denver. The once aspiring trumpeter now ran around town with a shaved head and wearing combat boots. After working for a year at a shop that restored rugs, she enrolled at Metro State College, a commuter school. There she struggled constantly with her emotions, often crying iri public, and soon she began seeing a therapist, who diagnosed her as depressed. Eventually she began to take an antidepressant, and during finals week in the spring of 1998, she found that she couldn't sleep. When she showed up at her therapist's office agitated and a little manic, he had a new explanation for all that bedeviled her: bipolar illness. "I was told it was chronic and that my episodes would increase in frequency, and that I would need to be on drugs for the rest of my life," she recalls.
Although this foretold a bleak future, Dorea took comfort in the diagnosis. It explained why she was so emotional. This also was a diagnosis common to many great artists. She read Kay Jamison's book Touched with Fire and thought, "I am just like all these famous writers. This is great." She now had a new identity, and as she resumed her academic career, she arrived at each new institution—first at the University of Nebraska for an undergraduate degree and then at Boston University for a Ph.D. in math and biology—with a "giant box of pills." The cocktail she took usually included a mood stabilizer, an antidepressant, and a benzodiazepine for anxiety, although the exact combination was always changing. One drug would make her sleepy, another would give her tremors, and none of the cocktails seemed to bring her emotional tranquility. Then, in
ANECDOTAL THOUGHTS • 29
2001, she was put on an antipsychotic, Zyprexa, which, in a sense,
worked like a charm.
"You know what?" she says today, amazed by what she is about to confess. "I loved the stuff. I felt like I finally found the answer. Because what do you know. I have no emotions. It was great. I
wasn't crying anymore."
Although Dorea did well academically at Boston University, she still felt "really stupid" on Zyprexa. She slept ten, twelve hours a day, and like so many people on the drug, she began to blimp up, putting on thirty pounds. Angela, who had met and fallen in love with Dorea prior to her going on Zyprexa, felt a sense of loss: "She wasn't as lively anymore, she didn't laugh," she says. But they both understood that Dorea needed to be on the medications, and they began organizing their lives—and their plans for the future—around her bipolar illness. They attended DBSA meetings, and they began to think that Dorea should scale back her career goals. She probably wouldn't be able to handle the stress of postdoctoral research; her previous work in a rug shop seemed about right. "That sounds insane now," says Angela, who is a professor of mathematics at Lesley College. "But at the time, she wasn't a very resilient person, and she was becoming more and more dependent. I had to bear the weight of caretaking."
Dorea's possibilities were diminishing, and she might have continued down that path except for the fact that
in 2003 she [Dorea Vierling-Clausen] stumbled across some literature that raised questions about Zyprexa's longterm safety and the merits of antipsychotic drugs. That led her to wean herself from that drug, and while that process was "pure hell"—she suffered terrible anxiety, severe panic attacks, paranoia, and horrible tremors—she eventually did get off that medication. She then decided to see if she could get off the benzodiazepine she was taking, Klonopin, and that turned into another horrible withdrawal experience, as she suffered such severe headaches she'd be in bed by noon. Still, she was gradually undoing her drug cocktail, and that caused her to question her bipolar diagnosis. She had first seen a therapist because she cried too much. There had been no mania—her sleeplessness and agitation hadn't arisen until after she had been placed on an antidepressant. Could she just have been a moody teenager who had some growing up to do? , p 29
"I had always thought before that I was one of those cases where the illness was clearly biological," she says. "It couldn't have been situational. Nothing had gone terribly wrong in my life. But then I thought, well, I came out as a lesbian, and I had no family support. Duh. That could have been kind of stressful."
The mood stabilizers were the last to go, and on November 22, 2006, Dorea pronounced herself drug free. "It was fabulous. I was surprised to find out who I was after all these years," she says, adding that having shed the bipolar label in her own mind, her sense of personality responsibility changed, too. "When I was 'bipolar,' I had an excuse for any unpredictable or unstable behavior. I had permission to behave in that way, but now I am holding myself to the same behavioral standards as everyone else, and it turns out I can meet them. This is not to say that I don't have bad days. I do, and I may still worry more than the average Joe, but not that much more.", quoting Dorea Vierling-Clausen, p 30
Dorea's research at Massachusetts General Hospital focuses on how vascular activity affects brain function, and given that her struggles with "mental illness" can seemingly be chalked up as a case of misdiagnosis—"I have this fantasy of being undiagnosed as bipolar," she says—it may seem that her story is irrelevant to this book. But, in fact, her story raises a possibility that could go a long way toward explaining the epidemic of disabling mental illness in the United States. If you expand the boundaries of mental illness, which is clearly what has happened in this country during the past twenty-five years, and you treat the people so diagnosed with psychiatric medications, do you run the risk of turning an angst-ridden teenager into a lifelong mental patient? Dorea, who is an extremely smart and capable person, barely escaped going down that path. Hers is a story of a possible iatrogenic process at work, of an otherwise normal person being made chronically sick by diagnosis and subsequent treatment. And thus we have to wonder: Do we have a paradigm of care that can, at times, create mental illness?
ANECDOTAL THOUGHTS • 31
The Parents' Dilemma
Early during the course of my reporting for this book, I met with two families in the Syracuse area who, a few years back, had been faced with deciding whether to put their children on a psychiatric medication. The reason that I had paired these two families up in my mind was that they had come to opposite conclusions about what was best for their child, and I was curious to know what information they had at their disposal when they made their decisions.
I first went to see Gwendolyn and Sean Oates. They live on the south side of Syracuse, in a pleasant house perched on a slight hill. A gracious, biracial couple, they have two children, Nathan and Alia, and as we spoke, Nathan—who was then eight years old—spent most of the time sprawled out in the living room, drawing pictures in a sketchbook with colored pencils.
"We began to worry about him when he was three," his mother says. "We noticed that he was hyperactive. He couldn't sit through a meal, he couldn't even sit down. Dinnertime consisted of him running around the table. It was the same thing in his preschool—he couldn't sit still. He wasn't sleeping either. It would take us until nine thirty or ten p.m. to get him down. He would be kicking and screaming. These were not normal temper tantrums."
They first took Nathan to his pediatrician. However, she was reluctant to diagnose him, and so they took him to a psychiatrist, who quickly concluded that Nathan suffered from "attention deficit hyperactivity disorder." His problem, the psychiatrist explained, was "chemical" in kind. Although they were nervous about putting Nathan on Ritalin—"We were going through this on our own, and we didn't know anything about ADHD," his mother says—kindergarten was looming, and they reasoned that it would be the best thing for him. "The hyperactivity was holding him back from learning," his mother says. "The school didn't even want us to send him to kindergarten, but we said, 'No, we are going to.' We made the decision to keep him moving forward."
At first, there was a period of "trial and error" with the medications. Nathan was put on a high dose of Ritalin, but "he was like a
32 • ANATOMY OF AN EPIDEMIC
zombie," his mother recalls. "He was calm but he didn't move. He stared off into space." Nathan was then switched to Concerta, a long-lasting stimulant, and he stabilized well on it. However, at some point, Nathan began to exhibit obsessive behaviors, such as refusing to step on the grass or constantly needing to have something in his hands, and he was put on Prozac to control those symptoms. While on that two-drug combo, he started having terrible "rages." He kicked out his bedroom window during one episode, and he repeatedly threatened to kill his sister and even his mother. He was taken off the Prozac, and although his behavior improved somewhat, he continued to be quite aggressive, and he was diagnosed as suffering from both bipolar and ADHD.
"They say that ADHD and bipolar go hand in hand," his mother says. "And now that we know that he is bipolar, too, we think he will probably be on drugs for the rest of his life."
Since that time, Nathan has been on a drug cocktail. When I visited, he was taking Concerta in the morning, Ritalin in the afternoon, and three low doses of Risperdal—an antipsychotic—at various times during the day. This combo, his parents say, works fairly well for him. While Nathan is still moody, he doesn't fly off into total rages, and his hostility toward his younger sister has abated. He does struggle with his schoolwork, but he is moving ahead from grade to grade, and he gets along fairly well with his classmates. The biggest worry that his parents have about the medications is that they may be stunting his growth. Nathan is smaller than his sister, even though he is three years older. However, the physician's assistant and others who are treating Nathan don't talk much about how the drugs may affect him over the long term. "They don't worry about that," his father says. "It's helping him now."
At the end of the interview, Nathan shows me his drawings. He is into sharks and dinosaurs, and after I tell him how much I like his artwork, he seems almost to blush. He has been quiet most of the time I have been there, and even a little subdued, but we shake hands as I get ready to leave, and he seems, at that particular moment, to be a very sweet and gentle kid.
ANECDOTAL THOUGHTS • 33
Jason and Kelley Smith live on the west side of Syracuse, about thirty minutes distant from the Oates family, and when I knocked on their door, it was their seven-year-old daughter, Jessica, who answered. It appeared that she had been waiting for me, and once I had my tape recorder on, she plunked down on the couch between her mother and me, ready to pipe in with her side of the story. "Jessica," her father says a short while later, "has a lot of charisma."
Jessica's behavioral problems began at age two when she was sent to day care. When she got angry, she would hit and bite the other children. At home, she started having "night terrors" and all-out meltdowns. "The mildest thing would trigger her and she would be off," her mother says.
The Smiths turned to their local school district for help. The district recommended that Jessica go to a "special ed" preschool in north Syracuse, and when she continued to behave aggressively at that school, they were told to take Jessica to the Health Sciences Center at the State University of New York for a psychiatric evaluation. There they saw a nurse practitioner, who immediately concluded that Jessica was "bipolar." The practitioner explained that Jessica had a chemical imbalance and recommended that Jessica be put on a cocktail of three drugs: Depakote, Risperdal, and lithium.
"It blew my mind, especially the thought of putting her on anti-psychotics," Jason says. "She was four years old."
He and his wife left that consultation not knowing what to do. Kelley works for Oswego County's family service agency, and she knew of many troubled children who had been put on psychiatric medications. In that setting, the county expected parents to comply with medical advice. "There was part of me that thought maybe Jessica is bipolar, that's what it is," Kelley says. Moreover, SUNY Health Sciences told the Smiths that the center wouldn't see Jessica again if she weren't medicated. All of this pointed to following the center's advice—the "experts are telling you that you need to do this, and that it is biological," Jason says—but he had previously worked as a pharmacy technician and knew that drugs could have powerful side effects. "I was scared out of my mind."
Kelley used the Internet to research the drugs that had been recommended. However, she couldn't find any study that told of good
34 • ANATOMY OF AN EPIDEMIC
long-term outcomes for children placed on such drug cocktails, and even the short-term side effects, she remembers, "were scary." Meanwhile, Jessica's pediatrician told them she thought it would be "absurd" to put Jessica on psychiatric drugs; Jason and Kelley's families also thought it would be a mistake. Jason remembered how a few years earlier talk therapy had helped him address his own "anger management" issues, and if he had been able to change without the use of medications, couldn't Jessica change her behavior too?
"We just didn't want to accept [the bipolar diagnosis]. Jessica is such an outgoing child, and we like to think she is gifted," Kelley says. "And she had made so much progress from the time she was two years old. We just couldn't see giving her the medications."
They made that decision in 2005, and three years later, they say, Jessica is doing well. She gets mostly A's in school; her teachers now think that her earlier bipolar diagnosis was "crazy." While she does sometimes quarrel with other kids and will lash back verbally if another child teases her, she knows that she can't hit anyone. At home, she still has the occasional meltdown, but her emotional outbursts are not so extreme as before. Jessica even has her own advice on how all parents should handle such tirades: "They should say [to their child] 'come here,' and then they should rub them on the back so they feel better and so they can't have a meltdown, and so when they stop having a meltdown, that's what they will remember."
Before I leave, Jessica reads to me the book The Little Old Lady Who Was Not Afraid of Anything, and more than once she jumps to the floor to act out a scene. "Even with her behavioral issues, everybody loves her," her father says. "And that's what we were afraid of, with the medication, was that it would totally change her, and her personality. We didn't want to impair her faculties. We just want her to grow up to be healthy and to succeed in life."
Two different families, two different decisions. Both families now saw their decision as the right one, and both believed that their child was on a better path than he or she otherwise would have been. That was heartening, and I promised to check in with both families
ANECDOTAL THOUGHTS • 35
later, toward the end of my reporting for this book. Still, Nathan and Jessica were clearly on different paths, and as I drove back to Boston, all I could think about was how both sets of parents had needed to make their decision, on whether to medicate their child, in a scientific vacuum. Did their child really suffer from a chemical imbalance? Were there studies showing that drug treatment for ADHD or juvenile bipolar illness is beneficial over the long term? If you put a young child on a drug cocktail that includes an anti-psychotic, how will it affect his or her physical health? Can the child expect to become a healthy teenager, a healthy adult?
42 • ANATOMY OF AN EPIDEMIC
dicted that infectious diseases might soon be wiped from the face of the earth. A few years later, President Dwight D. Eisenhower called for the "unconditional surrender" of all microbes.5
As the 1950s began, medicine could look back and count numerous other successes as well. Pharmaceutical firms had developed improved anesthetics, sedatives, antihistamines, and anticonvulsants, evidence of how scientists were getting better at synthesizing chem-icals that acted on the central nervous system in helpful ways. In 1922, Eli Lilly had figured out how to extract the hormone insulin from the pancreas glands of slaughterhouse animals, and this provided doctors with an effective treatment for diabetes. Although re-placement insulin didn't rise to the level of a magic-bullet cure for the illness, it came close, for it provided a biological fix for what was missing in the body. In 1950, British scientist Sir Henry Dale, in a letter to the British Medical Journal, summed up this extra-ordinary moment in medicine's long history: "We who have been able to watch the beginning of this great movement may be glad and proud to have lived through such a time, and confident that an even wider and more majestic advance will be seen by those living through the fifty years now opening."6
The United States geared up for this wondrous future. Prior to the war, most basic research had been privately funded, with Andrew Carnegie and John D. Rockefeller the most prominent benefactors, but once the war ended, the U.S. government established the National Science Foundation to federally fund this endeavor. There were still many diseases to conquer, and as the nation's leaders looked around for a medical field that had lagged behind, they quickly found one that seemed to stand above all the rest. Psychiatry, it seemed, was a discipline that could use a little help.
Imagining a New Psychiatry
As a medical specialty, psychiatry had its roots in the nineteenth-
century asylum, its founding moment occurring in 1844, when
thirteen physicians who ran small asylums met in Philadelphia to
THE ROOTS OF AN EPIDEMIC • 43
form the Association of Medical Superintendents of American Institutions for the Insane. At that time, the asylums provided a form of environmental care known as moral therapy, which had been introduced into the United States by Quakers, and for a period, it pro-duced good results. At most asylums, more than 50 percent of newly admitted patients would be discharged within a year, and a significant percentage of those who left never came back. A nineteenth-century long-term study of outcomes at Worcester State Lunatic Asylum in Massachusetts found that 58 percent of the 984 patients discharged from the asylum remained well throughout the rest of their lives. However, the asylums mushroomed in size in the latter part of the 1800s, as communities dumped the senile elderly and patients with syphilis and other neurological disorders into the institutions, and since these patients had no chance of recovering, moral therapy came to be seen as a failed form of care.
At their 1892 meeting, the asylum superintendents vowed to leave moral therapy behind and instead utilize physical treatments. This was the dawn of a new era in psychiatry, and in very short order, they began announcing the benefits of numerous treatments of this kind. Various water therapies, including high-pressure showers and prolonged baths, were said to be helpful. An injection of extract of sheep thyroid was reported to produce a 50 percent cure rate at one asylum; other physicians announced that injections of metallic salts, horse serum, and even arsenic could restore lucidity to a mad mind. Henry Cotton, superintendent at Trenton State Hospital in New Jersey, reported in 1916 that he cured insanity by removing his patients' teeth. Fever therapies were said to be beneficial, as were deep-sleep treatments, but while the initial reports of all these somatic therapies told of great success, none of them stood the test of time.
In the late 1930s and early 1940s, asylum psychiatrists embraced a trio of therapies that acted directly on the brain, which the popular media—at least initially—reported as "miracle" cures. First came insulin coma therapy. Patients were injected with a high dose of insulin, which caused them to lapse into hypoglycemic comas, and when they were brought back to life with an injection of glucose, the New York Times explained, the "short circuits of the brain
44 • ANATOMY OF AN EPIDEMIC
vanish, and the normal circuits are once more restored and bring back with them sanity and reality."' Next came the convulsive therapies. Either a poison known as Metrazol or electroshock was used to induce a seizure in the patient, and when the patient awoke, he or she would be free of psychotic thoughts and happier in spirit—or so the asylum psychiatrists said. The final "breakthrough" treatment was frontal lobotomy, the surgical destruction of the frontal lobes apparently producing an instant cure. This "surgery of the soul," the New York Times explained, "transforms wild animals into gentle creatures in the course of a few hours."8
With such articles regularly appearing in major newspapers and magazines like Harper's, Reader's Digest, and the Saturday Evening Post, the public had reason to believe that psychiatry was making great strides in treating mental illness, participating in medicine's great leap forward, but then, in the wake of World War II, the public was forced to confront a very different reality, one that produced a great sense of horror and disbelief. There were 425,000 people locked up in the country's mental hospitals at that time, and first • Life magazine and then journalist Albert Deutsch, in his book The Shame of the States, took Americans on a photographic tour of the decrepit facilities. Naked men huddled in barren rooms, wallowing in their own feces. Barefoot women clad in coarse tunics sat strapped to wooden benches. Patients slept on threadbare cots in sleeping wards so crowded that they had to climb over the foot of their beds to get out. These images told of unimaginable neglect and great suffering, and at last, Deutsch drew the inevitable comparison:
As I passed through some of Byberry's wards, I was reminded of the Nazi concentration camps at Belsen and Buchenwald. I entered buildings swarming with naked humans herded like cattle and treated with less concern, pervaded by a fetid odor so heavy, so nauseating, that the stench seemed to have almost a physical existence of its own. I saw hundreds of patients living under leaking roofs, surrounded by moldy, decaying walls, and sprawling on rotting floors for want of seats or benches.9
THE ROOTS OF AN EPIDEMIC • 45
The nation clearly needed to remake its care of the hospitalized mentally ill, and even as it contemplated that need, it found reason to worry about the mental health of the general population. During the war, psychiatrists had been charged with screening draftees for psychiatric problems, and they had deemed 1.75 million American men mentally unfit for service. While many of the rejected draftees may have been feigning illness in order to avoid conscription, the numbers still told of a societal problem. Many veterans returning from Europe were also struggling emotionally, and in September 1945, General Lewis Hershey, who was the director of the Selective Service System, told Congress that the nation badly needed to address this problem, which had remained hidden for so long. "Mental illness was the greatest cause of noneffectiveness and loss of manpower that we met" during the war, he said.1°
With mental illness now a primary concern for the nation—and this awareness coming at the very time that antibiotics were taming bacterial killers—it was easy for everyone to see where a long-term solution might be found. The country could put its faith in the transformative powers of science. The existing "medical" treatments said to be so helpful—insulin coma, electroshock, and lobotomy—would have to be provided to more patients, and then long-term solutions could arise from the same process that had produced such astonishing progress in fighting infectious diseases. Research into the biological causes of mental illnesses would lead to better treatments, both for those who were seriously ill and those who were only moderately distressed. "I can envisage a time arriving when we in the field of Psychiatry will entirely forsake our ancestry, forgetting that we had our beginnings in the poorhouse, the workhouse and the jail," said Charles Burlingame, director of the Institute of the Living in Hartford, Connecticut. "I can envisage a time when we will be doctors, think as doctors, and run our psychiatric institu-tions in much the same way and with much the same relationships as obtain in the best medical and surgical institutions."11
In 1946, Congress passed a National Mental Health Act that put the federal government's economic might behind such reform. The government would sponsor research into the prevention, diagnosis, and treatment of mental disorders, and it would provide grants to
46 • ANATOMY OF AN EPIDEMIC
states and cities to help them establish clinics and treatment centers. Three years later, Congress created the National Institute of Mental Health (NIMH) to oversee this reform.
"We must realize that mental problems are just as real as physical disease, and that anxiety and depression require active therapy as much as appendicitis or pneumonia," wrote Dr. Howard Rusk, a professor at New York University who penned a weekly column for the New York Times. "They are all medical problems requiring medical care."12
The stage had now been set for a transformation of psychiatry and its therapeutics. The public believed in the wonders of science, the nation saw a pressing need to improve its care of the mentally ill, and the NIMH had been created to make this happen. There was the expectation of great things to come and, thanks to the sales of antibiotics, a rapidly growing pharmaceutical industry ready to capitalize on that expectation. And with all those forces lined up, perhaps it is no surprise that wonder drugs for both severe and not-so-severe mental illnesses—for schizophrenia, depression, and anxiety—soon arrived. 4
Psychiatry's Magic Bullets
"It was the first drug cure in all of
psychiatric history."
-NATHAN KLINE
DIRECTOR OF RESEARCH AT ROCKLAND STATE
HOSPITAL IN NEW YORK (1974)'
The "magic bullet" model of medicine that had led to the discovery of the sulfa drugs and antibiotics was very simple in kind. First, identify the cause or nature of the disorder. Second, develop a treatment to counteract it. Antibiotics killed known bacterial invaders. Eli Lilly's insulin therapy was a variation on the same theme. The company developed this treatment after researchers came to understand that diabetes was due to an insulin deficiency. In each instance, knowledge of the disease came first—that was the magic formula for progress. However, if we look at how the first generation of psychiatric drugs was discovered, and look too at how they came to be called antipsychotics, anti-anxiety agents, and antidepressants—words that indicate they were antidotes to specific disorders—we see a very different process at work. The psychopharmacology revolution was born from one part science and two parts wishful thinking.
• ANATOMY OF AN EPIDEMIC
Delay and Pierre Deniker, began administering chlorpromazine to psychotic patients at St. Anne's Hospital in Paris, and soon use of the drug spread to asylums throughout Europe. Everywhere the reports were the same: Hospital wards were quieter, the patients easier to manage. Delay and Deniker, in a series of articles they published in 1952, described the "psychic syndrome" induced by chlorpromazine:
Seated or lying down, the patient is motionless on his bed, often pale and with lowered eyelids. He remains silent most of the time. If questioned, he responds after a delay, slowly, in an indifferent monotone, expressing himself with few words and quickly becoming mute. Without exception, the response is generally valid and pertinent, showing that the subject is capable of attention and of reflection. But he rarely takes the initiative of asking a question; he does not express his preoccupations, desires, or preference. He is, usually conscious of the amelioration brought on by the treatment, but he does not express euphoria. The apparent indifference or the delay of the response to external stimuli, the emotional and affective neutrality, the decrease in both initiative and preoccupation without alteration in conscious awareness or in intellectual faculties constitute the psychic syndrome due to the treatment.5
U.S. psychiatrists dubbed chlorpromazine, which was marketed in the United States as Thorazine, as a "major tranquilizer." Back in France, Delay and Deniker coined a more precise scientific term: This new drug was a "neuroleptic," meaning it took hold of the ner-vous system. Chlorpromazine, they concluded, induced deficits similar to those seen in patients ill with encephalitis lethargica. "In fact," Deniker wrote, "it would be possible to cause true encephalitis epidemics with the new drugs. Symptoms progressed from re-versible somnolence to all types of dyskinesia and hyperkinesia, and finally to parkinsonism."6 Physicians in the United States similarly understood that this new drug was not fixing any known pathology. "We have to remember that we are not treating diseases with this drug," said psychiatrist E. H. Parsons, at a 1955 meeting in Philadelphia on chlorpromazine. "We are using a neuropharmacologic agent to produce a specific effect." Fn 7, p50
At the same time that Rhone-Poulenc was testing phenothiazines for their possible magic-bullet properties against malaria, Frank Berger, a Czech-born chemist, was doing research of a somewhat similar kind in London, and his work led, in 1955, to the introduction of "minor tranquilizers" to the market.
During the war, Berger had been one of the scientists in Britain who had helped develop methods to produce medically useful quantities of penicillin. But penicillin was effective only against gram-positive bacteria (microbes that took up a stain developed by Danish scientist Hans Christian Gram), and after the war ended, Berger sought to find a magic bullet that could kill gram-negative microbes, the ones that caused a host of troubling respiratory, urinary, and gastrointestinal illnesses. At that time, there was a commercial disinfectant sold in Britain, called Phenoxetol, that was advertised as effective against gram-negative bacteria in the environment, and Berger, who worked for British Drug Houses, Ltd., tinkered with the active ingredient in that product, a phenylglycerol ether, in an effort to produce a product with superior antibacterial effects. When a compound called mephenesin proved promising, he gave it to mice to test its toxicity. "The compound, much to my surprise, produced reversible flaccid paralysis of the voluntary skeletal muscles unlike that I had ever seen before," Berger wrote.8
Berger had stumbled on a potent muscle-relaxing agent. That was curious enough, but what was even more surprising, the drug-paralyzed mice didn't show any signs of being stressed by their new predicament. He would put the animals on their backs and they would be unable to right themselves, and yet their "heart beat was regular, and there were no signs suggesting an involvement of the autonomic nervous system." The mice remained quiet and tranquil, and Berger found that even when he administered low doses of this amazing new compound to mice—the doses too small to cause muscle paralysis—they displayed this odd tranquility.
52 • ANATOMY OF AN EPIDEMIC
Berger realized that a drug of this sort might have commercial possibilities as an agent that allayed anxiety in people. However, mephenesin was a very short-acting drug, providing only a few minutes of peace. In 1947, Berger moved to the United States and went to work for Wallace Laboratories in New Jersey, where he synthesized a compound, meprobamate, that lasted eight times as long in the body as mephenesin. When Berger gave it to animals, he discovered that it also had powerful "taming" effects. "Monkeys after being given meprobamate lost their viciousness and could be more easily handled," he wrote.9
Wallace Laboratories brought meprobamate to market in 1955, selling it as Miltown. Other pharmaceutical companies scrambled to develop competitor drugs, and as they did so, they looked for compounds that would make animals less aggressive and numb to pain. At Hoffmann-La Roche, chemist Leo Sternbach identified chlordiazepoxide as having a "powerful and unique" tranquilizing effect after he gave it to mice that ordinarily could be prompted to fight by the application of electric shocks to their feet.1° Even with a low dose of the drug, the mice remained noncombative when shocked. This compound also proved to have potent taming effects in larger animals—it turned tigers and lions into pussycats. The final proof of chlordiazepoxide's merits involved another electric-shock exam. Hungry rats were trained to press a lever for food, and then they were taught that if they did so while a light in the cage blinked on, they would be shocked. Although the rats quickly learned not to press the lever while the light was on, they nevertheless exhibited signs of extreme stress—defecating, etc.—whenever it lit up their cage. But if they were given a dose of chlordiazepoxide? The light would flash and they wouldn't be the least bit bothered. Their "anxiety" had vanished, and they would even press the lever to get something to eat, unworried about the shock to come. Hoffmann-La Roche brought chlordiazepoxide to market in 1960, selling it as Librium.
For obvious reasons, the public heard little about the animal tests that had given rise to the minor tranquilizers. However, an article published in the Science News Letter was the exception to the rule, as its reporter put the animal experiments into a human frame of
PSYCHIATRY'S MAGIC BULLETS • 53
reference. If you took a minor tranquilizer, he explained, "this would mean that you might still feel scared when you see a car speeding toward you, but the fear would not make you run.""
Psychiatry now had a new drug for quieting hospitalized patients and a second one for easing anxiety, the latter a drug that could be marketed to the general population, and by the spring of 1957, it gained a medicine for depressed patients, iproniazid, which was marketed as Marsilid. This drug, which was dubbed a "psychic energizer," could trace its roots back to a poetically apt source: rocket fuel.
Toward the end of World War II, when Germany ran low on the liquid oxygen and ethanol it used to propel its V-2 rockets, its scientists developed a novel compound, hydrazine, to serve as a substitute fuel. After the war ended, chemical companies from the Allied countries swooped in to grab samples of it, their pharmaceutical divisions eager to see if its toxic properties could be harnessed for magic-bullet purposes. In 1951, chemists at Hoffmann-La Roche created two hydrazine compounds, isoniazid and iproniazid, that proved effective against the bacillus that caused tuberculosis. The novel medicines were rushed into use in several TB hospitals, and soon there were reports that the drug seemed to "energize" patients. At Staten Island's Sea View Hospital, Time magazine reported, "pa-tients who had taken the drugs danced in the wards, to the delight of news photographers."12,
The sight of TB patients doing a jig suggested that these drugs might have a use in psychiatry as a treatment for depression. For various reasons, iproniazid was seen as having the greater potential, but initial tests did not find it to be particularly effective in lifting spirits, and there were reports that it could provoke mania. Tuberculosis patients treated with iproniazid were also developing so many nasty side effects—dizziness, constipation, difficulty urinating, neuritis, perverse skin sensations, confusion, and psychosis—that its use had to be curtailed in sanitariums. However, in the spring of 1957, Nathan Kline, a psychiatrist at Rockland State Hospital in Orangeburg, New York, rescued iproniazid with a report that if depressed patients were kept on the drug long enough, for at
54 • ANATOMY OF AN EPIDEMIC
least five weeks, it worked. Fourteen of the sixteen patients he'd treated with iproniazid had improved, and some had a "complete remission of all symptoms.""
On April 7, 1957, the New York Times summed up iproniazid's strange journey: "A side effect of an ,anti-tuberculosis drug may have led the way to chemical therapy for the unreachable, severely depressed mental patient. Its developers call it an energizer as opposed to a tranquilizer."14
Such were the drugs that launched the psychopharmacology revolution. In the short span of three years (1954-1957), psychiatry gained new medicines for quieting agitated and manic patients in asylums, for anxiety, and for depression. But none of these drugs had been developed after scientists had identified any disease process or brain abnormality that might have been causing these symptoms. They arrived out of the post–World War II search for magic bullets against infectious diseases, with researchers, during that process, stumbling on compounds that affected the central nervous system in novel ways. The animal tests of chlorpromazine, meprobamate, and chlordiazepoxide revealed that these agents sharply curbed normal physical and emotional responses, but did so without causing a loss of consciousness. That was what was so novel about the major and minor tranquilizers. They curbed brain function in a selective manner. It was unclear how iproniazid worked—it seemed to rev up the brain in some way—but, as the New York Times had noted, its mood-lifting properties were properly seen as a "side effect" of an anti-tuberculosis agent.
The drugs were best described as "tonics." But in the media, a story of a much different sort was being told.
An Unholy Alliance
The storytelling forces in American medicine underwent a profound
shift in the 1950s, and to see how that is so, we need to briefly
PSYCHIATRY'S MAGIC BULLETS • 55
recount the history of the American Medical Association prior to that time. At the turn of the century, the AMA set itself up as the organization that would help the American public distinguish the good from the bad. At that time, there were fifty thousand or so medicinal products sold in the United States, and they were of two basic types. There were thousands of small companies that sold syrups, elixirs, and herbal remedies directly to the public (or as packaged goods in stores), with these "patent" medicines typically made from "secret" ingredients. Meanwhile, Merck and other "drug houses" sold their chemical preparations, which were known as "ethical" drugs, to pharmacists, who then acted as the retail vendors of these products. Neither group needed to prove to a govern-ment regulatory agency that its products were safe or effective, and the AMA, eager to establish a place for doctors in this freewheeling marketplace, set itself up as the organization that would do this assessment. It established a "propaganda 'department" to investigate the patent medicines and thus protect Americans from "quackery," and it established a Council on Pharmacy and Chemistry to conduct chemical tests of the ethical drugs. The AMA published the results of these tests in its journals and provided the best ethical drugs with its "seal of approval." The AMA also published each year a "useful drugs" book, and its medical journals would not allow advertisements for any drug that had not passed its vetting process.
With this work, the AMA turned itself into a watchdog of the pharmaceutical industry and its products. By doing so, the organization was both providing a valuable service to the public and furthering its members' financial interests, for its drug evaluations provided patients with a good reason to visit a doctor. A physician, armed with his book of useful drugs, could prescribe an appropriate one. And it was this knowledge, as opposed to any government-authorized prescribing power, that provided physicians with their value in the marketplace (in terms of providing access to medicines).
The selling of drugs in the United States began to change with the passage of the 1938 Food and Drug Cosmetics Act. The law required drug firms to prove to the Food and Drug Administration that their products were safe (they still did not have to prove that their drugs were helpful), and in its wake, the FDA began decreeing
58 • ANATOMY OF AN EPIDEMIC
Miracle Pills
Smith Kline and French, which obtained a license from Rhone-Poulenc to sell chlorpromazine in • the United States, secured FDA approval for Thorazine on March 26, 1954. A few days later, the company used its March of Medicine show to launch the product. Although Smith Kline and French had spent only $350,000 developing Thorazine, having administered it to fewer than 150 psychiatric patients prior to submitting its application to the FDA, the company's president, Francis Boyer, told viewers that this was a product that had gone through the most rigorous testing imagin-able. "It was administered to well over five thousand animals and proved active and safe for human administration," he said. "We then placed the compound in the hands of physicians in our great American medical centers to explore its clinical value and possible limitations. In all, over two thousand doctors in this country and Canada have used it. . . . The development of a new medicine is difficult and costly, but it is a job our industry is privileged to perform."21
Boyer's was a story of rigorous science at work, and less than three months later, Time, in an article titled "Wonder Drug of 1954?", pronounced Thorazine a "star performer." After a dose of Thorazine, the magazine explained, patients "sit up and talk sense with [the doctor], perhaps for the first time in months."22 In a follow-up article, Time reported that patients "willingly took [the] pills" and that once they did, they "fed themselves, ate heartily and slept well." Thorazine, the magazine concluded, was as important "as the germ-killing sulfas discovered in the 1930s."23
This was a magic-bullet reference that was impossible to miss, and other newspapers and magazines echoed that theme. Thanks to chlorpromazine, U.S. News and World Report explained, "patients who were formerly untreatable within a matter of weeks or months become sane, rational human beings."24 The New York Times, in a series of articles in 1954 and 1955, called Thorazine a "miracle" pill that brought psychiatric patients "peace of mind" and "freedom
PSYCHIATRY'S MAGIC BULLETS • 59
from confusion." Thorazine, newspapers and magazines agreed, had ushered in a "new era of psychiatry."25
With such stories being told about Thorazine, it was little wonder that the public went gaga when Miltown, in the spring of 1955, was introduced into the market. This drug, Time reported, was for "walk-in neurotics rather than locked-in psychotics," and according to what psychiatrists were telling newspaper and magazine reporters, it had amazing properties.26 Anxiety and worries fled so quickly, Changing Times explained, that it could be considered a "happy pill." Reader's Digest likened it to a "Turkish bath in a tablet." The drug, explained Consumer Reports, "does not deaden or dull the senses, and it is not habit forming. It relaxes the muscles, calms the mind, and gives people a renewed ability to enjoy life."27
psychiatry-harms-damages-society-anti-psychotic-drugs-cause-brain-damage-chlorpromazine-thorazine-1950ad.htm
psychiatry-harms-damages-society-anti-psychotic-drugs-cause-brain-damage-meprobamate-miltown-happy-pills-1953ad.htm
The brain is a machine that consists of sparks and soups.
The public rush to obtain this new drug was such that Wallace Laboratories and Carter Products, which were jointly selling meprobamate, struggled to keep up with the demand. Drugstores lucky enough to have a supply put out signs that screamed: YES, WE HAVE MILTOWN! The comedian Milton Berle said that he liked the drug so much that he might change his first name to Miltown. Wallace Laboratories hired Salvador Dali to help stoke Miltown fever, paying the great artist $35,000 to create an exhibit at an AMA convention that was meant to capture the magic of this new drug. Attendees walked into a darkened claustrophobic tunnel that represented the interior of a caterpillar—this was what it was like to be anxious—and then, as they emerged back into the light, they came upon a golden "butterfly of tranquility," this metamorphosis due to meprobamate. "To Nirvana with Miltown" is how Time described Dali's exhibit.28
There was one slightly hesitant note that appeared in newspaper and magazine articles during the introduction of Thorazine and Miltown. In the 1950s, many of the psychiatrists at top American medical schools were Freudians, who believed that mental disorder's were caused by psychological conflicts, and their influence led Smith Kline and French, in its initial promotion of Thorazine, to caution reporters that "there is no thought that chlorpromazine is a cure for mental illness, but it can have great value if it relaxes patients and
6o • ANATOMY OF AN EPIDEMIC
makes them accessible to treatment."29 Both Thorazine and
Miltown, explained the New York Times, should be considered as
"adjuncts to psychotherapy, not the cure."" Thorazine was called a
"major tranquilizer" and Miltown a "minor tranquilizer," and when Hoffmann-La Roche brought iproniazid to market, it was described as a "psychic energizer." These drugs, although they may have been remarkable in kind, were not antibiotics for the mind. As Life magazine noted in a 1956 article titled "The Search Has Only Started," psychiatry was still in the early stages of its revolution, for the "bacteria" of mental disorders had yet to be discovered."
Yet, in very short order, even this note of caution went by the wayside. In 1957, the New York Times reported that researchers now believed that iproniazid might be a "potent regulator of unbalanced cerebral metabolism."32 This suggested that the drug, which had been developed to fight tuberculosis, might be fixing something that was wrong in the brains of depressed patients. A second drug for depressed patients, imipramine, arrived on the market during this time, and in 1959 the New York Times called them "anti-depressants" for the first time. Both appeared to "reverse psychic states," the paper said." These drugs were gaining a new status, and finally psychiatrist Harold Himwich, in a 1958 article in Science, explained that they "may be compared with the advent of insulin, which counteracts symptoms of diabetes."34 The antidepressants were fixing something wrong in the brain, and when Hoffmann-La Roche brought Librium to market in 1960, it picked up on this curative message. Its new drug was not just another tranquilizer, but rather "the successor to this entire group. . . . Librium is the biggest step yet toward 'pure' anxiety relief as distinct from central sedation or hypnotic action. "3S Merck did the same, marketing its drug Suavitil as "a mood normalizer. . . . Suavitil offers a new and specific type of neurochemical treatment for the patient who is disabled
by anxiety, tension, depression, or obsessive-compulsive manifestations."36
The final step in this image makeover of the psychiatric drugs came in 1963. The NIMH had conducted a six-week trial of Thorazine and other neuroleptics, and after these drugs were shown to be more effective than a placebo in knocking down psychotic
PSYCHIATRY'S MAGIC BULLETS • 6r
symptoms, the researchers concluded that that the drugs should be regarded "as antischizophrenic in the broad sense. In fact, it is questionable whether the term 'tranquilizer' should be retained."37
With this pronouncement by the NIMH, the transformation of the psychiatric drugs was basically complete. In the beginning, Thorazine and other neuroleptics had been viewed as agents that made patients quieter and emotionally indifferent. Now they were "antipsychotic" medications. Muscle relaxants that had been developed for use in psychiatry because of their "taming" properties were now "mood normalizers." The psychic energizers were "antidepressants." All of these drugs were apparently antidotes to specific disorders, and in that sense, they deserved to be compared to antibiotics. They were disease-fighting agents, rather than mere tonics. All that was missing from this story of magic-bullet medicine was an understanding of the biology of mental disorders, but with the drugs reconceived in this way, once researchers came to understand how the drugs affected the brain, they developed two hypotheses that, at least in theory, filled in this gap.
Chemicals in the Brain
At the start of the 1950s, there was an ongoing debate among neurologists about how signals crossed the tiny synapses that separated neurons in the brain. The prevailing view was that the signaling was electrical in kind, but others argued for chemical transmission, a debate that historian Elliot Valenstein, in his book Blaming the Brain, characterized as the "war between the sparks and the soups." However, by the mid-1950s, researchers had isolated a, number of possible chemical messengers in the brains of rats and other mammals, including acetylcholine, serotonin, norepinephrine, and dopamine, and soon the "soup" model had prevailed.
With that understanding in place, an investigator at the NIMH, Bernard Brodie, planted the intellectual seed that grew into the theory that depression was due to a chemical imbalance in the brain. In 1955, in experiments with rabbits, Brodie reported that re-
62 • ANATOMY OF AN EPIDEMIC
serpine, an herbal drug used in India to quiet psychotic patients, lowered brain levels of serotonin. It also made the animals "lethargic" and "apathetic." Arvid Carlsson, a Swedish pharmacologist who had worked for a time in Brodie's lab, soon reported that reserpine also reduced brain levels of norepinephrine and dopamine (which jointly are known as catecholamines). Thus, a drug that depleted serotonin, norepinephrine, and dopamine in the brain seemed to make animals "depressed." However, investigators discovered that if animals were pretreated with iproniazid or imipramine before they were given reserpine, they didn't become lethargic and apathetic. The two "antidepressants," in one manner or another, apparently blocked reserpine's usual depletion of serotonin and the catecholamines.38
During the 1960s, scientists at the NIMH and elsewhere figured out how iproniazid and imipramine worked. The transmission of signals from the "presynaptic" neuron to the "postsynaptic" neuron needs to be lightning fast and sharp, and in order for the signal to be terminated, the chemical messenger must be removed from the synapse. This is done in one of two ways. Either the chemical is metabolized by an enzyme and shuttled off as waste, or else it flows back into the presynaptic neuron. Researchers discovered that ipro-niazid thwarts the first process. It blocks an enzyme, known as monoamine oxidase, that metabolizes norepinephrine and serotonin. As a result, the two chemical messengers remain in the synapse longer than normal. Imipramine inhibits the second process. It blocks the "reuptake" of norepinephrine and serotonin by the presynaptic neuron, and thus, once again, the two chemicals remain in the synapse longer than normal. Both drugs produce a similar end result, although they do so by different means., p62
In 1965, the NIMH's Joseph Schildkraut, in a paper published in the Archives of General Psychiatry, reviewed this body of research and set forth a chemical imbalance theory of affective disorders:
Those drugs [like reserpine] which cause depletion and inactivation of norepinephrine centrally produce sedation or depression, while drugs which increase or potentiate norepi-nephrine are associated with behavioral stimulation or excite-
PSYCHIATRY'S MAGIC BULLETS • 63
ment and generally exert an antidepressant effect in man. From these findings a number of investigators have formulated a hypothesis about the pathophysiology of the affective disorders. This hypothesis, which has been designated the "catecholamine hypothesis of affective disorders," proposes that some, if not all depressions are associated with an ab-solute or relative deficiency of catecholamines, particularly norepinephrine."
Although this hypothesis had its obvious limitations—it was, Schildkraut said, "at best a reductionistic oversimplification of a very complex biological state"—the first pillar in the construction of the doctrine known today as "biological psychiatry" had been erected. Two years later, researchers erected the second pillar: the dopamine hypothesis of schizophrenia.
Evidence for this theory arose from investigations into Parkinson's disease. In the late 1950s, Sweden's Arvid Carlsson and others suggested that Parkinson's might be due to a deficiency in dopamine. To test this possibility, Viennese neuropharmacologist Oleh Hornykiewicz applied iodine to the brain of a man who'd died from the illness, as this chemical turns dopamine pink. The basal ganglia, an area of the brain that controls motor movements, was known to be rich in dopaminergic neurons, and yet in the basal ganglia of the Parkinson's patient, there was "hardly a tinge of pink discoloration," Hornykiewicz reported.4°
Psychiatric researchers immediately understood the possible relevance of this to schizophrenia. Thorazine and other neuroleptics regularly induced Parkinsonian symptoms—the same tremors, tics, and slowed gait. And if Parkinson's resulted from the death of dopaminergic neurons in the basal ganglia, then it stood to reason that anti-psychotic drugs, in some manner or another, thwarted dopamine transmission in the brain. The death of dopaminergic neurons and the blocking of dopamine transmission would both produce a dopamine malfunction in the basal ganglia: Carlsson soon reported that Thorazine and the other drugs for schizophrenia did just that.
This was a finding, however, that told of drugs that "disconnected" certain brain regions. They weren't normalizing brain
64 • ANATOMY OF AN EPIDEMIC
function; they were creating a profound pathology. However, at this same time, researchers reported that amphetamines—drugs known to trigger hallucinations and paranoid delusions—elevated dopamine activity in the brain. Thus, it appeared that psychosis might be caused by too much dopamine activity, which the neuroleptics then curbed (and thus brought back into balance). If so, the drugs could be said to be antipsychotic in kind, and in 1967, Dutch scientist Jacques Van Rossum explicitly set forth the dopamine hypothesis of schizophrenia. "When the hypothesis of dopamine blockade by neuroleptic agents can be further substantiated, it may have fargoing consequences for the pathophysiology of schizophrenia. Overstimulation of dopamine receptors could then be part of the aetiology" of the disease.'"
PSYCHIATRY'S MAGIC BULLETS • 65
history of medicine itself."'" Roland Kuhn, who had "discovered" imipramine, reasoned that the development of antidepressants could properly be seen as "an achievement of the progressively developing human intellect."'" Anti-anxiety medicines, said Frank Berger, the creator of Miltown, were "adding to happiness, human achievement, and the dignity of man."45 Such were the sentiments of those who had led this revolution, and finally, at a 1970 symposium on biological psychiatry in Baltimore, Nathan Kline summed up what most of those in attendance understood to be true: They all had earned a place in the pantheon of great medical men.
"Medicine and science will be just that much different because we have lived," Kline told his colleagues. "Treatment and understanding of [mental] illness will forever be altered . . . and in our own way we will persist for all time in that small contribution we have made toward the Human Venture."46
Expectations Fulfilled
The revolution in mental health care that Congress had hoped for when it created the NIMH twenty years earlier was now—or so it seemed—complete. Psychiatric drugs had been developed that were antidotes to biological disorders, and researchers believed that the drugs worked by countering chemical imbalances in the brain. The horrible mental hospitals that had so shamed the nation at the end of World War II could now be shuttered, as schizophrenics—thanks to the new drugs—could be treated in the community. Those suffering from a milder disorder, like depression or anxiety, simply needed to reach into their medicine cabinets for relief. In 1967, one in three American adults filled a prescription for a "psychoactive" medication, with total sales of such drugs reaching $692 million.42
This was a narrative of a scientific triumph, and in the late 1960s and early 1970s, the men who had been the pioneers in this new field of "psychopharmacology" looked back with pride at their handiwork. "It was a revolution and not just a transition period," said Frank Ayd Jr., editor of the International Drug Therapy Newsletter. "There was an actual revolution in the history of psychiatry and one of the most important and dramatic epics in the
A Scientific Revolution . . . or a Societal Delusion?
Today, by retracing the discovery of the first generation of psychiatric drugs and following their transformation into magic bullets, we can see that by 1970 two possible histories were unfolding. One possibility is that psychiatry, in a remarkably fortuitous turn of events, had stumbled on several types of drugs that, although they produced abnormal behaviors in animals, nevertheless fixed various abnormalities in the brain chemistry of those who were mentally ill. If so, then a true revolution was indeed under way, and we can expect that when we review the long-term outcomes produced by these drugs, we will find that they help people get well and stay well. The other possibility is that psychiatry, eager to have its own magic pills and eager to take its pla.ce in mainstream medicine, turned the drugs into something they were not. These first-generation drugs were simply agents that perturbed normal brain function in some way, which is what the animal research had shown, and if that is so, then it stands to reason that the long-term outcomes produced by the drugs might be problematic in kind.
66 • ANATOMY OF AN EPIDEMIC
Two possible histories were under way, and in the 1970s and 1980s, researchers investigated the critical question: Do people diagnosed with depression and schizophrenia suffer from a chemical imbalance that is then corrected by the medication? Were the new drugs truly antidotes to something chemically amiss in the brain?
5
The Hunt for Chemical Imbalances
"The great tragedy of science—the slaying of a.
beautiful hypothesis by an ugly fact."
-THOMAS HUXLEY (1870)1
The adult human brain weighs about three pounds, and when you see it close up, removed from the skull, it is a bit larger than you imagined it to be. I had thought a brain could rest fairly easily in the palm of one's hand, but you really need both hands to lift it securely into the air. If the brain is fresh, not yet pickled in formaldehyde, a spiderweb of blood vessels pinkens the surface, and the tissue feels soft, almost gelatinous. It is definitely "biological" in kind, and yet somehow it gives rise to all of the mysterious and remarkable talents of the human mind. At the invitation of a friend, Jang-Ho Cha, who is a neuroscientist at Massachusetts General Hospital, I attended a brain-cutting seminar at the hospital, with the thought that seeing a human brain would help me better visualize the neurotransmitter pathways that are said to give rise to depression and psychosis, but naturally my visit turned into something more than that. The human brain up close takes your breath away.
The mechanics of its messaging system are fairly well understood. There are, Cha noted, 100 billion neurons in the human brain. The cell body of a "typical" neuron receives input from a vast web of dendrites, and it sends out a signal via a single axon that may project to a distant area of the brain (or down the spinal cord). At its end, an axon branches into numerous terminals, and it is from
70 • ANATOMY OF AN EPIDEMIC
memory, learning, sleep, appetite, and the regulation of moods and behaviors. As Efrain Azmitia, a professor of biology at NYU, has noted, "the brain serotonin system is the single largest brain system known and can be characterized as a 'giant' neuronal system."2
There are three major dopaminergic pathways in the brain. The cell bodies of all three systems are located atop the brain stem, in either the substantia nigra or the ventral tegmentum. Their axons project to the basal ganglia (nigrostriatal system), the limbic region (mesolimbic system), and the frontal lobes (mesocortical system). The basal ganglia initiates and controls movement. The limbic structures—the olfactory tubercle, the nucleus accumbens, and the amygdala, among others—are located behind the frontal lobes and help regulate our emotions. It is here that we feel the world, a process that is vital to our sense of self and our conceptions of reality. The frontal lobes are the most distinguishing feature of the human brain, and provide us with the godlike capacity to monitor our own selves.
All of this physiology—the 100 billion neurons, the 150 trillion synapses, the various neurotransmitter pathways—tell of a brain that is almost infinitely complex. Yet the chemical imbalance theory of mental disorders boiled this complexity down to a simple disease mechanism, one easy to grasp. In depression, the problem was that the serotonergic neurons released too little serotonin into the synaptic gap, and thus the serotonergic pathways in the brain were "underactive." Antidepressants brought serotonin levels in the synaptic gap up to normal, and that allowed these pathways to transmit mes-sages at a proper pace. Meanwhile, the hallucinations and voices that characterized schizophrenia resulted from overactive dopaminergic pathways. Either the presynaptic neurons pumped out too much dopamine into the synapse or the target neurons had an ab-normally high density of dopamine receptors. Antipsychotics put a brake on this system, and this allowed the dopaminergic pathways to function in a more normal manner.
That was the chemical imbalance theory put forth by Schildkraut and Jacques Van Rossum, and the very research that had led Schildkraut to his hypothesis also provided investigators with a method for testing it. The studies of iproniazid and imipramine had shown that neurotransmitters were removed from the synapse in one of two ways. Either the chemical was taken back up into the presynaptic neuron and restored for later use, or it was metabolized by an enzyme and carted off as waste. Serotonin is metabolized into 5-hydroxyindole acetic acid (5-HIAA); dopamine is turned into homovanillic acid (HVA). Researchers could comb the cerebrospinal fluid for these metabolites, and the amounts found would serve as an indirect gauge of the synaptic levels of the neurotransmitters. Since low serotonin was theorized to cause depression, anyone in that emotional state should have lower-than-normal levels of 5-HIAA in his or her cerebrospinal fluid. Similarly, since an overactive dopamine system was theorized to cause schizophrenia, people who heard voices or were paranoid should have abnormally high cerebrospinal levels of HVA. , p 70
This line of research kept scientists busy for nearly fifteen years.
The Serotonin Hypothesis Is Put to the Test
In 1969, Malcolm Bowers at Yale University became the first to report on whether depressed patients had low levels of serotonin metabolites in their cerebrospinal fluid. In a study of eight depressed patients (all of whom had been previously exposed to antidepres-sants), he announced that their 5-HIAA levels were lower than normal, but not "significantly" so.3 Two years later, investigators at McGill University said that they, too, had failed to find a "statistically significant" difference in the 5-HIAA levels of depressed patients and normal controls, and that they also had failed to find any correlation between 5-HIAA levels and the severity of depressive symptoms.4 In 1974, Bowers was back with a more finely tuned follow-up study: Depressed patients who had not been exposed to antidepressants had perfectly normal 5-HIAA levels.s
The serotonin theory of depression did not seem to be panning out, and in 1974, two researchers at the University of Pennsylvania, Joseph Mendels and Alan Frazer, revisited the evidence that had led Schildkraut to advance his theory in the first place. Schildkraut had
• ANATOMY OF AN EPIDEMIC
noted that reserpine, which depleted monoamines in the brain (norepinephrine, serotonin, and dopamine), regularly made people depressed. But when Mendels and Frazer looked closely at the scientific literature, they found that when hypertensive patients were given reserpine, only 6 percent in fact got the blues. Furthermore, in 1955, a group of physicians in England had given the herbal drug to their depressed patients, and it had lifted the spirits of many. Reserpine, Mendels and Frazer concluded, didn't reliably induce depres-sion at al1.6 They also noted that when researchers had given other monoamine-depleting drugs to people, those agents hadn't induced depression either. "The literature reviewed here strongly suggests that the depletion of brain norepinephrine, dopamine or serotonin is in itself not sufficient to account for the development of the clinical syndrome of depression," they wrote.'
It seemed that the theory was about to be declared dead and buried, but then, in 1975, Marie Asberg and her colleagues at the Karolinska Institute in Stockholm breathed new life into it. Twenty of the sixty-eight depressed patients they had tested suffered from low 5-HIAA levels, and these low-serotonin patients were somewhat more suicidal than the rest, with two of the twenty eventually committing suicide. This was evidence, the Swedish researchers said, that there might be "a biochemical subgroup of depressive dis-order characterized by a disturbance of serotonin turnover."8
Soon prominent psychiatrists in the United States were writing that "nearly 30 percent" of depressed patients had been found to have low serotonin levels. The serotonin theory of depression seemed at least partly vindicated. But today, if we revisit Asberg's study and examine her data, we can see that her finding of a "biological subgroup" of depressed patients was mostly a story of wishful thinking.
In her study, Asberg reported that 25 percent of her "normal" group had cerebrospinal 5-HIAA levels below fifteen nanograms per milliliter. Fifty percent had fifteen to twenty-five nanograms of 5-HIAA per milliliter, and the remaining 25 percent had levels above twenty-five nanograms. The bell curve for her "normals" showed that 5-HIAA levels were quite variable. But what she failed
THE HUNT FOR CHEMICAL IMBALANCES • 73
to note in her discussion was that the bell curve for the sixty-eight depressed patients in her study was almost exactly the same. Twenty-nine percent (twenty of the sixty-eight) had 5-HIAA counts below fifteen nanograms, 47 percent had levels between fifteen and twenty-five nanograms, and 24 percent had levels above twenty-five nanograms. Twenty-nine percent of depressed patients may have had "low" levels of serotonin metabolites in their cerebrospinal fluid (this was her "biological subgroup"), but then so did 25 percent of "normal" people. The median level for normals was twenty nanograms, and, it so turned out, more than half of the depressed patients—thirty-seven of sixty-eight—had levels above that amount.
Viewed in this way, her study had not provided any new reason to believe in the serotonin theory of depression. Japanese investigators soon revealed, in an unwitting way, the faulty logic at work. They reported that some antidepressants (used in Japan) blocked serotonin receptors, inhibiting the firing of those pathways, and thus they reasoned that depression might be caused by an "excess of free serotonin in the synaptic cleft."9 They had applied the same backwards reasoning that had given rise to the low-serotonin theory of depression, and if the Japanese scientists had wanted to, they could have pointed to Asberg's study for support of their theory, as the Swedes had found that 24 percent of depressed patients had "high" levels of serotonin.
In 1984, NIMH investigators studied the low-serotonin theory of depression one more time. They wanted to see whether the "biological subgroup" of depressed patients with "low" levels of serotonin were the best responders to an antidepressant, amitriptyline, that selectively blocked its reuptake. If an antidepressant was an antidote to a chemical imbalance in the brain, then amitriptyline should be most effective in that subgroup. But, lead investigator James Maas wrote, "contrary to expectations, no relationships between cerebrospinal 5-HIAA and response to amitriptyline were found." Fn 10. Moreover, he and the other NIMH researchers discovered—just as Asberg had—that 5-HIAA levels varied widely in depressed patients. Some had high levels of serotonin metabolites in their cerebrospinal fluid, while others had low levels. The NIMH scientists drew the only possible conclusion: "Elevations or decrements in the functioning of serotonergic systems per se are not likely to be associated with depression." Fn 10, p 74
Even after this report, the serotonin theory of depression did not completely go away. The commercial success of Prozac, a "selective serotonin reuptake inhibitor" brought to market in 1988 by Eli Lilly, fueled a new round of public claims that depression was due to low levels of this neurotransmitter, and once again any number of investigators conducted experiments to see if that were so. But this second round of studies produced the same results as the first. "I spent the first several years of my career doing full-time research on brain serotonin metabolism, but I never saw any convincing evidence that any psychiatric disorder, including depression, results from a deficiency of brain serotonin," said Stanford psychiatrist David Burns in 2003. Fn 11, p 74 Numerous others made this same point. "There is no scientific evidence whatsoever that clinical depression is due to any kind of biological deficit state," wrote Colin Ross, an associate professor of psychiatry at Southwest Medical Center in Dallas, in his 1995 book, Pseudoscience in Biological Psychiatry. Fn 12, p 74
In 2000, the authors of Essential Psychopharmacology told medical students "there is no clear and convincing evidence that monoamine deficiency accounts for depression; that is, there is no 'real' monoamine deficit." Fn 13, p 74
* The NIMH researchers also looked at a number of other possible associations between variable neurotransmitter levels and response to an antidepressant. They measured norepinephrine metabolites and dopamine metabolites; they divided their depressed patients into bipolar and unipolar groups; and they evaluated their response to two antidepressants, imipramine and amitriptyline. They found mild associations between several of these subgroups and their response to one or other of the drugs; I have focused here on their findings regarding whether (a) depression is due to low levels of serotonin, and (b) if the subgroup of patients with low levels of serotonin responds better to a drug that selectively blocks the reuptake of this neurotransmitter.
" Yet, fueled by pharmaceutical advertisements, the belief lived on, and it caused Irish psychiatrist David Healy, who has written a number of books on the history of psychiatry, to quip in 2005 that this theory needed to be put into the medical dustbin, where other such discredited theories can be found. "The serotonin theory of depression," he wrote, with evident exasperation, "is comparable to the masturbatory theory of insanity." Fn 14, p 74
Dopamine Deja Vu
When Van Rossum set forth his dopamine hypothesis of schizophrenia, he noted that the first thing that investigators needed to do was "further substantiate" that antipsychotic drugs did indeed thwart dopamine transmission in the brain. This took some time, but by 1975, Solomon Snyder at Johns Hopkins Medical School and Philip Seeman at the University of Toronto had fleshed out how the drugs achieved that effect. First, Snyder identified two distinct types of dopamine receptors, known as D1 and D2. Next, both in-vestigators found that antipsychotics blocked 70 to 90 percent of the D2 receptors.15 Newspapers now told of how these drugs might be correcting a chemical imbalance in the brain.
"Too much dopamine function in the brain could account for the overwhelming flood of sensations that plagues the schizophrenic," the New York Times explained. "By blocking the brain's receptor sites for dopamine, neuroleptics put an end to sights and sounds that are not really there."16
However, even as Snyder and Seeman were reporting their results, Malcolm Bowers was announcing findings that cast a cloud over the dopamine hypothesis. He had measured the level of dopamine metabolites in the cerebrospinal fluid of unmedicated schizophrenics and found them to be quite normal. "Our findings," he wrote, "do not furnish neurochemical evidence for an over-arousal in these patients emanating from a midbrain dopamine system."17 Others soon reported similar results. In 1975, Robert Post at the NIMH determined that HVA levels in the cerebrospinal fluid of twenty unmedicated schizophrenics "were not significantly different from controls."'" Autopsy studies also revealed that the brain tissue of drug-free schizophrenics did not have abnormal levels of
6 • ANATOMY OF AN EPIDEMIC
dopamine. In 1982, UCLA's John Haracz reviewed this body of research and drew the obvious bottom-line conclusion: "These findings do not support the presence of elevated dopamine turnover in the brains of [unmedicated] schizophrenics."19
Having discovered that dopamine levels in never-medicated schizophrenics were normal, researchers turned their attention to a second possibility. Perhaps people with schizophrenia had an overabundance of dopamine receptors. If so, the postsynaptic neurons would be "hypersensitive" to dopamine, and this would cause the dopaminergic pathways to be overstimulated. In 1978, Philip Seeman at the University of Toronto announced in Nature that this was indeed the case. At autopsy, the brains of twenty schizophrenics had 70 percent more D2 receptors than normal. At first glance, it seemed that the cause of schizophrenia had been found, but Seeman cautioned that all of the patients had been on neuroleptics prior to their deaths. "Although these results are apparently compatible with the dopamine hypothesis of schizophrenia in general," he wrote, the increase in D2 receptors might "have resulted from the long-term administration of neuroleptics." Fn 20
A variety of studies quickly proved that the drugs were indeed the culprit. When rats were fed neuroleptics, their D2 receptors quickly increased in number. Fn 21 If rats were given a drug that blocked D, receptors, that receptor subtype increased in density. Fn 22, In each instance, the increase was evidence of the brain trying to compensate for the drug's blocking of its signals. Then, in 1982, Angus MacKay and his British colleagues reported that when they examined brain tissue from forty-eight deceased schizophrenics, "the increases in [D2] receptors were seen only in patients in whom neuroleptic medication had been maintained until the time of death, indicating that they were entirely iatrogenic [drug-caused]." Fn 23 A few years later, German investigators reported the same results from their autopsy studies. Fn 24 Finally, investigators in France, Sweden, and Finland used positron emission topography to study D2-receptor densities in living patients who had never been exposed to neuroleptics, and all reported "no significant differences" between the schizophrenics and "normal controls." Fn 25 p76
THE HUNT FOR CHEMICAL IMBALANCES • 77
Since that time, researchers have continued to study whether there might be something amiss with the dopaminergic pathways in people diagnosed with schizophrenia, and now and then someone reports having found an abnormality of some type in a subset of pa-tients. But by the end of the 1980s, it was clear that the chemical-imbalance hypothesis of schizophrenia—that this was a disease characterized by a hyperactive dopamine system that was then put somewhat back into balance by the drugs—had come to a crashing end. "The dopaminergic theory of schizophrenia retains little credibility for psychiatrists," observed Pierre Deniker in 1990.26 Four years later, John Kane, a well-known psychiatrist at Long Island Jewish Medical Center, echoed the sentiment, noting that there was "no good evidence for any perturbation of the dopamine function in schizophrenia." Fn 27 Still, the public continued to be told that people diagnosed with schizophrenia had overactive dopamine systems, with the drugs likened to "insulin for diabetes," and thus former NIMH director Steve Hyman, in his 2002 book, Molecular Neuropharmacology, was moved to once again remind readers of the truth. "There is no compelling evidence that a lesion in the dopamine system is a primary cause of schizophrenia," he wrote. Fn 28
Requiem for a Theory
The low-serotonin hypothesis of depression and the high-dopamine hypothesis of schizophrenia had always been the twin pillars of the chemical-imbalance theory of mental disorders, and by the late 1980s, both had been found wanting. Other mental disorders have also been touted to the public as diseases caused by chemical imbalances, but there was never any evidence to support those claims. p 77
Parents were told that children diagnosed with attention deficit hyperactivity disorder suffered from low dopamine levels, but the only reason they were told that was because Ritalin stirred neurons to release extra dopamine. This became the storytelling formula that was relied upon by pharmaceutical companies again and again:
78 • ANATOMY OF AN EPIDEMIC
Researchers would identify the mechanism of action for a class of drugs, how the drugs either lowered or raised levels of a brain neurotransmitter, and soon the public would be told that people treated with those medications suffered from the opposite problem.
From a scientific point of view, it is apparent today that the chemical imbalance hypothesis was always wobbly in kind, and many of the scientists who watched its rise and fall have looked back on it with a bit of embarrassment. As early as 1975, Joseph Mendels and Alan Frazer had concluded that Schildkraut's hypothesis of depression had arisen out of "tunnel thinking" that relied on an "inadequate evaluation of certain findings not consistent with the initial assumption."29 In 1990, Deniker said that the same was true of the dopamine hypothesis of schizophrenia. When psychiatric researchers recast the drugs as "antischizophrenic" agents, he noted, they had gone "a bit far . . . one can say that neuroleptics diminish certain phenomena of schizophrenia, but [the drugs] do not pretend to be an etiological treatment of these psychoses." fn 30, p78
The chemical-imbalance theory of mental disorders, wrote David Healy, in his book The Creation of Psychopharmacology, was embraced by psychiatrists because it "set the stage" for them "to become real doctors."31 Doctors in internal medicine had their antibiotics, and now psychiatrists could have their "anti-disease" pills too.
Yet a societal belief in chemical imbalances has remained (for reasons that will be explored later), and it has led those who have investigated and written about this history to emphasize, time and again, the same bottom-line conclusion. "The evidence does not sup-port any of the biochemical theories of mental illness," concluded Elliot Valenstein, a professor of neuroscience at the University of Michigan, in his 1998 book Blaming the Brain. fn 32
Even U.S. surgeon general David Satcher, in his 1999 report Mental Health, confessed that "the precise causes [etiologies] of mental disorders are not known." fn 33
In Prozac Backlash, Joseph Glenmullen, an instructor of psychiatry at Harvard Medical School, noted that "in every instance where such an imbalance was thought to be found, it was later proved to be false." fn 34
Finally, in 2005, Kenneth Kendler, coeditor in chief of Psychological Medicine, penned an admirably succinct epitaph for this whole story: "We have hunted for big simple neurochemical explanations for psychiatric disorders and have not found them." fn 35
This brings us to our next big question: If psychiatric drugs don't fix abnormal brain chemistry, what do they do?
Prozac on My Mind
During the 1970s and 1980s, investigators put together detailed accounts of how the various classes of psychiatric drugs act on the brain, and how the brain in turn reacts to the drugs. We could relate the history of antidepressants, neuroleptics, benzodiazepines, or stimulants, and all of those histories would tell of a somewhat common process at work. But since the story of chemical imbalances in the public mind really took off after Eli Lilly brought Prozac (fluoxetine) to market, it seems appropriate to review what Eli Lilly scientists and other investigators, in reports published in scientific journals, had to say about how this "selective serotonin reuptake inhibitor" actually worked.
As was noted earlier, once a presynaptic neuron has released serotonin into the synaptic gap, it must be quickly removed so that the signal can be crisply terminated. An enzyme metabolizes a small amount; the rest is pumped back into the presynaptic neuron, entering via a channel known as SERT (serotonin reuptake transport). Fluoxetine blocks this reuptake channel, and as a result, Eli Lilly scientist James Clemens wrote in 1975, it causes a "pile-up of serotonin at the synapse."36
However, as the Eli Lilly investigators discovered, a feedback mechanism then kicks in. The presynaptic neuron has "auto-receptors" on its terminal membrane that monitor the level of serotonin in the synapse. If serotonin levels are too low, one scientist quipped, these autoreceptors scream "turn on the serotonin machine." If serotonin levels are too high, they scream "turn it off." This is a feedback loop designed by evolution to keep the serotonergic system in balance, and fluoxetine triggers the latter message. With serotonin no longer being whisked away from the synapse, the
8o • ANATOMY OF AN EPIDEMIC
autoreceptors tell the presynaptic neurons to fire at a dramatically lower rate. They begin to release lower-than-normal amounts of serotonin into the synapse.
Feedback mechanisms also change the postsynaptic neurons. Within four weeks, the density of their serotonin receptors drops 25 percent below normal, Eli Lilly scientists reported in 1981.37 Other investigators subsequently reported that "chronic fluoxetine treatment" may lead to a 50 percent reduction in serotonin receptors in certain areas of the brain.38 As a result, the postsynaptic neurons become "desensitized" to the chemical messenger.
At this point, it may seem that the brain has successfully adapted to the drug. Fluoxetine blocks the normal reuptake of serotonin from the synapse, but the presynaptic neurons then begin releasing less serotonin and the postsynaptic neurons become less sensitive to serotonin and thus don't fire so readily. The drug was designed to accelerate the serotonergic pathway; the brain responded by putting on the brake. It has kept its serotonergic pathway more or less in balance, an adaptive response that researchers have dubbed "synaptic resilience. "39 However, there is one other change that occurs during this initial two-week period, and it ultimately short-circuits the brain's compensatory response. The autoreceptors for serotonin on the presynaptic neurons decline in number. As a result, this feedback mechanism becomes partially disabled, and the "turn off the serotonin machine" message dims. The presynaptic neurons begin to fire at a normal rate again, at least for a while, and to release more serotonin than normal each time."4°
As the Eli Lilly scientists and others put together this picture of fluoxetine's effects on the brain, they speculated as to what part of this process was responsible for the drug's antidepressant properties. Psychiatrists had long observed that antidepressants took two or three weeks to "work," and thus the Eli Lilly researchers reasoned in 1981 that it was the decline in serotonin receptors, which took several weeks to occur, that was "the underlying mechanism associated with the therapeutic response."41 If so, the drug could be
* Over the long term, it appears that serotonin release falls to an abnormally low level, at least in certain regions of the brain.
THE HUNT FOR CHEMICAL IMBALANCES • 81
said to work because it drove the serotonergic system into a less responsive state. But once researchers discovered that fluoxetine partially disabled the feedback mechanism, Claude de Montigny at McGill University argued that this was what allowed the drug to begin working. This disabling process also took two or three weeks to occur, and it allowed the presynaptic neurons to begin pumping higher amounts of serotonin than normal into the synapse. At that point, with fluoxetine continuing to block serotonin's removal, the neurotransmitter could now indeed "pile up" in the synapse, and that would lead "to an enhancement of central serotonergic neurotransmission," de Montigny wrote.42
That is the scientific story of how fluoxetine alters the brain, and it may be that this process helps depressed people get well and stay well. Only the outcomes literature can reveal whether that is so. But the medicine clearly doesn't fix a chemical imbalance in the brain. Instead, it does precisely the opposite. Prior to being medicated, a depressed person has no known chemical imbalance. Fluoxetine then gums up the normal removal of serotonin from the synapse, and that triggers a cascade of changes, and several weeks later the serotonergic pathway is operating in a decidedly abnormal manner. The presynaptic neuron is putting out more serotonin than usual. Its serotonin reuptake channels are blocked by the drug. The system's feedback loop is partially disabled. The postsynaptic neurons are "desensitized" to serotonin. Mechanically speaking, the serotonergic system is now rather mucked up. Eli Lilly's scientists were well aware that this was so. , p81
In 1977, Ray Fuller and David Wong observed that fluoxetine, since it disrupted serotonergic pathways, could be used to study "the role of serotonin neurons in various brain functions—behavior, sleep, regulation of pituitary hormone release, thermoregulation, pain responsiveness and so on." To conduct such experiments, researchers could administer fluoxetine to animals and observe which functions became compromised. They would look for pathologies to appear. This type of research in fact was already being done: Fuller and Wong reported in 1977 that the drug stirred "stereotyped hyperactivity" in rats and "suppressed REM sleep" in both rats and cats.43
82 • ANATOMY OF AN EPIDEMIC
In 1991, in a paper published in the Journal of Clinical Psychiatry, Princeton neuroscientist Barry Jacobs made this very point about SSRIs. He wrote:
These drugs "alter the level of synaptic transmission beyond the physiologic range achieved under [normal] environmental/biological conditions. Thus, any behavioral or physiologic change produced under these conditions might more appropriately be considered pathologic, rather than reflective of the normal biological role of 5-HT [serotonin.] " fn 44
During the 1970s and 1980s, researchers studying the effects of neuroleptics fleshed out a similar story. Thorazine and other standard antipsychotics block 70 to 90 percent of all D2 receptors in the brain. In response, the presynaptic neurons begin pumping out more dopamine and the postsynaptic neurons increase the density of their D2 receptors by 30 percent or more. In this manner, the brain is trying to "compensate" for the drug's effects so that it can maintain the transmission of messages along its dopaminergic pathways. However, after about three weeks, the pathway's feedback mechanism begins to fail, and the presynaptic neurons begin to fire in irregular patterns or turn quiescent. It is this "inactivation" of dopaminergic pathways that "may be the basis for the antipsychotic action," explains the American Psychiatric Association's Textbook of Psychopharmacology. fn 45, p82
Once again, this is a story of neurotransmitter pathways that have been transformed by the medication. After several weeks, their feedback loops are partially disabled, the presynaptic neurons are releasing less dopamine than normal, the drug is thwarting dopamine's effects by blocking D2 receptors, and the postsynaptic neurons have an abnormally high density of these receptors. The drugs do not normalize brain chemistry, but disturb it, and if Jacob's reasoning is followed, to a degree that could be considered "pathological."
THE HUNT FOR CHEMICAL IMBALANCES • 83
A Paradigm for Understanding Psychotropic Drugs
Today, as provost of Harvard University, Steve Hyman is mostly engaged in the many political and administrative tasks that come with leading a large institution. But he is a neuroscientist by training, and in 1996 to 2001, when he was the director of the NIMH, he wrote a paper, one both memorable and provocative in kind, that summed up all that had been learned about psychiatric drugs. Titled "Initiation and Adaptation: A Paradigm for Understanding Psychotropic Drug Action," it was published in the American Journal of Psychiatry, and it told of how all psychotropic drugs could be understood to act on the brain in a common way.'"
Antipsychotics, antidepressants, and other psychotropic drugs, he wrote, "create perturbations in neurotansmitter functions." In response, the brain goes through a series of compensatory adaptations. If a drug blocks a neurotransmitter (as an antipsychotic does), the presynaptic neurons spring into hyper gear and release more of it, and the postsynaptic neurons increase the density of their receptors for that chemical messenger. Conversely, if a drug increases the synaptic levels of a neurotransmitter (as an antidepressant does), it provokes the opposite response: The presynaptic neurons decrease their firing rates and the postsynaptic neurons decrease the density of their receptors for the neurotransmitter. In each instance, the brain is trying to nullify the drug's effects. "These adaptations," Hyman explained, "are rooted in homeostatic mechanisms that exist, presumably, to permit cells to maintain their equilibrium in the face of alterations in the environment or changes in the internal milieu."
However, after a period of time, these compensatory mechanisms break down. The "chronic administration" of the drug then causes "substantial and long-lasting alterations in neural function," Hyman wrote. As part of this long-term adaptation process, there are changes in intracellular signaling pathways and gene expression. After a few weeks, he concluded, the person's brain is functioning in a manner that is "qualitatively as well as quantitatively different from the normal state."
90 • ANATOMY OF AN EPIDEMIC
ple diagnosed with schizophrenia likely fare over time? What chance—if any—would they have of recovering? How well might they fare in society? The same questions can be asked in regard to anxiety, depression, and bipolar illness. What would outcomes look like in the absence of anti-anxiety drugs, antidepressants, and mood stabilizers? Once we have a sense of a baseline for a disorder, we can trace the outcomes literature for that illness, and we can hope that it will tell a consistent, coherent story. Do the drug treatments alter the long-term course of a mental disorder—in the patient population as a whole—for the better? Or for the worse?
Since chlorpromazine (Thorazine) was the drug that launched the psychopharmacology revolution, it seems appropriate to investigate schizophrenia outcomes first.
The Natural History of Schizophrenia
Schizophrenia today is regularly thought of as a lifelong, chronic illness, and that is an understanding that originated with the work of German psychiatrist Emil Kraepelin. In the late 1800s, he systematically tracked the outcomes of patients at an asylum in Estonia, and he observed that there was an identifiable group that reliably deteriorated into dementia. These were patients who, upon entry to the asylum, showed a lack of emotion. Many were catatonic, or lost hopelessly in their own worlds, and they often had gross physical problems. They walked oddly, suffered from facial tics and muscle spasms, and were unable to complete willed physical acts. In his 1899 textbook Lehrbuch der Psychiatrie, Kraepelin wrote that these patients suffered from dementia praecox, and in 1908, Swiss psychiatrist Eugen Bleuler coined the term "schizophrenia" as a substitute diagnostic term for patients in this dilapidated condition.
However, as British historian Mary Boyle convincingly argued in a 1990 article, "Is Schizophrenia What It Was? A Re-analysis of Kraepelin's and Bleuler's Population," many of Kraepelin's dementia praecox patients were undoubtedly suffering from a viral disease, encephalitis lethargica, which in the late 1800s had yet to be
A PARADOX REVEALED • 91
identified. This disease caused people to turn delirious, or to drop into a stupor, or to start walking in a jerky manner, and once Austrian neurologist Constantin von Economo described the illness in 1917, the encephalitis lethargica patients were no longer part of the "schizophrenia" pool, and after that happened, the patient group that remained was quite different from Kraepelin's dementia praecox group. "The inaccessible, the stuporous catatonic, the intellectually deteriorated"—those types of schizophrenia patients, Boyle noted, largely disappeared. As a result, the descriptions of schizophrenia in psychiatric textbooks during the 1920s and 1930s changed. All of the old physical symptoms—the greasy skin, the odd gait, the muscle spasms, the facial tics—disappeared from the diagnostic manuals. What remained were the mental symptoms—the hallucinations, the delusions, and the bizarre thoughts. "The referents of schizophrenia," Boyle wrote, "gradually changed until the diagnosis came to be applied to a pOpulation who bore only a slight, and possibly superficial, resemblance to Kraepelin's."2
So now we have to ask: What is the natural spectrum of outcomes for that group of psychotic patients? Here, unfortunately, we run into a second problem. From 1900 until the end of World War II, eugenic attitudes toward the mentally ill were quite popular in the United States, and that social philosophy dramatically affected their outcomes. Eugenicists argued that the mentally ill needed to be sequestered in hospitals to keep them from having children and spreading their "bad genes." The goal was to keep them confined in asylums, and in 1923, an editorial in the Journal of Heredity concluded, with an air of satisfaction, that "segregation of the insane is fairly complete."3 As a result, many people diagnosed with schizophrenia in the first half of the century were hospitalized and never discharged, but that social policy was then misperceived as outcomes data. The fact that schizophrenics never left the hospital was seen as proof that the disease was a chronic, hopeless illness.
However, after World War II, eugenics fell into disrepute. This was the very "science" that Hitler and Nazi Germany had embraced, and after Albert Deutsch's expose of the abysmal conditions in U.S. mental hospitals, in which he likened them to concentration
camps, many states began talking about treating the mentally ill in
92 • ANATOMY OF AN EPIDEMIC
the community. Social policy changed and discharge rates soared. As a result, there is a brief window of time, from 1946 to 1954, when we can look at how newly diagnosed schizophrenia patients fared and thereby get a sense of the "natural outcomes" of schizo-phrenia prior to the arrival of Thorazine.*
Here's the data. In a study conducted by the NIMH, 62 percent of first-episode psychotic patients admitted to Warren State Hospital in Pennsylvania from 1946 to 1950 were discharged within twelve months. At the end of three years, 73 percent were out of the hospital. fn 4 p 92
A study of 216 schizophrenia patients admitted to Delaware State Hospital from 1948 to 1950 produced similar results. Eighty-five percent were discharged within five years, and on January 1, 1956—six years or more after initial hospitalization- 70 percent were successfully living in the community. fn 5, p92
Meanwhile, Hillside Hospital in Queens, New York, tracked 87 schizophrenia patients discharged in 1950 and determined that slightly more than half never relapsed in the next four years. fn 6 p 92
During this period, outcomes studies in England, where schizophrenia was more narrowly defined, painted a similarly encouraging picture: Thirty-three percent of the patients enjoyed a "complete recovery," and another 20 percent a "social recovery," which meant they could support themselves and live independently. fn 7, p92
These studies provide a rather startling view of schizophrenia outcomes during this time. According to the conventional wisdom, it was Thorazine that made it possible for people with schizophrenia to live in the community. But what we find is that the majority of people admitted for a first episode of schizophrenia during the late 1940s and early 1950s recovered to the point that within the first twelve months, they could return to the community. By the end of three years, that was true for 75 percent of the patients. Only a small percentage-20 percent or so—needed to be continuously hospitalized. Moreover, those returning to the community weren't
* During this period, schizophrenia was a diagnosis being broadly applied to those being hospitalized. Many of these patients would be diagnosed as bipolar or schizoaffective today. Still, this was the diagnosis for the most "seriously disturbed" people in American society at that time.
A PARADOX REVEALED • 93
living in shelters and group homes, as facilities of that sort didn't yet exist. They were not receiving federal disability payments, as the SSI and SSDI programs had yet to be established. Those discharged from hospitals were mostly returning to their families, and judging by the social recovery data, many were working. All in all, there was reason for people diagnosed with schizophrenia during that postwar period to .be optimistic that they could get better and function fairly well in the community.
It is also important to note that the arrival of Thorazine did not improve discharge rates in the 1950s for people newly diagnosed with schizophrenia, nor did its arrival trigger the release of chronic patients. In 1961, the California Department of Mental Hygiene re-ported on discharge rates for all 1,413 first-episode schizophrenia patients hospitalized in 1956, and it found that 88 percent of those who weren't prescribed a neuroleptic were discharged within eighteen months. Those treated with a neuroleptic—about half of the 1,413 patients—had a lower discharge rate; only 74 percent were discharged within eighteen months. This is the only large-scale study from the 1950s that compared discharge rates for first-episode patients treated with. and without drugs, and the investigators concluded that "drug-treated patients tend to have longer periods of hospitalization. . . . The untreated patients consistently show a somewhat lower retention rate." fn 8, p93
The discharge of chronic schizophrenia patients from state mental hospitals—and thus the beginning of deinstitutionalization—got under way in 1965 with the enactment of Medicare and Medicaid. In 1955, there were 267,000 schizophrenia patients in state and county mental hospitals, and eight years later, this number had barely budged. There were still 253,000 schizophrenics residing in the hospitals.' But then the economics of caring for the mentally ill changed. The 1965 Medicare and Medicaid legislation provided federal subsidies for nursing home care but no such subsidy for care in state mental hospitals, and so the states, seeking to save money, naturally began shipping their chronic patients to nursing homes.. That was when the census in state mental hospitals began to noticeably drop, rather than in 1955, when Thorazine was introduced. Unfortunately, our societal belief that it was this medication that
94 • ANATOMY OF AN EPIDEMIC
emptied the asylums, which is so central to the "psychopharma-
cology revolution" narrative, is belied by the hospital census data.
Through a Lens Darkly
In 1955, pharmaceutical companies were not required to prove to the FDA that their new drugs were effective (that requirement was added in 1962), and thus it fell to the NIMH to assess the merits of Thorazine and the other new "wonder drugs" coming to market. Much to its credit, the NIMH organized a conference in September 1956 to "consider carefully the entire psychotropic question," and ultimately the conversation at the conference focused on a very particular question: How could psychiatry adapt, for its own use, a scientific tool that had recently proven its worth in infectious medicine: the placebo-controlled, double-blind, randomized clinical trial ?1°
As many speakers noted, this tool wasn't particularly well suited for assessing outcomes of a psychiatric drug. How could a study of a neuroleptic possibly be "double-blind"? The psychiatrist would quickly see who was on the drug and who was not, and any patient given Thorazine would know he was on a medication as well. Then there was the problem of diagnosis: How would a researcher know if the patients randomized into a trial really had "schizophrenia"? The diagnostic boundaries of mental disorders were forever chang-ing. Equally problematic, what defined a "good outcome" ? Psychiatrists and hospital staff might want to see drug-induced behavioral changes that made the patient "more socially acceptable" but weren't to the "ultimate benefit of the patient," said one conference speaker.11 And how could outcomes be measured? In a study of a drug for a known disease, mortality rates or laboratory results could serve as objective measures of whether a treatment worked. For instance, to test whether a drug for tuberculosis was effective, an X-ray of the lung could show whether the bacillus that caused the disease was gone. What would be the measurable endpoint in a
A PARADOX REVEALED • 95
trial of a drug for schizophrenia? The problem, said NIMH physician Edward Evarts at the conference, was that "the goals of therapy in schizophrenia, short of getting the patient 'well,' have not been clearly defined."12
All of these questions bedeviled psychiatry, and yet the NIMH, in the wake of that conference, made plans to mount a trial of the neuroleptics. The push of history was simply too great. This was the scientific method now used in internal medicine to assess the merits of a therapy, and Congress had created the NIMH with the thought that it would transform psychiatry into a more modern, scientific discipline. Psychiatry's adoption of this tool would prove that it was moving toward that goal. The NIMH established a Psychopharmacology Service Center to head up this effort, and Jonathan Cole, a psychiatrist from the National Research Council, was named its director.
Over the next couple of years, Cole and the rest of psychiatry settled on a trial design for testing psychotropic drugs. Psychiatrists and nurses would use "rating scales" to measure numerically the characteristic symptoms of the disease that was to be studied. Did a drug for schizophrenia reduce the patient's "anxiety"? His or her "grandiosity"? "Hostility"? "Suspiciousness" ? "Unusual thought content"? "Uncooperativeness"? The severity of all of those symptoms would be measured on a numerical scale and a total "symptom" score tabulated, and a drug would be deemed effective if it reduced the total score significantly more than a placebo did within a six-week period.
At least in theory, psychiatry now had a way to conduct trials of psychiatric drugs that would produce an "objective" result. Yet the adoption of this assessment put psychiatry on a very particular path: The field would now see short-term reduction of symptoms as evidence of a drug's efficacy. Much as a physician in internal medicine would prescribe an antibiotic for a bacterial infection, a psychiatrist would prescribe a pill that knocked down a "target symptom" of a "discrete disease." The six-week "clinical trial" would prove that this was the right thing to do. However, this tool wouldn't provide any insight into how patients were faring over the long term.
96 • ANATOMY OF AN EPIDEMIC
Were they able to work? Were they enjoying life? Did they have friends? Were they getting married? None of those questions would be answered.
This was the moment that magic-bullet medicine shaped psychiatry's future. The use of the clinical trial would cause psychiatrists to see their therapies through a very particular prism, and even at the 1956 conference, New York State Psychiatric Institute researcher Joseph Zubin. warned that when it came to evaluating a therapy for a psychiatric disorder, a six-week study induced a kind of scientific myopia. "It would be foolhardy to claim a definite advantage for a specified therapy without a two- to five-year follow-up," he said. "A two-year follow-up would seem to be the very minimum for the long-term effects.""
The Case for Neuroleptics
The Psychopharmacology Service Center launched its nine-hospital trial of neuroleptics in 1961, and this is the study that marks the beginning of the scientific record that serves today as the "evidence base" for these drugs. In the six-week trial, 270 patients were given Thorazine or another neuroleptic (which were also known as "phenothiazines,") while the remaining 74 were put on a placebo. The neuroleptics did help reduce some target symptoms—unrealistic thinking, anxiety, suspiciousness, auditory hallucinations, etc.—better than the placebo, and thus, according to the rating's scales cumulative score, they were effective. Furthermore, the psychiatrists in the study judged 75 percent of the drug-treated patients to be "much improved" or "very much improved," versus 23 percent of the placebo patients.
After that, hundreds of smaller trials produced similar results, and thus the evidence that these drugs reduce symptoms over the short term better than placebo is fairly robust.* In 1977, Ross Baldessarini
* In 2007, the Cochrane Collaboration, an international group of scientists
that doesn't take funding from pharmaceutical companies, raised questions
A PARADOX REVEALED • 97
at Harvard Medical School reviewed 149 such trials and found that the antipsychotic drug proved superior to a placebo in 83 percent of them.14 The "Brief Psychiatric Rating Scale" (BPRS) was regularly employed in such trials, and the American Psychiatric Association eventually decided that a 20 percent reduction in total BPRS score represented a clinically significant response to a drug.15 Based on this measurement, an estimated 70 percent of all schizophrenia patients suffering from an acute episode of psychosis "respond," over a six-week period, to an antipsychotic medication.
Once the NIMH investigators determined that the antipsychotics were efficacious over the short term, they naturally wanted to know how long schizophrenia patients should stay on the medication. To investigate this question, they ran studies that, for the most part, had this design: Patients who were good responders to the medication were either maintained on the drug or abruptly withdrawn from it. In 1995, Patricia Gilbert at the University of California at San Diego reviewed sixty-six relapse studies, involving 4,365 patients, and she found that 53 percent of the drug-withdrawn patients relapsed within ten months versus 16 percent of those maintained on the medications. "The efficacy of these medications in reducing the risk of psychotic relapse has been well documented," she concluded." 16
This is the scientific evidence that supports the use of anti-psychotic medications for schizophrenia, both in the hospital and long-term. As John Geddes, a prominent British researcher, wrote in
about this short-term efficacy record. They conducted a meta-analysis of all chlorpromazine-versus-placebo studies in the scientific literature, and after identifying fifty of decent quality, they concluded that the advantage of drug over placebo was smaller than commonly thought. They calculated that seven patients had to be treated with chlorpromazine to produce a net gain of one "global improvement," and that "even this finding may be an overestimate of the positive and an understimate of the negative effects of giving chlorpromazine." The Cochrane investigators, somewhat startled by their results, wrote that "reliable evidence about [chlorpromazine's] short-term efficacy is' surprisingly weak."
* There is an evident flaw with Gilbert's meta-analysis. She didn't determine
whether the speed with which drugs were withdrawn affected the relapse rate.
98 • ANATOMY OF AN EPIDEMIC
a 2002 article in the New England Journal of Medicine, "Anti-psychotic drugs are effective in treating acute psychotic symptoms and preventing relapse."17 Still, as many investigators have noted, there is a hole in this evidence base, and it's the very hole that Zubin predicted would arise. "Little can be said about the efficacy and effectiveness of conventional antipsychotics on nonclinical outcomes," confessed Lisa Dixon and other psychiatrists at the University of Maryland School of Medicine in 1995. "Well-designed long-term studies are virtually nonexistent, so the longitUdinal impact of treatment with conventional antipsychotics is unclear."18
This doubt prompted an extraordinary 2002 editorial in European Psychiatry, penned by Emmanuel Stip, a professor of psychiatry at the Universite de Montreal. "After fifty years of neuroleptics, are we able to answer the following simple question: Are neuroleptics effective in treating schizophrenia?" There was, he said, "no compelling evidence on the matter, when `long-term' is considered."19
A Conundrum Appears
Although Dixon's and Stip's comments suggest that there is no longterm data to be reviewed, it is in fact possible to piece together a story of how antipsychotics alter the course of schizophrenia, and this story begins, quite appropriately, with the NIMH's follow-up study of the 344 patients in its initial nine-hospital trial. In some ways, the patients—regardless of what treatment they had received in the hospital—were not faring so badly. At the end of one year,
After her study appeared, Adele Viguera at Harvard Medical School reanalyzed the same sixty-six studies and determined that when the drugs were gradually withdrawn, the relapse rate was only one-third as high as in the abrupt-withdrawal studies. The abrupt-withdrawal design in the majority of the relapse studies dramatically increased the risk that the schizophrenia patients would become sick again. Indeed, the relapse rate for gradually withdrawn patients was similar to what it was for the drug-maintained patients.
A PARADOX REVEALED • 99
254 were living in the community, and 58 percent of those who—according to their age and gender—could be expected to work were in fact employed. Two-thirds of the "housewives" were functioning OK in that domestic role. Although the researchers didn't report on the medication use of patients during the one-year follow-up, they were startled to discover that "patients who received placebo treatment [in the six-week trial] were less likely to be rehospitalized than those who received any of the three active phenothiazines." fn 20
Here, at this very first moment in the scientific literature, there is the hint of a paradox: While the drugs were effective over the short term, perhaps they made people more vulnerable to psychosis over the long term, and thus the higher rehospitalization rates for drug-treated patients at the end of one year. Soon, NIMH investigators were back with another surprising result. In two drug withdrawal trials, both of which included patients who weren't on any drug at the start of the study, relapse rates rose in correlation with drug dosage. Only 7 percent of those who had been on a placebo at the start of the study replapsed, compared to 65 percent of those taking more than five hundred milligrams of chlorpromazine before the drug was withdrawn. "Relapse was found to be significantly related to the dose of the tranquilizing medication the patient was receiving before he was put on placebo--the higher the dose, the greater the probability of relapse," the researchers wrote. fn 21, p 99.
Something was amiss, and clinical observations deepened the suspicion. Schizophrenia patients discharged on medications were returning to psychiatric emergency rooms in such droves that hospital staff dubbed it the "revolving door syndrome." Even when patients reliably took their medications, relapse was common, and researchers observed that "relapse is greater in severity during drug administration than when no drugs are given." fn 22
At the same time, if patients relapsed after quitting the medications, Cole noted, their psychotic symptoms tended to "persist and intensify," and, at least for a time, they suffered from a host of new symptoms as well: nausea, vomiting, diarrhea, agitation, insomnia, headaches, and weird motor tics.23 Initial exposure to a neuroleptic seemed to be setting patients up for a future of severe psychotic episodes, and that was true regardless of whether they stayed on the medications.
.roo • ANATOMY OF AN EPIDEMIC
These poor results prompted two psychiatrists at Boston Psychopathic Hospital, J. Sanbourne Bockoven and Harry Solomon, to revisit the past. They had been at the hospital for decades, and in the period after World War II ended, when they treated psychotic patients with a progressive form of psychological care, they had seen the majority regularly improve. That led them to believe that "the majority of mental illnesses, especially the most severe, are largely self-limiting in nature if the patient is not subjected to a demeaning experience or loss of rights and liberties." The anti-psychotics, they reasoned, should speed up this natural healing process. But were the drugs improving long-term outcomes? In a retrospective study, they found that 45 percent of the patients treated in 1947 at their hospital hadn't relapsed in the next five years and that 76 percent were successfully living in the community at the end of that follow-up period. In contrast, only 31 percent of the patients treated at the hospital in 1967 with neuroleptics remained relapse-free for five years, and as a group they were much more "socially dependent"—on welfare and needing other forms of support. "Rather unexpectedly, these data suggest that psychotropic drugs may not be indispensable," Bockoven and Solomon wrote. "Their extended use in aftercare may prolong the social dependency of many discharged patients."24
With debate over the merits of neuroleptics rising, the NIMH funded three studies during the 1970s that reexamined whether schizophrenia patients—and in particular those suffering a first episode of schizophrenia—could be successfully treated without medications. In the first study, which was conducted by William Carpenter and Thomas McGlashan at the NIMH's clinical research facility in Bethesda, Maryland, those treated without drugs were discharged sooner than the drug-treated patients, and only 35 percent of the nonmedicated group relapsed within a year after discharge, compared to 45 percent of the medicated group. The off-drug patients also suffered less from depression, blunted emotions, and retarded movements. Indeed, they told Carpenter and McGlashan that they had found it "gratifying and informative" to have gone through their psychotic episodes without having their feelings numbed by the drugs. Medicated patients didn't have that
A PARADOX REVEALED • 101
same learning experience, and as a result, Carpenter and McGlashan concluded, over the long term they "are less able to cope with subsequent life stresses."25
A year later, Maurice Rappaport at the University of California in San Francisco announced results that told the same story, only more strongly so. He had randomized eighty young newly diagnosed male schizophrenics admitted to Agnews State Hospital into drug and non-drug groups, and although symptoms abated more quickly in those treated with antipsychotics, both groups, on average, stayed only six weeks in the hospital. Rappaport followed the patients for three years, and it was those who weren't treated with antipsychotics in the hospital and who stayed off the drugs after discharge that had—by far—the best outcomes. Only two of the twenty-four patients in this never-exposed-to-antipsychotics group relapsed during the three-year follow-up. Meanwhile, the patients that arguably fared the worst were those on drugs throughout the study. The very standard of care that, according to psychiatry's "evidence base," was supposed to produce the best outcomes had instead produced the worst.
"Our findings suggest that antipsychotic medication is not the treatment of choice, at least for certain patients, if one is interested in long-term clinical improvement," Rappaport wrote. "Many unmedicated-while-in-hospital patients showed greater long-term improvement, less pathology at follow-up, fewer hospitalizations, and better overall functioning in the community thatn patients who were given chlorpromazine while in the hospital. fn 26, p102
Rappaport's Study:Three-Year Schizophrenia Outcomes
Medication Use (In hospital/ after discharge) Number of Patients Severity Illness Scale (1=best outcome; 7=worst outcome) Rehospitalization
Placebo/off 24 1.70 8%
Antipsychotic/off 17 2.79 47%
Placebo/on 17 3.54 53%
Antipsychotic/on 22 3.51 73%
In this study, patients were grouped according to both their in-hospital care (placebo or drug) and whether they used antipsychotics after they were discharged. Thus, 24 of the 41 patients treated with placebo in the hospital remained off the drugs during the follow-up period. This never-exposed group had the best outcomes by far. Rappaport, M. "Are there schizophrenics for whom drugs may be unnecessary or contraindicated!' International Pharmacopsychiatry 13 (1978): 100-11.
104 • ANATOMY OF AN EPIDEMIC
antipsychotic medication may make some schizophrenic patients more vulnerable to future relapse than would be the case in the natural course of the illness.29
And if that was so, these drugs were increasing the likelihood that a person who suffered a psychotic break would become chronically ill.
A Cure Worse Than the Disease?
All drugs have a risk-benefit profile, and the usual thought within medicine is that a drug should provide a benefit that outweighs the risks. A drug that curbs psychotic symptoms clearly provides a marked benefit, and that was why antipsychotics could be viewed as helpful even though the list of negatives with these drugs was a long one. Thorazine and other first-generation neuroleptics caused Parkinsonian symptoms and extraordinarily painful muscle spasms. Patients regularly complained that the drugs turned them into emo-tional "zombies." In 1972, researchers concluded that neuroleptics "impaired learning."30 Others reported that even if medicated patients stayed out of the hospital, they seemed totally unmotivated and socially disengaged. Many lived in "virtual solitude" in group homes, spending most of the time "staring vacantly at television," wrote one investigator.31 None of this told of medicated schizophrenia patients faring well, and here was the quandary that psychiatry now faced: If the drugs increased relapse rates over the long term, then where was the benefit? This question was made all the more pressing by the fact that many patients maintained on the drugs were developing tardive dyskinesia (TD), a gross motor dysfunction that remained even after the drugs were withdrawn, evidence of permanent brain damage.
All of this required psychiatry to recalculate the risks and benefits of antipsychotics, and in 1977 Jonathan Cole did so in an article provocatively titled "Is the Cure Worse Than the Disease?" He reviewed all of the long-term harm the drugs could cause and observed that studies had shown that at least 50 percent of all schizophrenia patients could fare well without the drugs. There was only one moral thing for psychiatry to do: "Every schizophrenic outpatient maintained on antipsychotic medication should have the benefit of an adequate trial without drugs." This, he explained, would save many "from the dangers of tardive dyskinesia as well as the financial and social burdens of prolonged drug therapy." fn 32
The evidence base for maintaining schizophrenia patients on antipsychotics had collapsed. "Are the antipsychotics to be withdrawn?" asked Pierre Deniker, the French psychiatrist who, in the early 1950s, had first promoted their use.33
Supersensitivity Psychosis
In the late 1970s, two physicians at McGill University, Guy Chouinard and Barry Jones, stepped forward with a biological explanation for why the drugs made schizophrenia patients more biologically vulnerable to psychosis. Their understanding arose, in large part, from the investigations into the dopamine hypothesis of schizophrenia, which had detailed how the drugs perturbed this neurotransmitter system.
Thorazine and other standard antipsychotics block 70 to 90 percent of all D2 receptors in the brain. In an effort to compensate for this blockade, the postsynaptic neurons increase the density of their D2 receptors by 30 percent or more. The brain is now "supersensitive" to dopamine, Chouinard and Jones explained, and this neurotransmitter is thought to be a mediator of psychosis. "Neuroleptics can produce a dopamine supersensitivity that leads to both dyskinetic and psychotic symptoms," they wrote. "An implication is that the tendency toward psychotic relapse in a patient who has developed such a supersensitivity is determined by more than just the normal course of the illness."34
A simple metaphor can help us better understand this drug-induced biological vulnerability to psychosis and why it flares up when the drug is withdrawn. Neuroleptics put a brake on dopamine transmission, and in response the brain puts down the dopamine accelerator (the extra D2 receptors). If the drug is abruptly withdrawn, the brake on dopamine is suddenly released while the accelerator is still pressed to the floor. The system is now wildly out of balance, and just as a car might careen out of control, so too the dopaminergic pathways in the brain. The dopaminergic neurons in the basal ganglia may fire so rapidly that the patient withdrawing from the drugs suffers weird tics, agitation, and other motor abnormalities. The same out-of-control firing is happening with the dopaminergic pathway to the limbic region, and that may lead to "psychotic relapse or deterioration," Chouinard and Jones wrote. fn 35
This was an extraordinary piece of scientific detective work by the two Canadian investigators. They had—at least in theory—identified the reason that relapse rates were so high in the medication-withdrawal trials, which psychiatry had mistakenly interpreted as proving that the drugs prevented relapse. The severe relapse suffered by many patients withdrawn from antipsychotics was not necessarily the result of the "disease" returning, but rather was drug-related. Chouinard and Jones's work also revealed that both psychiatrists and their patients would regularly suffer from a clinical delusion: They would see the return of psychotic symptoms upon drug withdrawal as proof that the antipsychotic was necessary and that it "worked." The relapsed patient would then go back on the drug and often the psychosis would abate, which would be further proof that it worked. Both doctor and patient would experience this to be "true," and yet, in fact, the reason that the psychosis abated with the return of the drug was that the brake on dopamine transmission was being reapplied, which countered the stuck dopamine accelerator. As Chouinard and Jones explained: "The need for continued neuroleptic treatment may itself be drug-induced."
In short, initial exposure to neuroleptics put patients onto a path where they would likely need the drugs for life. Yet—and this was the second haunting aspect to this story of medicine—staying on the drugs regularly led to a bad end. Over time, Chouinard and Jones noted, the dopaminergic pathways tended to become permanently dysfunctional. They became irreversibly stuck in a hyperactive state,
A PARADOX REVEALED • 107
and soon the patient's tongue was slipping rhythmically in and out of his mouth (tardive dyskinesia) and psychotic symptoms were worsening (tardive psychosis). Doctors would then need to prescribe higher doses of antipsychotics to tamp down those tardive symptoms. "The most efficacious treatment is the causative agent itself, the neuroleptic," Chouinard and Jones said.
Over the next few years, Chouinard and Jones continued to flesh out and test their hypothesis. In 1982, they reported that 30 percent of 216 schizophrenia outpatients they studied showed signs of tar-dive psychosis.36 They also observed that it tended to afflict those patients who, at initial diagnosis, had a "good prognosis," and thus would have had a chance to fare well over the long term if they had never been exposed to neuroleptics. These were the "placebo responders" who had fared best in the studies conducted by Rappaport and Mosher, and now Chouinard and Jones were reporting that they were becoming chronically psychotic after years of taking antipsychotics. Finally, Chouinard quantified the risk, reporting that tardive psychosis seemed to develop at a slightly slower rate than tardive dyskinesia. It afflicted 3 percent of patients a year, with the result that after fifteen years on the drugs, perhaps 45 percent suffered from it. When tardive psychosis sets in, Chouinard added, "the illness appears worse" than ever before. "New schizophrenic or original symptoms of greater severity will appear."37
Animal studies confirmed this picture too. Philip Seeman reported that antipsychotics caused an increase in D2 receptors in rats, and while the density of these receptors could revert to normal if the drug was withdrawn (he reported that for every month of exposure, it took two months for renormalization to occur), at some point the increase in receptors became irreversible. fn 38
In 1984, Swedish physician Lars Martensson, in a presentation at the World Federation of Mental Health Conference in Copenhagen, summed up the devastating bottom line. "The use of neuroleptics is a trap," he said. "It is like having a psychosis-inducing agent built into the brain."39
io8 • ANATOMY OF AN EPIDEMIC
A Crazy Idea . . . Or Not?
This was the view of neuroleptics that came together in the early 1980s, and it was a story of science at its best. Psychiatrists saw that the drugs "worked." They saw that antipsychotics knocked down psychotic symptoms, and they observed that patients who stopped taking their medications regularly became psychotic again. Scientific tests reinforced their clinical perceptions. Six-week trials proved the drugs were effective. Relapse studies proved that patients should be maintained on the drugs. Yet once researchers came to understand how the drugs acted on the brain, and once they began investigating why patients were developing tardive dyskinesia and why they were becoming so chronically ill, then this counterintuitive picture of the drugs—that they were increasing the likelihood that patients would become chronically ill—emerged. It was Chouinard and Jones who explicitly connected all the dots, and for a time, their work did stir up a hornet's nest within psychiatry. One physician, at a meeting where the two McGill University doctors spoke, asked in astonishment: "I put my patients on neuroleptics because they're psychotic. Now you're saying that the same drug that controls their schizophrenia also causes a psychosis?" fn 40
But what was psychiatry supposed to do with this information? It clearly imperiled the field's very foundation. Could it really now confess to the public, or even admit to itself, that the very class of drugs said to have "revolutionized" the care of the mentally ill was in fact making patients chronically ill? That antipsychotics made patients—at least in the aggregate—more psychotic over time? Psychiatry desperately needed this discussion to go away. Soon the articles by Chouinard and Jones on "supersensitivity psychosis" were filed away in the "interesting hypothesis" category, and everyone in the field breathed a sigh of relief when Solomon Snyder, who knew as much about dopamine receptors as any scientist in the world, assured everyone in his 1986 book Drugs and the Brain that it had all turned out to be a false alarm. "If dopamine receptor sensitivity is greater in patients with tardive dyskinesia, one might wonder whether they would also suffer a corresponding increase in schizo-
A PARADOX REVEALED • 109
phrenia symptoms. Interestingly, though researchers have looked carefully for any possible exacerbation of schizophrenic symptoms in patients who begin to develop tardive dyskinesia, none has ever been found."41
That moment of crisis within psychiatry, when it briefly worried about supersensitivity psychosis, occurred nearly thirty years ago, and today the notion that antipsychotics increase the likelihood that a person diagnosed with schizophrenia will become chronically ill seems, on the face of it, absurd. Ask psychiatrists at top medical schools, staff at a mental hospital, NIMH officials, leaders of the National Alliance for the Mentally Ill, science writers at major newspapers, or the ordinary person in the street, and everyone will attest that antipsychotics are essential for treating schizophrenia, the very cornerstone of care, and that anyone who touts a different idea is, well, a bit loony. Still, we started down this path of research, I've invited readers into this loony bin, and so now we need to move up one floor in the Countway Library. The volumes in the basement end in 1986, and now we need to comb the scientific literature since that date, and see what story it has to tell. Was it all a false alarm . . . or not?
The most efficient way to answer that question is to summarize, one by one, the relevant studies and avenues of research.
The Vermont longitudinal study
In the late 1950s and early 1960s, Vermont State Hospital discharged 269 chronic schizophrenics, most of whom were middle-aged, into the community. Twenty years later, Courtenay Harding interviewed 168 patients from this cohort (those who were still alive), and found that 34 percent were recovered, which meant they were "asymptomatic and living independently, had close relationships, were employed or otherwise productive citizens, were able to care for themselves, and led full lives in general."42 This was a startling good long-term outcome for patients who had been seen as hopeless in the 1950s, and those who had recovered, Harding told the APA Monitor, had one thing in common: They all "had long since stopped taking medications. " fn 43 She concluded that it was a "myth" that schizophrenia patients "must be on medication all their lives," and that, in fact, "it may be a small percentage who need medication indefinitely." fn 44
The World Health Organization cross-cultural studies
In 1969, the World Health Organization launched an effort to track schizophrenia outcomes in nine countries. At the end of five years, the patients in the three "developing" countries—India, Nigeria, and Colombia—had a "considerably better course and outcome" than patients in the United States and five other "developed countries." They were much more likely to be asymptomatic during the follow-up period, and even more important, they enjoyed "an exceptionally good social outcome."
These findings stung the psychiatric community in the United States and Europe, which protested that there must have been a design flaw in the study. Perhaps the patients in India, Nigeria, and Colombia had not really been schizophrenic. In response, WHO launched a ten-country study in 1978, and this time they primarily enrolled patients suffering from a first episode of schizophrenia, all of whom were diagnosed by Western criteria. Once again, the results were much the same. At the end of two years, nearly two-thirds of the patients in the "developing countries" had had good outcomes, and slightly more than one-third had become chronically ill. In the rich countries, only 37 percent of the patients had good outcomes, and 59 percent became chronically ill. "The findings of a better outcome of patients in developing countries was confirmed," the WHO scientists wrote. "Being in a developed country was a strong predictor of not attaining a complete remission." fn 45
Although the WHO investigators didn't identify a reason for the stark disparity in outcomes, they had tracked antipsychotic usage in the second study, having hypothesized that perhaps patients in the poor countries fared better because they more reliably took their medication. However, they found the opposite to be true. Only 16 percent of the patients in the poor countries were regularly maintained on antipsychotics, versus 61 percent of the patients in the rich countries. Moreover, in Agra, India, where patients arguably fared the best, only 3 percent of the patients were kept on an
antipsychotic. Medication usage was highest in Moscow, and that
city had the highest percentage of patients who were constantly ill. fn 46
In this cross-cultural study, the best outcomes were clearly associated with low medication use. Later, in 1997, WHO researchers interviewed the patients from the first two studies once again (fifteen to twenty-five years after the initial studies), and they found that those in the poor countries continued to do much better. The "outcome differential" held up for "general clinical state, symptomatology, disability, and social functioning." In the developing countries, 53 percent of the schizophrenia patients were simply "never psy-chotic" anymore, and 73 percent were employed.47 Although the WHO investigators didn't report on medication usage in their follow-up study, the bottom line is clear: In countries where patients hadn't been regularly maintained on antipsychotics earlier in their illness, the majority had recovered and were doing well fifteen years later.
Tardive dyskinesia and global decline
Tardive dyskinesia and tardive psychosis occur because the dopaminergic pathways to the basal ganglia and limbic system be come dysfunctional. But there are three dopaminergic pathways, and so it stands to reason that the third one, which transmits messages to the frontal lobes, also becomes dysfunctional over time. If so, researchers could expect to find a global decline in brain function in patients diagnosed with tardive dyskinesia, and from 1979 to 2000, more than two dozen studies found that to be the case. "The relationship appears to be linear," reported Medical College of Virginia psychiatrist James Wade in 1987. "Individuals with severe forms of the disorder are most impaired cognitively."48 Researchers determined that tardive dyskinesia was associated with a worsening of the negative symptoms of schizophrenia (emotional disengagement); psychosocial impairment; and a decline in memory, visual retention, and the capacity to learn. People with TD lose their "road map of consciousness," concluded one investigator." Investigators have dubbed this long-term cognitive deterioration tardive
112 • ANATOMY OF AN EPIDEMIC
dementia; in 1994, researchers found that three-fourths of medicated schizophrenia patients seventy years and older suffer from a brain pathology associated with Alzheimer's disease.s°
MRI studies
The invention of magnetic resonance imaging technology provided researchers with the opportunity to measure volumes of brain structures in people diagnosed with schizophrenia, and while they hoped to identify abnormalities that might characterize the illness, they ended up documenting instead the effect of antipsychotics on brain volumes. In a series of studies from 1994 to 1998, investigators reported that the drugs caused basal ganglion structures and the thalamus to swell, and the frontal lobes to shrink, with these changes in volumes "dose related." fn 51 Then, in 1998, Raquel Gur at the University of Pennsylvania Medical Center reported that the swelling of the basal ganglia and thalamus was "associated with greater severity of both negative and positive symptoms." fn 52
This last study provided a very clear picture of an iatrogenic process. The antipsychotic causes a change in brain volumes, and as this occurs, the patient becomes more psychotic (known as the "positive symptoms" of schizophrenia) and more emotionally disengaged ("negative symptoms"). The MRI studies showed that antipsychotics worsen the very symptoms they are supposed to treat, and that this worsening begins to occur during the first three years that patients are on the drugs.
Modeling psychosis
As part of their investigations of schizophrenia, researchers have sought to develop biological "models" of psychosis, and one way they have done that is to study the brain changes induced by various drugs—amphetamines, angel dust, etc.—that can trigger delusions and hallucinations. They also have developed ways to induce psychotic-like behaviors in rats and other animals. Lesions to the hippocampus can cause such disturbed behaviors; certain genes can be "knocked out" to produce such symptoms.
In 2005, Philip Seeman reported that all of these psychotic triggers cause an increase in D2 receptors in the brain that have a "HIGH affinity" for dopamine, and by that, he meant that the receptors bound quite easily with the neurotransmitter. These "results imply that there may be many pathways to psychosis, including multiple gene mutations, drug abuse, or brain injury, all of which may converge via D2 HIGH to elicit psychotic symptoms," he wrote." fn 53 Seeman reasoned that this is why antipsychotics work: They block D2 receptors. But in his research, he also found that these drugs, including the newer ones like Zyprexa and Risperdal, double the density of "high affinity" D2 receptors. They induce the same abnormality that angel dust does, and thus this research confirms what Lars Martensson observed in 1984: Taking a neuroleptic is like having a "psychosis inducing agent built into the brain."
Nancy Andreasen's longitudinal MRI study
In 1989, Nancy Andreasen, a psychiatry professor at the University of Iowa who was editor in chief of the American Journal of Psychiatry from 1993 to 2005, began a long-term study of more than five hundred schizophrenia patients. In 2003, she reported that at the time of initial diagnosis, the patients had slightly smaller frontal lobes than normal, and that over the next three years, their frontal lobes continued to shrink. Furthermore, this "progressive reduction in frontal lobe white matter volume" was associated with a worsen-ing of negative symptoms and functional impairment, and thus Andreasen concluded that this shrinkage is evidence that schizophrenia is a "progressive neurodevelopmental disorder," one which antipsychotics unfortunately fail to arrest. "The medications currently used cannot modify an injurious process occurring in the brain, which is the underlying basis of symptoms."'"
Hers was a picture of antipsychotics as therapeutically ineffective, rather than harmful, and two years later, she fleshed out this picture. Her patients' cognitive abilities began to "worsen significantly" five years after initial diagnosis, a decline tied to the "progressive brain volume reductions after illness onset."55 In other words, as her patients' frontal lobes shrank in size, their ability
114 • ANATOMY OF AN EPIDEMIC
to think declined.
But other researchers conducting MRI studies had found that the shrinkage of the frontal lobes was drug-related, and in a 2008 interview with the New York Times, Andreasen conceded that the "more drugs you've been given, the more brain tissue you lose." The shrinkage of the frontal lobes may be part of a disease process, which the drugs then exacerbate. "What exactly do these drugs do?" Andreasen said. "They block basal ganglia activity. The prefrontal cortex doesn't get the input it needs and is being shut down by drugs. That reduces the psychotic symptoms. It also causes the prefrontal cortex to slowly atrophy." fn 56 Once again, Andreasen's investigations revealed an iatrogenic process at work. The drugs block dopamine activity in the brain and this leads to brain shrinkage, which in turn correlates with a worsening of negative symptoms and cognitive impairment.
This was yet another disturbing finding, and it prompted Yale psychiatrist Thomas McGlashan, who three decades earlier had wondered whether antipsychotics were making patients "more biologically vulnerable to psychosis," to once again question this entire paradigm of care. He put his troubled thoughts into a scientific context:
“In the short term, acute D2 [receptor] blockade detaches salience and the patient's investment in positive symptoms. In the long term, chronic D2 blockade dampens salience for all events in everyday life, inducing a chemical anhedonia that is sometimes labeled postpsychotic depression or neuroleptic dysphoria. . . . Do we free patients from the asylum with D2 blocking agents only to block incentive, engagement with the world, and the joie de vivre of everyday life? Medication can be lifesaving in a crisis, but it may render the patient more psychosis-prone should it be stopped and more deficit-ridden should it be maintained.” fn 57
I attended the 2008 meeting of the American Psychiatric Association for a number of reasons, but the person I most wanted to hear speak was Martin Harrow, who is a psychologist at the University of Illinois College of Medicine. From 1975 to 1983, he enrolled sixty-four young schizophrenics in a long-term study funded by the NIMH, recruiting the patients from two Chicago hospitals. One was private and the other public, as this ensured that the group would be economically diverse. p115
Ever since then, he has been periodically assessing how well they are doing. Are they symptomatic? In recovery? Employed? Do they take antipsychotic medications? His results provide an up-to-date look at how schizophrenia patients in the United States are faring, and thus his study can bring our investigation of the scientific literature to a fitting climax. If the conventional wisdom is to be believed, then those who stayed on antipsychotics should have had better outcomes. If the scientific literature we have just reviewed is to be believed, then it should be the reverse.
Here is Harrow's data. In 2007, he published a report on the patients' fifteen-year outcomes in the Journal of Nervous and Mental Disease, and he further updated that review in his presentation at the APA's 2008 meeting. fn 58 At the end of two years, the group not on antipsychotics were doing slightly better on a "global assessment scale" than the group on the drugs. Then, over the next thirty months, the collective fates of the two groups began to dramatically diverge. The off-med group began to improve significantly, and by the end of 4.5 years, 39 percent were "in recovery" and more than 60 percent were working. In contrast, outcomes for the medication group worsened during this thirty-month period. As a group, their global functioning declined slightly, and at the 4.5-year mark, only 6 percent were in recovery and few were working. That stark divergence in outcomes remained for the next ten years. At the fifteen year follow-up, 40 percent of those off drugs were in recovery, more than half were working, and only 28 percent suffered from psychotic symptoms. In contrast, only 5 percent of those taking anti-
6 • ANATOMY OF AN EPIDEMIC
Long-term Recovery Rates for Schizophrenia Patients
Source: Harrow, M. "Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications!' The Journal of Nervous and Mental Disease, 195 (2007): 406-14.
Journal of Nervous & Mental Disease:
May 2007 - Volume 195 - Issue 5 - pp 406-414
doi: 10.1097/01.nmd.0000253783.32338.6e
Original Article
psychotics were in recovery, and 64 percent were actively psychotic. "I conclude that patients with schizophrenia not on antipsychotic medication for a long period of time have significantly better global functioning than those on antipsychotics," Harrow told the APA audience.
Indeed, it wasn't just that there were more recoveries in the unmedicated group. There were also fewer terrible outcomes in this group. There was a shift in the entire spectrum of outcomes. Ten of the twenty-five patients who stopped taking antipsychotics recovered, eleven had so-so outcomes, and only four (16 percent) had a "uniformly poor outcome." In contrast, only two of the thirty-nine patients who stayed on antipsychotics recovered, eighteen had so-so outcomes, and nineteen (49 percent) fell into the "uniformly poor" camp. Medicated patients had one-eighth the recovery rate of unmedicated patients, and a threefold higher rate of faring miserably over the long term.
This is the outcomes picture revealed in an NIMH-funded study,
A PARADOX REVEALED • 117
The spectrum of outcomes for medicated versus unmedicated patients. Those on antipsychotics had a much lower recovery rate, and were much more likely to have a "uniformly poor" outcome. Source: Harrow, M."Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications:' The Journal of Nervous and Mental Disease, 195 (2007): 406-14.
the most up-to-date one we have today. It also provides us with insight into how long it takes for the better outcomes for nonmedicated patients, as a group, to become apparent. Although this difference began to show up at the end of two years, it wasn't until the 4.5-year mark that it became evident that the nonmedicated group, as a whole, was doing much better. Furthermore, through his rigorous tracking of patients, Harrow discovered why psychiatrists remain blind to this fact. Those who got off their antipsychotic medications left the system, he said. They stopped going to day programs, they stopped seeing therapists, they stopped telling people they had ever been diagnosed with schizophrenia, and they disappeared into society. A few of the nonmedicated people in Harrow's study even got "high-level jobs"—one became a college professor and another a lawyer—and several had "mid-level jobs." Explained Harrow: "We [clinicians] get our experience from seeing those who leave us, and then come back because they relapse. We don't see the ones who don't relapse. They don't come back. They are quite happy."
Afterward, I asked Dr. Harrow why he thought the nonmedicated patients did so much better. He did not attribute it to their being off antipsychotics, but rather said it was because this group "had a stronger internal sense of self," and once they initially stabilized on the medications, this "better personhood" gave them the
50%
45% 40% 35% 30% 25% • 20% Off Antipsychotics
15% 10% 5% 0% On Antipsychotics
2 4.5 7.5 10 15
Year Year Year Year Year
Follow-up Follow-up Follow-up Follow-up Follow-up
Spectrum of Outcomes in Schizophrenia Patients
• ANATOMY OF AN EPIDEMIC
confidence to go off the drugs. "It's not that those who went off medications did better, but rather it was those who did better [initially] who then went off the medications." When I pressed on with a question about whether his findings supported a different inter-pretation, which was that the drugs worsened long-term outcomes, he grew a bit testy. "That's a possibility, but I'm not advocating it," he said. "People recognize there may be side effects. . . . I'm not just trying to avoid the question. I'm one of the few people in the field without drug money."
I asked one last question. At the very least, shouldn't his findings be worked into the paradigm of care used in our society to treat those diagnosed with schizophrenia? "There is no question about that," he replied. "Our data is overwhelming that not all schizophrenic patients need to be on antipsychotics all their lives."
Reviewing the Evidence
We have followed a trail of documents to a surprising end, and thus I think we need to ask one final question: Does the evidence refuting the common wisdom all hang together? In other words, does the outcomes literature tell a coherent and consistent story? We need to double-check to make sure we are not missing something, for it is always discomforting to arrive at a conclusion so at odds with what society "knows" to be true.
First, as researchers Lisa Dixon and Emmanuel Stip acknowledged, there is no good evidence that antipsychotics improve longterm schizophrenia outcomes. As such, we can be confident that we haven't missed any such studies in our survey. Second, evidence that the drugs might worsen long-term outcomes showed up in the very first follow-up study conducted by the NIMH, and then it appears again and again over the next fifty years. We can link the authors of this research into a lengthy chain: Cole, Bockoven, Rappaport, Carpenter, Mosher, Harding, the World Health Organization, and Harrow. Third, once researchers came to understand how anti-
A PARADOX REVEALED • 119
psychotics affected the brain, Chouinard and Jones stepped forward with a biological explanation for why the drugs made patients more vulnerable to psychosis over the long term. They were also able to explain why the drug-induced brain changes made it so risky for people to go off the medications, and thus they revealed why the drug-withdrawal studies misled psychiatrists into believing that the drugs prevented relapse. Fourth, evidence that long-term recovery rates are higher for nonmedicated patients appears in studies and investigations of many different types. It shows up in the randomized studies conducted by Rappaport, Carpenter, and Mosher; in the cross-cultural studies conducted by the World Health Organization; and in the naturalistic studies conducted by Harding and Harrow. Fifth, we see in the tardive dyskinesia studies evidence that the drugs induce global brain dysfunction in a high percentage of patients over the long term. Sixth, once a new tool for studying brain structures came along (MRIs), investigators discovered that antipsychotics cause morphological changes in the brain and that these changes are associated with a worsening of both positive and negative symptoms, and with cognitive impairment as well. Finally, for the most part, the psychiatric researchers who conducted these studies hoped and expected to find the reverse. They wanted to tell a story of drugs that help schizophrenia patients fare well over the long term—their bias was in that direction.
We are trying to solve a puzzle in this book—why have the number of disabled mentally ill soared over the past fifty years—and I think we now have our first puzzle piece in hand. We saw that in the decade before the introduction of Thorazine, 65 percent or so of first-episode schizophrenics would be discharged within twelve months, and the majority of those discharged would not be rehospitalized in follow-up periods of four and five years. This was what we saw in Bockoven's study, too: Seventy-six percent of the psy-chotic patients treated with a progressive form of psychosocial care in 1947 were living successfully in the community five years later. But, as we saw in Harrow's study, only 5 percent of schizophrenia patients who stayed on their drugs long-term ended up recovered. That is a dramatic decline in recovery rates in the modern era, and
120 • ANATOMY OF AN EPIDEMIC
older psychiatrists, who can still remember what it was like to work with unmedicated patients, can personally attest to this difference in outcomes.
"In the nonmedication era, my schizophrenic patients did far better than do those in the more modern era," said Maryland psychiatrist Ann Silver, in an interview. "They chose careers, pursued them, and married. One patient, who had been called the sickest admitted to the adolescent division [of her hospital], is raising three children and works as a registered nurse. In the later [medicated] era, none chose a career, although many held various jobs, and none married or even had lasting relationships."
We can also see how this drug-induced chronicity has contributed to the rise in the number of disabled mentally ill. In 1955, there were 267,000 people with schizophrenia in state and county mental hospitals, or one in every 617 Americans. Today, there are an estimated 2.4 million people receiving SSI or SSDI because they are ill with schizophrenia (or some other psychotic disorder), a disability rate of one in every 125 Americans." Since the arrival of Thorazine, the disability rate due to psychotic illness has increased fourfold in our society.
Cathy, George, and Kate
In the second chapter, we met two people—Cathy Levin and George Badillo—who had been diagnosed with schizoaffective disorder (Cathy) or schizophrenia (George). We can now see how their stories fit into the outcomes literature.
As I said, Cathy Levin is one of the best responders to atypical antipsychotics that I've ever met. She could be Janssen's poster girl for promoting Risperdal. Still, she remains on SSDI and she perceives the medications as a barrier to her working full-time. Now let's go back to that moment when she had her first psychotic episode at Earlham College. What might her life have been like if she had not been immediately placed on neuroleptics, but instead
A PARADOX REVEALED • 121
had been treated with some form of psychosocial care? Or if, at some point early on, she had been encouraged to withdraw gradually from the antipsychotic medication? Would she have cycled in and out of hospitals for the next twelve years? Would she have ended up on SSDI? Although we can't really answer those questions, we can say that the drug treatment increased the likelihood that she would suffer that long period of constant hospitalizations, and decreased the likelihood that she would fully recover from her initial crackup. As Cathy said: "The thing I remember, looking back, is that I was not really that sick early on. I was really just confused."
Meanwhile, George Badillo's story illustrates how getting off meds can be the key to recovery, at least for some people diagnosed with schizophrenia. His journey out of the back wards of a state hospital began when he started tonguing his antipsychotic medica-tion. He is healthy today, he has an evident zest for life, and he revels in being a good father to his son and having his daughter Madelyne back in his life. He is an example of the many recovered people who showed up in the long-term studies by Harding and Harrow—former patients who have quit taking antipsychotics and are doing well.
Here is a third story of a young woman I'll call Kate, as she did not want her real name used. Diagnosed with schizophrenia at age nineteen, she did well on antipsychotics. In Harrow's study, she would have been among the 5 percent on meds who recovered. But she also knows what it is like to be off meds and doing well, and from her perspective, the latter type of recovery is totally unlike the first.
Before I met Kate in person, I knew from a phone conversation the bare outlines of her story, of how she had spent ten years on antipsychotics, and given that those drugs can take such a physical toll, I was a bit startled by her appearance when she showed up at my office. To be blunt, the words "drop dead gorgeous" popped into my head. A dark-haired woman, she wore jeans, a roseate top, and light makeup, and she introduced herself in a confident, warm way. Soon, she was showing me a "before" picture taken three
122 • ANATOMY OF AN EPIDEMIC
years earlier. "I was well over two-hundred pounds," she says. "I was very slow, my face was droopy. I smoked a lot of cigarettes. . . . It was very inhibiting to any sort of professional look."
Kate's story about her childhood is a familiar one. Her parents divorced when she was eight, and she remembers herself as socially awkward and horribly shy. "I only had social skills enough to interact with my family members," she says, and that awkwardness fol-lowed her to college. During her freshman year at the University of Massachusetts at Dartmouth, she found it difficult to make friends, and she felt so isolated that she cried constantly. Early in her sophomore year she dropped out and went to live with her mother in Boston, hoping to find a "purpose in life." Instead, "my sense of reality started to disintegrate," she recalls. "I started worrying about God versus the devil, and I started becoming afraid of everything. I'd say to my mom's friend, 'Is the food poisoned?' I was acting quite bizarre, and I couldn't make sense of the conversations around me. I would say these very odd things, and I would speak very slowly, very deliberately, and weird."
When she began talking about seeing wolves in her bedroom, her mother put her in the hospital. Although she stabilized pretty well on the antipsychotic medication, she hated how it made her feel, and not long after she was discharged, she abruptly went off it, which triggered a florid psychotic break. During her second hospitalization, in February 1997, she was diagnosed with schizophrenia, and this time she accepted the fact that she would have to take anti-psychotics for life. Eventually, she found a two-drug combination that worked well for her, and she began rebuilding a life. In 2001, she graduated from UMass Boston, and a year later she married a man she had met in a day treatment program. "We both had a psychiatric disability, and we both smoked heavily," she says. "We both saw therapists daily. This is what we had in common."
° Kate took a job in a group home for the mentally handicapped, and although at times she had trouble staying awake, a side effect of her medications, she earned enough to get off SSDI. For a person with schizophrenia, she was doing extremely well. Yet she wasn't happy. She had gained nearly one hundred pounds, and her husband often cruelly taunted her, telling her that she was "ugly" and
A PARADOX REVEALED • 123
had a "fat ass." She chafed too over how everybody in the system treated her. "Recovery on the med model requires you to be obedient, like a child," she explains. "You are obedient to your doctors, you are compliant with your therapist, and you take your meds. There's no striving toward greater intellectual concerns."
In 2005, she grew closer to a longtime friend, who was twenty years older and belonged to a fundamentalist religious community. She began attending their meetings, and they in turn began advising her to dress, speak, and present herself to the world in a more formal way. "They told me, 'You are representing God, and you don't want to bring shame to God," she says. Kate's older friend also urged her to stop thinking of herself as schizophrenic. "He's making me think outside the box, and to think in ways that before I never would have accepted. I would always defend my therapist, defend my psychiatrist, defend the drugs, and defend my illness. He was asking me to give up my identity as a mentally impaired person."
Soon, her old life fell completely apart. She discovered that her husband had been sleeping with one of her friends, and after she moved out of their apartment, she had to sleep for a time in her car. Although at first, during that desperate time, she clung to her meds, the nonschizophrenic vision of herself also beckoned, and in February of 2006, she decided to take the leap: She would stop smoking, she would stop drinking coffee, and she would wean herself from her psychiatric medications. "Now I have no drugs, no nicotine, and no coffee, and my body is going into shock. I am coming down from all of this, and I am almost vibrating because I need my cigarettes, my drugs."
This decision also put her at odds with most everyone in her life. "I stopped talking to my family, because I didn't want to go back into that identity [of a disabled person]. My mind was very delicate. So I had to disengage from what I knew, and disengage from my therapist." Soon, she was losing so much weight that her friends thought she must be sick. As she struggled to stay sane, she clung to the advice from her religious group, speaking to others in a very formal manner, and this behavior convinced her mother that she was relapsing. "Strange ain't the word, honey" is how her mother puts it, and even Kate privately feared that she was becoming psychotic
124 • ANATOMY OF AN EPIDEMIC
again. "But I had this hope, this faith, and so I said to myself, 'I am going to walk this tightrope across this horrible canyon, and hopefully when I get to the other side, there will be a mountain ridge I can stand on.' I had to focus on going forward regardless of where it took me, because if I fell off the tightrope, I was back in the hospital."
It was at that perilous moment, when it seemed that she was about to crash, that Kate agreed to meet her mother for dinner. "I think she is having a breakdown," her mother says. "She sat very proper, and looked scattered and disorganized. Her body was stiff. I was seeing a lot of the same symptoms as before. Her eyes were dilated and she seemed paranoid." As they drove away from the restaurant, Kate's mother started to turn toward the hospital, but at the last second she changed her mind. Kate "wasn't so crazy" that she needed to be locked up. "I went home and cried," her mother remembers. "I didn't know what was happening."
By her mother's reckoning, it took Kate six months to get through this withdrawal process. But she emerged on the other side transformed. "I see that her face is so alive now and she is more connected to her body," her mother says. "She feels comfortable in her own skin and more at peace with herself than ever. She is physically healthy. I didn't know that this kind of recovery was possible." In 2007, Kate married the older man who had encouraged her to go this route; she also has thrived in her job as the manager of a home for people with psychiatric problems, the company recognizing her for her "outstanding" performance in 2008, an award that came with a cash prize.
Kate does still struggle at times. The home she manages provides shelter to several men who are sexual deviants—"I've had people say they are going to set me on fire, or they are going to pee in my mouth," she says—and she no longer is having her emotional responses to such stress numbed by medication. "I've been off the drugs for two years, and sometimes I find it very, very difficult to deal with my emotions. I tend to have these rages of anger. Did the drugs bring such a cloud over my mind, make me so comatose, that I never gained skills on how to deal with my emotions? Now I'm finding myself getting angrier than ever and getting happier than
A PARADOX REVEALED • 125
ever too. The circle with my emotions is getting wider. And yes, it's easy to deal with when you're happy, but how do you deal with it when you are mad? I'm working on not getting overly defensive, and trying to take things in stride."
Kate's story, of course, is idiosyncratic in kind. Her success at getting off meds does not mean that everyone can successfully withdraw from them. Kate is an amazing person—incredibly willful and incredibly brave. Indeed, what the scientific literature reveals is that once a person is on an antipsychotic, it can be very difficult and risky to withdraw from the medication, and that many people suffer severe relapses. But the literature also reveals that there are people who can successfully withdraw from the medications and that it is this group that fares best in the long term. Kate made it into that group.
"That day in 2005 when I decided to get better, that's the dividing line in my life," she says. "I was a completely different person then. I was very heavy, I smoked all the time, I had flat affect. Today I run into people who knew me then, and they don't even recognize me. Even my mother says, 'You are not the same person.' "
134 • ANATOMY OF AN EPIDEMIC
Rebound Anxiety with Valium
In this 1985 study by British investigators, the patients treated with Valium did not fare better than the placebo patients during the first six weeks. The Valium patients were then withdrawn from the drug and their anxiety symptoms soared, to a much higher level than the symptoms in placebo patients. Source: Power, K. "Controlled study of withdrawal symptoms and rebound anxiety after six week course of diazepam for generalised anxiety:' British Medical Journal 290 (1985): 1246-48.
sharply during withdrawal, and to a point of panic in several patients. Patients commonly experienced bodily symptoms of anxiety, such as a choking feeling, dry mouth, hot and cold, legs like jelly, etc."29
Patients withdrawing from benzodiazepines, it seemed, were becoming more anxious than they had ever been. Over the course of the next decade, Lader and other British physicians (most notably Heather Ashton, a doctor at the University of Newcastle upon Tyne who ran a withdrawal clinic) continued to investigate this problem, and they compiled a long list of symptoms that could bedevil those quitting a benzodiazepine. In addition to rebound anxiety, patients could experience insomnia, seizures, tremors, headaches, blurred vision, a ringing in the ears, extreme sensitivity to noise, a feeling that insects were crawling over them, nightmares, hallucinations, extreme depression, depersonalization, and derealization (a sense that the external world is unreal). Withdrawal, one patient told Heather Ashton, was like "living death . . . I thought I had gone mad."
"These findings show very clearly that benzodiazepine withdrawal THE BENZO TRAP • 135
is a severe illness," Ashton wrote. "The patients were usually frightened, often in intense pain, and genuinely prostrated. . . . Through no fault of their own, the patients suffered considerable physical as well as mental distress.""
Not all people withdrawn from benzodiazepines suffer in this way. The risk of suffering withdrawal symptoms varies according to how long a person has been on the drug, the potency of the benzodiazepine, and the speed of the drug-tapering process. A majority of patients who've taken a benzodiazepine for a relatively short time, such as a month or two, may be able to withdraw from it with little difficulty. However, some people experience withdrawal symptoms after taking a benzodiazepine for only a few weeks, and it can take a longtime user a year or longer to taper from the drug. Moreover, a small percentage of people suffer a "protracted withdrawal syndrome," their anxiety remaining at elevated levels "for many months after benzodiazepine withdrawal," AshtOn observed.31 Depression may deepen, and the odd perceptual symptoms—the depersonalization, the derealization, the sensation of insects crawling on the skin—can haunt a person for an extended period. Most alarming, a small percentage of long-term users never fully recover. "It is very worrying," Lader said, in an interview. "Somehow there has been a change [in the brain]. I cannot say that everybody is going to recover back to normality when they come off long-term usage."
The biology of benzodiazepine withdrawal
5
0
7 14 28
Days of Treatment 42 56
40
35
E
o
E
V) '0
.71-2
el a)
5,
c--
< c 10
30 25 20 15
Drug withdrawal
136 • ANATOMY OF AN EPIDEMIC
In 1977, researchers discovered that benzodiazepines affect a neurotransmitter in the brain known as GABA. Unlike dopamine and serotonin, which transmit an "excitatory" message telling a neuron to fire, GABA (gamma-aminobutyric acid) inhibits neuronal activity. A neuron receiving the GABA message either fires at a slower rate or stops firing for a period of time. A majority of neurons in the brain have GABA receptors, which means that this neurotransmitter acts as the brain's brake on neuronal activity. A benzodiazepine binds to the GABA receptor and, in so doing, amplifies GABA's inhibitory effects. It pushes down on the GABA brake, so to speak, and as a result, it suppresses central nervous system activity. In response, the brain decreases its output of GABA and de-creases the density of its GABA receptors. It is trying to "restore normal GABA transmission," British scientists explained in 1982. fn 32 However, as a result of these adaptive changes, the brain's braking system is now in a physiologically impaired state. Its braking fluid is low (GABA output), and its brake pads are worn (GABA receptors). As a result, when the benzodiazepine is withdrawn, the brain is no longer able to properly inhibit neuronal activity, and its neurons may begin firing at a helter-skelter pace. This overactivity, Heather Ashton concluded, may "account for many of the effects of with-drawal." fn 33 The anxiety, the insomnia, the sensation of insects crawling across the skin, the paranoia, the derealization, the seizures—all of these vexing symptoms may arise from neuronal hyperactivity. p135
If a person gradually tapers off from a benzodiazepine, the GABA system may slowly revert to normal, and thus withdrawal symptoms may be mild. However, the fact that some long-term users suffer "protracted symptoms" is probably "due to the failure of the [GABA] receptors to revert to their normal state," Ashton said.34 Long-term benzodiazepine use, she explained, may "give rise not only to slowly reversible functional changes in the central nervous system, but may also occasionally cause structural neuronal damage."35 In such cases, the GABA brake never again functions like it should.
Long-term effects
Once researchers in the United States and the United Kingdom determined that benzodiazepines did not provide any durable relief from anxiety, an obvious question arose: Do these drugs, when taken on a continual basis, worsen the very symptom they are supposed to treat? In 1991, Karl Rickels at the University of Pennsylvania School of Medicine reported on a group of anxious patients who had tried to quit benzodiazepines three years earlier, and he found that those who had successfully gotten off the drugs were doing "significantly" better than those who had failed to do so.36 A few years later, he was back with a new study: When long-term
THE BENZO TRAP • 137
users withdrew from benzodiazepines, they "became more alert, more relaxed, and less anxious, and this change was accompanied by improved psychomotor functions."37 Those who stayed on the benzodiazepines were more emotionally distressed than those who got off.
Others told of similar long-term results. Canadian investigators found that benzodiazepine usage led to a fourfold increase in depressive symptoms.38 In England, Ashton observed that those who stay on the drugs tend to became more ill: "Many patients find that anxiety symptoms gradually increase over the years despite continuous benzodiazepine use, and panic attacks and agoraphobia may appear for the first time."39 These studies and observations told of a very problematic long-term course, and in 2007, French researchers surveyed 4,425 long-term benzodiazepine users and found that 75 percent were "markedly ill to extremely ill . . . a great majority of the patients had significant symptomatology, in particular major depressive episodes and generalized anxiety disorder, often with marked severity and disability."40
In addition to causing emotional distress, long-term benzodiazepine usage also leads to cognitive impairment. Early on, researchers recognized that memory problems were associated with short-term use, and this led David Knott, a physician at the University of Tennessee, to warn in 1976 that "I am very convinced that Valium, Librium and other drugs of that class cause damage to the brain. I have seen damage to the cerebral cortex that I believe is due to the use of these drugs, and I am beginning to wonder if the dam-age is permanent." fn 41, p137
Over the next twenty-five years, reports of cognitive impairment in long-term benzodiazepine users regularly appeared in scientific journals. These studies told of people who were having trouble focusing, remembering things, learning new material, and solving problems. However, the patients "are not aware of their reduced ability," Lader wrote, evidence that their self-insight was impaired as well. fn 42, p137
In 2004, a group of Australian scientists, after reviewing the relevant literature, concluded that "long-term benzodiazepine users were consistently more impaired than controls across all cognitive categories," with these deficits "moderate to large" in magnitude. The studies showed the "higher the intake, dose and period of use [of a benzodiazepine], the greater the risk of impairment." fn 43, p137
Increased anxiety, increased depression, and cognitive impairment—all of these factors contribute to a decline in a person's ability to function in society.
In 1983, the World Health Organization noted a "striking deterioration in personal care and social interactions" in long-term benzodiazepine users." fn 44
Another investigator reported that they end up with poor coping skills.45
In a study funded by Hoffmann-La Roche, the manufacturer of Valium, University of Michigan investigators determined that taking this drug was "associated with poor quality of life, poor performance in work and personal life, low social support, perceived lack of internal control, poor perceived health and high levels of stress." fn 46
Ashton determined that long-term use led to "malaise, ill-health, and elevated scores for neuroticism." fn 47 Benzodiazepines, she said, contribute to "job loss, unemployment, and loss of work through illness." fn 48
Such is the history told about benzodiazepines in the scientific literature. Moreover, it is a story easily traced, as Dr. Stevan Gressitt, who today is the medical director for Adult Mental Health Services in Maine, can attest. In 2002, he helped form the Maine Benzo Study Group, which was comprised of physicians and other health-care professionals, and it concluded that "there is no evidence supporting the long-term use of benzodiazepines for any mental health condition." Benzodiazepines, Gressitt and his colleagues wrote, may "aggravate" both "medical and mental health problems." In an interview, I asked Dr. Gressitt whether those "problems" included increased anxiety, cognitive impairment, and functional decline. Was his understanding of the scientific literature, I wondered, the same as mine?
"Your words I don't contradict or argue with," he replied.49 THE BENZO TRAP • 139
Geraldine, Hal, and Jill
The scientific literature reveals that benzodiazepines—much as the neuroleptics do—act like a trap. The drugs ameliorate anxiety for a short period of time, and thus they can provide a distressed person much needed relief. However, they work by perturbing a neurotransmitter system, and in response, the brain undergoes compensatory adaptations, and as a result of this change, the person becomes vulnerable to relapse upon drug withdrawal. That difficulty in turn may lead some to take the drugs indefinitely, and these patients are likely to become more anxious, more depressed, and cognitively impaired.
Here are the stories of three people who fell into the trap.
Geraldine Burns, a thin woman with dark red hair, still lives in the house she grew up in. She tells me her story while we sit in her kitchen, her elderly mother darting in and out.
Born in 1955, Geraldine was one of six children, and theirs was a happy family. Her father was Irish, her mother Lebanese, and their Boston neighborhood was known as "Little Lebanon," a place where everybody definitely knew your name. Aunts, uncles, and other relatives lived nearby. At age eighteen, Geraldine started dating a boy who lived down the block, Joe Burns. "I've been with him ever since," she says, and for a time their life unfolded just as Geraldine had hoped. She had a job that she enjoyed in human resources at a rehabilitation center, she and Joe had a healthy son (Garrett) in 1984, and they basked in their close-knit neighborhood. Geraldine—outgoing and energetic—was the constant hostess for gatherings of family and friends. "I loved my life," she says. "I loved working, I loved my family, and I loved this neighborhood. I was the one who organized the reunion of my grammar school. I still had friends from kindergarten. I couldn't have been more normal."
However, in March 1988, Geraldine gave birth to a daughter, Liana, and she felt physically unwell afterward. "I kept telling the doctors and nurses that I felt like I weighed a thousand pounds,"
142 • ANATOMY OF AN EPIDEMIC
Hal's life since then is a story of addiction. Shortly after going on the drug, he moved to San Francisco to pursue a career as a musician, and for a time it went well—he even got to hang out with Carlos Santana, the great guitarist. But his music career failed to take off, and today he thinks that the Klonopin was partly to blame, for it stifled his ambition and didn't help his finger dexterity, either. Eventually, he fell into a deep depression—"I felt like a zombie," he says—and at age twenty-nine he returned to Florida to live with his parents. At that point, he was diagnosed with bipolar illness, the government agreeing that he was so disabled by mental illness that he was eligible to receive SSI. The years slid by, his mother passed away, and then, in 2001, he began taking higher doses of Klonopin, as otherwise his depression would become unbearable. His doctor told him he was abusing the drug and sent him to a detox facility, where, over a period of ten days,, he was withdrawn from the benzodiazepine he had been taking for sixteen years.
"What happened next was absolutely the worst thing in my life," he says. "I could give you a list of symptoms, but that wouldn't do justice to what I was going through mentally. Month after month I got worse and worse. I couldn't sleep, and the symptoms—the most debilitating one was this feeling that I was dead. I felt that my brain was ripped out of my head, like I wasn't even a living thing. I had depersonalization, my skin felt weird, my body felt weird. I didn't even want to get into the shower. Even room-temperature water felt strange on my skin. If I put on mildly hot water, it felt like it was burning right through me. I couldn't digest food right, I couldn't go to the bathroom for weeks at a time, I couldn't urinate right . . . I was in a constant state of panic attacks, and this doctor is telling me it's all in my mind, that he won't write me a script, and that withdrawal symptoms can last a maximum of thirty days. I was cracking up, going insane."
This went on for ten months. He found Geraldine Burns on the Internet, as she had started a benzodiazepine support group, and she would console him for hours at a time. Ten, twenty times a night he would call his sister Susan, screaming that he was going to kill himself. He desperately sought to get a new prescription for Klonopin, but the doctors he saw didn't believe that his torment
THE BENZO TRAP • 143
was related to benzodiazepine withdrawal. Instead, they figured that he had abused the drug in the past and so they refused to put him back on it. "They don't understand that the drug changes the whole biology of your brain, and that your brain doesn't work right anymore," Hal says. Finally, his sister found a physician who agreed to write him a script, and "within hours, the nightmare was over. Every single side effect, every single withdrawal problem I had been going through was gone. Completely. Like magic. I was jumping up and down I was so excited."
Hal has never tried going off Klonopin again. His brain adapted to the drug, he says, and now it can't adapt back. "Klonopin ruined my life. It takes away your drive, and in the morning, you don't want to get out of bed, because you feel so groggy. I don't even know what it's like to feel normal. This is my world. Things don't get me as excited as most people because I'm in a constant state of sedation. It should never have been pregcribed for long-term use."
Susan sees it much the same way. "My sister and I have talked at length about how our brother is very good-looking, and how when he is acting normal, you would not know there is anything wrong," she says. "He is adorable, charming; he carries on conversations. He could have been with a nice woman and had a family. But now? He has no friends. None whatsoever. He stays at home most of the time, except when he has to go to the store. He is trapped. He can't get off Klonopin. I feel terrible for him, and I feel terrible for my dad, who when he dies will never have seen his son do well. It kills us that he could have had a life."
If a picture is worth a thousand words, the photos that Jill, an Ohio woman in her mid-thirties, sends me tell her story in a very succinct fashion. There is the "before" photo in which she is smiling and looking confidently into the camera, posed like a model in a fashionable black dress. One hand is posed gracefully on her hip, a pearl necklace adds a touch of elegance, and she is a bit dolled up—the makeup and styled black hair tell of a woman who presents herself carefully to the world. And then there is the "after" photo, her eyes hollowed out and bloodshot, her face taut and drawn, her hair
144 • ANATOMY OF AN EPIDEMIC
thinned—she looks like a somewhat crazed methamphetamine addict who is now getting her photo taken following an arrest.
We first spoke on the phone in July of 2008, three months after she had taken her last dose of a benzodiazepine, a drug she had been on for thirteen years. Here's how she starts her story: "My head is feeling crushed. It's like horses are kicking my skull."
Jill, who asked that I not use her last name, grew up in an affluent suburb of Columbus, Ohio, where she attended private schools and excelled in multiple ways. She sang competitively, won school awards for her art, and was a top student. Petite and pretty, she was asked by a representative of the Miss Ohio pageant to enter that competition. "I was a vibrant, creative, fun person," she says. However, she did occasionally struggle with anxiety and depression, and during her sophomore year at Ohio State University a psychiatrist put her on an antidepressant. Unfortunately, that drug seemed to increase her anxiety, and so eventually the psychiatrist added Klonopin to the mix. "He said it was a gentle little pill used to help old ladies sleep. He said that it wasn't addictive and that if I wanted to stop, at most I'd experience a few nights of bad sleep. But he said I would probably need to take it for life, just like a diabetic needs insulin."
For the next ten years, Jill functioned okay. She graduated summa cum laude from Ohio State University in 1996, earned a master's degree in counseling, and after various adventures, in 2002 she began teaching fourth grade in a public school. However, throughout this period, her anxiety returned again and again, and each time it did, her psychiatrist upped her dose of Klonopin. And as the dose increased, her ability to function declined. "I would wonder, What is wrong with me? Why am I becoming so withdrawn? Why am I losing interest in everything? I was getting sicker and sicker." Then, in late 2004, the anxiety, panic, and depression returned worse than ever, and new symptoms—obsessions and suicidal ideation—appeared too. She was told this meant she was "bipolar" and she was prescribed an antipsychotic, Abilify. "That's when I flipped out. My anxiety went through the roof, it was like being injected with stimulants, and I was teaching one day and I
THE BENZO TRAP • 145
started crying in class. I couldn't take it anymore, and I was hospitalized in a psychiatric ward."
Now came the drug merry-go-round. During the next two years, Jill was put on Lamictal, Lexapro, Seroquel, Neurontin, lithium, Wellbutrin, and other drugs she can't remember, with Klonopin always part of the cocktail. This treatment caused her eyes to swell, her skin to break into rashes, and her eyebrows and hair to fall out. "My poor brain was being treated like a mixing bowl," she says. Only when she asked doctors whether the cocktail might be making her sick, "they would say, 'We have tried the drugs and they are not helping, and, so the problem is you.' " Indeed, since the drugs weren't working, her psychiatrists gave her electroshock, which took its toll on her memory.
Growing ever more desperate, toward the end of 2006 Jill concluded that "it was the drugs that were making me sick." She began withdrawing from the medications one by one, and although she was able to get off the antidepressants and antipsychotics, every time she tried tapering off Klonopin she suffered a long list of torments: hallucinations, horrible anxiety, vertigo, painful muscle spasms, perceptual distortions, and derealization, just to name a few. Finally, in the spring of 2008, she adopted a new strategy: She would get off by progressively switching to less potent benzodiazepines. Klonopin was replaced by Valium, the Valium by Librium, and then, in April 2008, she withdrew from Librium. She was now drug free, yet three months later, when I spoke to her on the phone, she was still in withdrawal torment. "What I've been through .. . the trauma," she says, breaking into tears. "I feel dizzy all the time. It is like the floor is tilting one way and I am spinning the other way. It is horrific. I have had hallucinations, I have to wear sunglasses in the house, sometimes I scream from the pain."
At the end of our interview, I asked her to think back to what her life had been like before she was put on a benzodiazepine, and once more she began to cry.
"My anxiety then was like a mild case of asthma, and today it's like I have end-stage lung disease. I'm terrified that I'm not going to make it. I'm so, so scared."
154 • ANATOMY OF AN EPIDEMIC
Four years later, the NIMH conducted a review of all antidepressant studies, and it found that the "more stringently controlled the study, the lower the improvement rate reported for a drug." In well-controlled studies, 61 percent of the drug-treated patients improved versus 46 percent of the placebo patients, a net benefit of only 15 percent. "The differences between the effectiveness of antidepressant drugs and placebo are not impressive," it said.19 The NIMH then conducted its own trial of imipramine, and it was only in psychotically depressed patients that this tricyclic showed any significant benefit over a placebo. Only 40 percent of the drug-treated patients completed the seven-week study, and the reason so many dropped out was that their condition "deteriorated." For many depressed patients, the NIMH concluded in 1970, "drugs play a minor role in influencing the clinical course of their illness."2°
The minimal efficacy of imipramine and other antidepressants led some investigators to wonder whether the placebo response was the mechanism that was helping people feel better. What the drugs did, several speculated, was amplify the placebo response, and they did so because they produced physical side effects, which helped convince patients that they were getting a "magic pill" for depression. To test this hypothesis, investigators conducted at least seven studies in which they compared a tricyclic to an "active" placebo, rather than an inert one. (An active placebo is a chemical that produces an unpleasant side effect of some kind, like dry mouth.) In six of the seven, there was no difference in outcomes. fn 21, p 154
That was the efficacy record racked up by tricyclics in the 1970s: slightly better than inactive placebo, but no better than an active placebo. The NIMH visited this question of imipramine's efficacy one more time in the 1980s, comparing it to two forms of psy-chotherapy and placebo, and found that nothing had changed. At the end of sixteen weeks, "there were no significant differences among treatments, including placebo plus clinical management, for the less severely depressed and functionally impaired patients." Only the severely depressed patients fared better on imipramine than on a placebo.22
Societal belief in the efficacy of antidepressants was reborn with the arrival of Prozac in 1988. Eli Lilly, it seemed, had come up
AN EPISODIC ILLNESS TURNS CHRONIC • 155
with a very good pill for the blues. This selective serotonin reuptake inhibitor (SSRI) was said to make people feel "better than well." Unfortunately, once researchers began poking through the clinical trial data submitted to the FDA for Prozac and the other SSRIs that were subsequently brought to market, the "wonder drug" story fell apart.
The first blow to the SSRIs' image came from Arif Khan at the Northwest Clinical Research Center in Washington. He reviewed the study data submitted to the FDA for seven SSRIs and concluded that symptoms were reduced 42 percent in patients treated with tricyclics, 41 percent in the SSRI group, and 31 percent in those given a placebo.23 The new drugs, it turned out, were no more effective than the old ones. Next, Erick Turner from Oregon Health and Science University, in a review of FDA data for twelve antidepressants approved between 1987 and 2004, determined that thirty-six of the seventy-four trials had failed to show any statistical benefit for the antidepressants. There were just as many trials that had produced negative or "questionable" results as positive ones.24 Finally, in 2008, Irving Kirsch, a psychologist at the University of Hull in the United Kingdom, found that in the trials of Prozac, Effexor, Serzone, and Paxil, symptoms in the medicated patients dropped 9.6 points on the Hamilton Rating Scale of Depression, versus 7.8 points for the placebo group. This was a difference of only 1.8 points, and the National Institute for Clinical Excellence in Britain had previously determined that a three-point drug-placebo difference was needed on the Hamilton scale to demonstrate a "clinically significant benefit." It was only in a small subgroup of patients—those most severely depressed—that the drugs had been shown to be of real use. "Given these data, there seems little evidence to support the prescription of antidepressant medication to any but the most severely depressed patients, unless alternative treatments have failed to provide benefit," Kirsch and his collaborators concluded.25
All of this provoked some soul-searching by psychiatrists in their journals. Randomized clinical trials, admitted a 2009 editorial in the British Journal of Psychiatry, had generated "limited valid evidence" for use of the drugs.26
A group of European psychiatrists affiliated with the World Health Organization conducted their own review of Paxil's clinical data and concluded that "among adults with moderate to severe major depression," this popular SSRI "was not superior to placebo in terms of overall treatment effectiveness and acceptability." fn 27, p 156
Belief in these medications' effectiveness, wrote Greek psychiatrist John Ioannidis, who has an appointment at Tufts University School of Medicine in Massachusetts, was a "living myth." A review of the SSRI clinical data had led to a depressing end for psychiatry, and, as Ioannidis quipped, he and his colleagues couldn't even now turn to Prozac and the other SSRIs for relief from this dispiriting news because, alas, "they probably won't work."28
There is one other interesting addendum to this research history. In the late 1980s, many Germans who were depressed turned to Hypericum perforatum, the plant known as Saint-John's-wort, for relief. German investigators began conducting double-blind trials of this herbal remedy, and in 1996, the British Medical Journal summarized the evidence: In thirteen placebo-controlled trials, 55 percent of the patients treated with Saint-John's-wort significantly improved, compared with 22 percent of those given a placebo. The herbal remedy also bested antidepressants in head-to-head competition: In those trials, 66 percent given the herb improved compared to 55 percent of the drug-treated patients. In Germany, SaintJohn's-wort was effective. But would it work similar magic in Americans? In 2001, psychiatrists at eleven medical centers in the United States reported that it wasn't effective at all. Only 15 percent of the depressed outpatients treated with the herb improved in their eight-week trial. Yet—and this was the curious part—only 5 percent of the placebo patients got better in this study, far below the usual placebo response. American psychiatrists, it seemed, were not eager to see anyone as having gotten better, lest the herb prove effective.
But then the NIH funded a second trial of Saint-John's-wort that had a design that complicated matters for any researcher who wanted to play favorites. It compared Saint-John's-wort to both Zoloft and a placebo. Since the herb causes side effects, such as dry mouth, it would act at the very least as an active placebo. As such, this truly was a blinded trial, the psychiatrists unable to rely on side effects as a clue to which patients were getting what, and here were the results: Twenty-four percent of the patients treated with Saint John's-wort had a "full response," 25 percent of the Zoloft patients, and 32 percent of the placebo group. "This study fails to support the efficacy of H perforatum in moderately severe depression," the investigators concluded, glossing over the fact that their drug had failed this test too. fn 29, p156
The Chronicity Factor, Yet Again
The antidepressants' relative lack of short-term efficacy was not, by itself, a reason to think that the drugs were causing harm. After all, most of those treated with antidepressants were seeing their symptoms abate. Medicated patients in the short-term trials were getting better. The problem was that they were not improving significantly more than those treated with a placebo. However, during the 1960s, several European psychiatrists reported that the long-term course of depression in their drug-treated patients seemed to be worsening.
Exposure to antidepressants, wrote German physician H. P. Hoheisel in 1966, appeared to be "shortening the intervals" between depressive episodes in his patients. These drugs, wrote a Yugoslavian doctor four years later, were causing a "chronification" of the disease. The tricyclics, agreed Bulgarian psychiatrist Nikola Schipkowensky in 1970, were inducing a "change to a more chronic course." The problem, it seemed, was that many people treated with antidepressants were only "partially cured."3° Their symptoms didn't entirely remit, and then, when they stopped taking the antidepressant, their depression regularly got much worse again.
With this concern having surfaced in a few European journals, a Dutch physician, J. D. Van Scheyen, examined the case histories of ninety-four depressed patients. Some had taken an antidepressant and some had not, and when Van Scheyen looked at how the two groups had fared over a five-year period, the difference was startling: "It was evident, particularly in the female patients, that more systematic long-term antidepressant medication, with or without ECT [electroconvulsive therapy], exerts a paradoxical effect on the
158 • ANATOMY OF AN EPIDEMIC
recurrent nature of the vital depression. In other words, this therapeutic approach was associated with an increase in recurrent rate and a decrease in cycle duration. . . . Should [this increase] be regarded as an untoward long-term side effect of treatment with tricyclic antidepressants ?"31
Over the next twenty years, investigators reported again and again that people treated with an antidepressant were very likely to relapse once they stopped taking the drug. In 1973, investigators in Britain wrote that 50 percent of drug-withdrawn patients relapsed within six months;32 a few years later, investigators at the University of Pennsylvania announced that 69 percent of patients withdrawn from antidepressants relapsed within this time period. There was, they confessed, "rapid clinical deterioration in most of the pa-tients."33 In 1984, Robert Prien at the NIMH reported that 71 percent of depressed patients relapsed within eighteen months of drug withdrawal.34 Finally, in 1990, the NIMH added to this gloomy picture when it reported the long-term results from its study that had compared imipramine to two forms of psychotherapy and to a placebo. At the end of eighteen months, the stay-well rate was best for the cognitive therapy group (30 percent) and lowest for the imipramine-exposed group (19 percent).35
Everywhere, the message was the same: Depressed people who were treated with an antidepressant and then stopped taking it regularly got sick again. In 1997, Ross Baldessarini from Harvard Medical School, in a meta-analysis of the literature, quantified the relapse risk: Fifty percent of drug-withdrawn patients relapsed within fourteen months.36 Baldessarini also found that the longer a person was on an antidepressant, the greater the relapse rate following drug withdrawal. It was as though a person treated with the drug gradually became less and less able, in a physiological sense, to do without it. Investigators in Britain came to the same sobering realization: "After stopping an antidepressant, symptoms tend to build up gradually and become chronic."37
AN EPISODIC ILLNESS TURNS CHRONIC • 159
Do All Psychotropics Work This Way?
Although a handful of European physicians may have sounded the alarm about the changing course of depression in the late 1960s and early 1970s, it wasn't until 1994 that an Italian psychiatrist, Giovanni Fava, from the University of Bologna, pointedly announced that it was time for psychiatry to confront this issue. Neuroleptics had been found to be quite problematic over the long term, the benzodiazepines had, too, and now it looked like the antidepressants were producing a similar long-term record. In a 1994 editorial in Psychotherapy and Psychosomatics, Fava wrote:
“Within the field of psychopharmacology, practitioners have been cautious, if not fearful, of opening a debate on whether the treatment is more damaging [than helpful]. . . . I wonder if the time has come for debating and initiating research into the likelihood that psychotropic drugs actually worsen, at least in some cases, the progression of the illness which they are supposed to treat." fn 38 (1994 that an Italian psychiatrist, Giovanni Fava, from the University of Bologna, 1994 editorial in Psychotherapy and Psychosomatics)
In this editorial and several more articles that followed, Fava offered a biological explanation for what was going on with the antidepressants. Like antipsychotics and benzodiazepines, these drugs perturb neurotransmitter systems in the brain. This leads to compensatory
"processes that oppose the initial acute effects of a drug. . . . When drug treatment ends, these processes may operate unopposed, resulting in appearance of withdrawal symptoms and increased vulnerability to relapse," he wrote. fn 39 Moreover, Fava noted, pointing to Baldessarini's findings, it was evident that the longer one stayed on antidepressants, the worse the problem. "Whether one treats a depressed patient for three months, or three years, it does not matter when one stops the drugs. A statistical trend suggested that the longer the drug treatment, the higher the likelihood of relapse." fn 40
But, Fava also wondered, what was the outcome for people who stayed on antidepressants indefinitely? Weren't they also relapsing
i6o • ANATOMY OF AN EPIDEMIC
with great frequency? Perhaps the drugs cause "irreversible receptor modifications," Fava said, and, as such, "sensitize" the brain to depression. This could explain the "bleak long term outcome of depression." He summed up the problem in this way:
“Antidepressant drugs in depression might be beneficial in the short term, but worsen the progression of the disease in the long term, by increasing the biochemical vulnerability to depression. . . . Use of antidepressant drugs may propel the illness to a more malignant and treatment unresponsive course.” fn 41
This possibility was now front and center in psychiatry. "His question and the several related matters . . . are not pleasant to contemplate and may seem paradoxical, but they now require open-minded and serious clinical and research consideration," Baldessarini said.42 Three physicians from the University of Louisville School of Medicine echoed the sentiment. "Long-term antidepressant use may be depressogenic," they wrote, in a 1998 letter to the Journal of Clinical Psychiatry. "It is possible that antidepressant agents modify the hardwiring of neuronal synapses [which] not only render antidepressants ineffective but also induce a resident, refractory depressive state." fn 43
One-Year Outcomes in WHO Screening Study for Depression
The WHO investigators reported that a higher percentage of the unmedicated group recovered, and that"continuing depression"was highest in those treated with an antidepressant. Source: Goldberg, D. "The effects of detection and treatment of major depression in primary care."British Journal of General Practice 48 (1998): 1840-44.
i66 • ANATOMY OF AN EPIDEMIC
Mental Health in Ontario identified 1,281 people who went on short-term disability between 1996 and 1998 because they missed ten consecutive' days of work due to depression. The 564 people who subsequently didn't fill a prescription for an antidepressant returned to work, on average, in 77 days, while the medicated group took 105 days to get back on the job. More important, only 9 percent of the unmedicated group went on to long-term disability, compared to 19 percent of those who took an antidepressant." "Does the lack of antidepressant use reflect a resistance to adopting a sick role and consequently a more rapid return to work?" Dewa won-
" This study powerfully illustrates why we, as a society, may be deluded about the merits of antidepressants. Seventy-three percent of those who took an antidepressant returned to work (another 8 percent quit or retired), and undoubtedly many in that group would tell of how the drug treatment helped them. They would become societal voices attesting to the benefits of this paradigm of care, and without a study of this kind, there would be no way to know that the medications were, in fact, increasing the risk of long-term disability.
AN EPISODIC ILLNESS TURNS CHRONIC • 167
The Risk of Disability for Depressed Patients
This was a study of 1,281 employees in Canada who went on short-term disability due to depression. Those who took an antidepressant were more than twice as likely to go on to longterm disability. Source: Dewa, C. "Pattern of antidepressant use and duration of depression-related absence from work:' British Journal of Psychiatry 183 (2003): 507-13.
dered."' In a similar vein, University of Iowa psychiatrist William Coryell and his NIMH-funded colleagues studied the six-year "naturalistic" outcomes of 547 people who suffered a bout of depression, and they found those who were treated for the illness were three times more likely than the untreated group to suffer a "cessation" of their "principal social role" and nearly seven times more likely to become "incapacitated." Moreover, while many of the treated patients saw their economic status markedly decline during the six years, only 17 percent of the unmedicated group saw their incomes drop, and 59 percent saw their incomes rise. "The untreated individuals described here had milder and shorter-lived illnesses [than those who were treated], and, despite the absence of treatment, did not show significant changes in socioeconomic status in the long term," Coryell wrote."
Several countries also observed that following the arrival of the SSRIs, the number of their citizens disabled by depression dramatically increased. In Britain, the "number of days of incapacity" due to depression and neurotic disorders jumped from 38 million in 1984 to 117 million in 1999, a threefold increase.62 Iceland reported that the percentage of its population disabled by depression
60% 50% 40% 30% 20% 10% 0% Diagnosed/ Antidepressants
•Diagnosed/ Sedatives 1111 Diagnosed/
No Drug
1.1 Undiagnosed/
No Drug
Well Continuing Depression
Returned to Work
Long-term Disability
Quit/Retired/ Fired
0% 20% 40% 60% 80% 100%
Medicated
Unmedicated
It's the Disease, Not the Drug
Once again, psychiatry had reached a moment of crisis. The specter of supersensitivity psychosis had stirred up a hornets' nest in the early 1980s, and now, in the mid-1990s, a concern very similar in kind had appeared. This time, the stakes were perhaps even higher. Fava was raising this issue even as U.S. sales of SSRIs were soaring. Prominent psychiatrists at the best medical schools in the United States had told newspaper and magazine reporters of their wonders. These drugs were now being prescribed to an ever-larger group of people, including to more than a million American children. Could
AN EPISODIC ILLNESS TURNS CHRONIC • 1-61
the field now confess that these medications might be making people chronically depressed? That they led to a "malignant" long-term course? That they caused biological changes in the brain that "sensitized" a person to depression? And if that were so, how could they possibly be prescribed to young children and teenagers? Why would doctors do that to children? This concern of Fava's needed to be hushed Up, and hushed up fast. Early in 1994, after Fava first broached the subject, Donald Klein from Columbia University told Psychiatric News that this subject was not going to be investigated.
"The industry is not interested [in this question], the NIMH is not interested, and the FDA is not interested," he said. "Nobody is interested."44
Indeed, by this time, leaders of American psychiatry were already coming up with an alternative explanation for the "bleak" longterm outcomes, one that spared their drugs any blame. The old epidemiological studies from the pre-antidepressant era, which had shown that people regularly recovered from a severe depressive episode and that a majority then stayed well, were "flawed." A panel of experts convened by the NIMH put it this way: "Improved approaches to the description and classification of [mood] disorders and new epidemiologic studies [have] demonstrated the recurrent and chronic nature of these illnesses, and the extent to which they represent a continual source of distress and dysfunction for affected individuals. "45. Depression was at last being understood, that was the story that psychiatry embraced, and textbooks were rewritten to tell of this advance in knowledge. Not long ago, noted the 1999 edition of the American Psychiatric Association's Textbook of Psychiatry, it was believed that "most patients would eventually recover from a major depressive episode. However, more extensive studies have disproved this assumption."46 It was now known, the APA said, that "depression is a highly recurrent and pernicious disorder."
Depression, it seemed, had never been the relatively benign illness described by Silverman and others at the NIMH in the late 1960s and early 1970s. And with depression reconceived in this way, as a chronic illness, psychiatry now had a rationale for long-term use of antidepressants. The problem wasn't that exposure to an antidepressant caused a biological change that made people more
164 • ANATOMY OF AN EPIDEMIC
person's lifetime, but more often, it recurs throughout a person's life," the NIMH warns.54
4
Unmedicated v. Medicated Depression
We've now arrived at an intellectual place similar to what we expe rienced with the antipsychotics: Can it really be that antidepressants, which are so popular with the public, worsen long-term outcomes? All of the data we've reviewed so far indicates that the drugs do just that, but there is one piece of evidence that we are still missing: What does unmedicated depression look like today? Does it run a better long-term course? Unfortunately, as researchers from the University of Ottawa discovered in 2008, there aren't good-quality randomized trials comparing long-term outcomes in antidepressant-treated and never-medicated patients. As such, they concluded, randomized trials "provide no guidance for longer treatment."55 However, we can search for "naturalistic" studies that might help us answer this question.*
Researchers in the UK, the Netherlands, and Canada investigated this question by looking back at case histories of depressed patients whose medication use had been tracked. In a 1997 study of outcomes at a large inner-city facility, British scientists reported that ninety-five never-medicated patients saw their symptoms decrease by 62 percent in six months, whereas the fifty-three drug-treated patients experienced only a 33 percent reduction in symptoms. The medicated patients, they concluded, "continued to have depressive symptoms throughout the six months. "56 Dutch investigators, in a retrospective study of the ten-year outcomes of 222 people who had
* The caveat with the naturalistic studies is that the unmedicated cohort, at the moment of initial diagnosis, may not be as depressed as those who go on drugs. Furthermore, those who eschew drugs may also have a greater "inner resilience." Even given these caveats, we should be able to gain a sense of the course of unmedicated depression from the naturalistic studies, and see how it compares to the course of depression treated with antidepressants.
AN EPISODIC ILLNESS TURNS CHRONIC • 165
suffered a first episode of depression, found that 76 percent of those not treated with an antidepressant recovered and never relapsed, compared to 50 percent of those prescribed an antidepressants7 Finally, Scott Patten, from the University of Calgary, plumbed a large Canadian health database to assess the five-year outcomes of 9,508 depressed patients, and he determined that the medicated patients were depressed on average nineteen weeks each year, versus eleven weeks for those not taking the drugs. These findings, Patten wrote, were consistent with Giovanni Fava's hypothesis that "antidepressant treatment may lead to a deterioration in the long-term course of mood disorders."58
A study conducted by the World Health Organization in fifteen cities around the world to assess the value of screening for depression led to similar results. The researchers looked for depression in patients who showed up at health clinics for other complaints, and then, in a fly-on-the-wall manner, followed those they had identified as depressed for the next twelve months. They reasoned that the general practitioners in the clinics would detect depression in some of the patients but not all, and hypothesized that outcomes would fall into four groups: those diagnosed and treated with antidepressants would fare the best, those diagnosed and treated with benzodiazepines would fare the second best, those diagnosed and treated without psychotropics the third best, and those undetected and un-treated the worst. Alas, the results were the opposite. Altogether, the WHO investigators identified 740 people as depressed, and it was the 484 who weren't exposed to psychotropic medications (whether diagnosed or not) that had the best outcomes. They enjoyed much better "general health" at the end of one year, their depressive symptoms were much milder, and a lower percentage were judged to still be "mentally ill." The group that suffered most from "continued depression" were the patients treated with an antide-pressant. The "study does not support the view that failure to recognize depression has serious adverse consequences," the investigators wrote."
Next, researchers in Canada and the United States studied whether antidepressant use affected disability rates. In Canada, Carolyn Dewa and her colleagues at the Centre for Addiction and
168 • ANATOMY OF AN EPIDEMIC
NIMH's Study of Untreated Depression
In this study, the NIMH investigated the naturalistic outcomes of people diagnosed with major depression who got treatment and those who did not. At the end of six years, the treated patients were much more likely to have stopped functioning in their usual societal roles and to have become incapacitated. Source: Coryell, W."Characteristics and significance of untreated major depressive disorder." American Journal of Psychiatry 152 (1995): 1124-29.
nearly doubled from 1976 to 2000. If antidepressants were truly helpful, the Iceland investigators reasoned, then the use of these drugs "might have been expected to have a public health impact by reducing disability, morbidity, and mortality due to depressive disorders."63 In the United States, the percentage of working-age Americans who said in health surveys that they were disabled by depression tripled during the 1990s.64
There is one final study we need to review. In 2006, Michael Posternak, a psychiatrist at Brown University, confessed that "unfortunately, we have little direct knowledge regarding the untreated course of major depression." The poor long-term outcomes detailed in APA textbooks and the NIMH studies told the story of medicated depression, which might be a very different beast. To study what untreated depression might be like in modern times, Posternak and his collaborators identified eighty-four patients enrolled in the NIMH's Psychobiology of Depression program who, after recovering from an initial bout of depression, subsequently relapsed but did not then go back on medication. Although these patients were not a "never-exposed" group, Posternak could still track their "untreated" recovery from this second episode of depression. Here were the results: Twenty-three percent recovered in one month, 67 percent in six months, and 85 percent within a year. Kraepelin, Posternak noted, had said that untreated depressive episodes usually cleared up within six to eight months, and these results provided "perhaps the most methodologically rigorous confirmation of this estimate." fn 65
The old epidemiological studies were apparently not so flawed after all. This study also showed why six-week trials of the drugs had led psychiatry astray. Although only 23 percent of the unmedicated patients were recovered after one month, spontaneous remis-sions continued after that at the rate of about 2 percent per week, and thus at the end of six months, two-thirds were depression free. It takes time for unmedicated depression to lift, and that is missed in short-term trials. "If as many as 85% of depressed individuals who go without somatic treatment spontaneously recover within one year, it would be extremely difficult for any intervention to demonstrate a superior result to this," Posternak said.66
It was just as Joseph Zubin had warned in 1955: "It would be foolhardy to claim a definite advantage for a specified therapy without a two- to five-year follow-up."67
Nine Million and Counting
We can now see how the antidepressant story all fits together, and why the widespread use of these drugs would contribute to a rise in the number of disabled mentally ill in the United States. Over the short term, those who take an antidepressant will likely see their symptoms lessen. They will see this as proof that the drugs work, as will their doctors. However, this short-term amelioration of symptoms is not markedly greater than what is seen in patients treated with a placebo, and this initial use also puts them onto a problem-atic long-term course. If they stop taking the medication, they are at high risk of relapsing. But if they stay on the drugs, they will also
Treated
35%
30% 25% 20% 15% 10% 5% 0% Treated
Untreated
Cessation of Role Function Became Incapacitated
174 • ANATOMY OF AN EPIDEMIC
pharmaceutical firms. They regularly opened with a joke before moving on to their PowerPoint slides, which were splashed on ballroom screens larger than those found in most theaters. Often the diners were given handheld remote devices to answer multiple-choice questions during the presentations, with dramatic music playing as they keyed in their responses, much as it might during "Final Jeopardy," and when their collective wisdom was splashed on the screens, most usually got the answer right. "You guys are so smart," one speaker said.
Patty Duke provided the 2008 APA meeting with its celebrity patient story. AstraZeneca sponsored her talk, and the company spokesman who introduced her, apparently worried that somehow the audience might miss the point of what she had to say, informed everyone that "the take-home message is that mental illness is diagnosable and recognizable, and that treatment works." Then the Oscar-winning actress, clad in a pumpkin orange dress, told of how she had suffered from undiagnosed bipolar illness for twenty years, during which time she drank excessively and was sexually promiscuous. Diagnosis and medication "made me marriage material," she said, and whenever she speaks to patient groups around the country, she hammers this point home. "I tell them, 'Take your medicines!' " she said. The drugs fix the disease "with very little downside!" The audience clapped loudly at that, and then America's favorite identical cousin offered the psychiatrists a final benediction: "We are beyond blessed to have people like you who have chosen to take care of us and to lead us to a balanced life. . . . I get my information from you and NAMI [National Alliance on Mental Illness], and if I resisted such information, I would deserve to have a net thrown over me. When I hear someone say, at one of my talks, 'I don't need the medication, I don't take it,' I tell them to 'sit down, you are making a fool of yourself.' "
That led to a standing ovation, and so, as I put away my notebook, it seemed certain that this was a meeting where the bottom-line message, no matter where you went, would be quite well controlled. Nearly everything was set up and organized in a way that told of a profession quite confident in its therapeutics, and while I knew that Martin Harrow would be giving a talk on his
THE BIPOLAR BOOM • 175
long-term study of schizophrenia outcomes, he had been allotted only twenty minutes, and his session had been assigned to one of the convention center's smallest rooms. His presentation would be the one exception to the rule, and so I didn't expect to hear anything startling on the Tuesday afternoon that I squeezed my way into a crowded, slightly larger room for a forum titled "Antidepressants in Bipolar Disorder." I figured that the speakers would simply present trial results that justified, in one way or another, the use of these drugs, but soon I was writing furiously away. The discussion, which was led by the top bipolar experts in the country, including the two grand old men of biological psychiatry in the United States, Frederick Goodwin and Robert Post, focused on this question: Do antidepressants worsen the long-term course of bipolar disorder? And notably so?
"The illness has been altered," said Goodwin, who in 1990 coauthored the first edition of his text Manic-Depressive Illness, which is considered the bible in the field. Today "we have a lot more rapid cycling than we described in the first edition, a lot more mixed states than we described in the first edition, a lot more lithium resistance, and a lot more lithium treatment failure than there was in the first edition. The illness is not what Kraepelin described anymore, and the biggest factor, I think, is that most patients who have the illness get an antidepressant before they ever get exposed to a mood stabilizer."
This was the opening salvo in what turned into an hour-long confessional. Although not all the speakers agreed that antidepressants had been disastrous for bipolar patients, that was the general theme, and nobody questioned Goodwin's bottom-line summary that bipolar outcomes had noticeably worsened in the past twenty years.
Antidepressants, said Nassir Ghaemi, from Tufts Medical Center, can cause manic switches and turn patients into "rapid cyclers," and may increase the amount of time they spend in depressive episodes. Rapid cycling, Post added, led to a very bad end.
"The number of episodes, and it's a very rich literature [documenting this], is associated with more cognitive deficits," he said. "We are building more episodes, more treatment resistance, more cognitive dysfunction, and there is data showing that if you have four depressive episodes, unipolar or bipolar, it doubles your late-risk of dementia. And guess what? That isn't even the half of . . . In the United States, people with depression, bipolar, and schizophrenia are losing twelve to twenty years in life expectancy impared to people not in the mental health system." (Antidepressants in Bipolar Disorder: Do antidepressants worsen the long-term course of bipolar disorder?, Fredrick Goodwin, 2008 APA annual meeting)
These were words that told of a paradigm of care that had npletely failed, of treatment that made patients constantly symptoLtic and cognitively impaired, and led to their early death as well. low you just heard that one of the things we do doesn't work very .11 in the long term," Post practically screamed. "So what the hell mild we be doing?"
The confessions came fast and furious. Psychiatry, of course, had "evidence base" for using antidepressants in bipolar disorder, t, Post said, the clinical trials conducted by pharmaceutical comnies "are virtually useless for us as clinicians. . . . They don't tell what we really need to know, what our patients are going to re3nd to, and if they don't respond to that first treatment, what Auld be the next iteration, and how long they should stay on ngs." Only a small percentage of people, he added, actually "re3nd to these crummy treatments, like antidepressants." As for :ent pharma-funded trials that had shown that bipolar patients thdrawn from antipsychotic medications relapsed at high rates, rich theoretically served as evidence that patients needed to take :se drugs long-term, those studies "were designed to get relapse the placebo group]," Goodwin said. "It isn't evidence that the ag is still needed; it's evidence that if you suddenly change a brain it has adapted to the drug, you are going to get 'relapse." Added st: "Right now, fifty years after the advent of antidepressant ags, we still don't really know how to treat bipolar depression. need new treatment algorithms that aren't just made up."
This was all much like the moment in The Wizard of Oz when curtain is pulled back and the mighty wizard is revealed as a 41 old man. For anyone in the audience who had spent his or her )rning in Pfizer's welcoming center, answering video-game quesns about the wonders of Geodon for bipolar illness, it must have en crushing. Thirty years earlier, Guy Chouinard and Barry Jones d rattled the profession with their talks on drug-induced
THE BIPOLAR BOOM • 177
"supersensitivity psychosis," and now the profession was being asked to confront the fact that bipolar outcomes were worse today than they had been thirty years earlier, and that antidepressants were a likely culprit. Stimulants, it seemed, could make bipolar patients worse too, and at last Ghaemi told the audience that psychiatry needed to adopt a "Hippocratic" approach to the use of psychiatric medications, which would require them to stop prescribing them unless they had good evidence they were truly beneficial over the long term. "Diagnosis, not druggery," he said, and at one point, several in the audience—which had grown increasingly agitated by this discussion—booed him.
"Can fifty thousand psychiatrists be wrong?" he asked, speaking about the profession's use of antidepressants as a treatment for bipolar disorder. "I think that the answer is yes, probably."
Bipolar Before Lithium
Readers of this book, having come this far in the text, cannot be surprised to learn that outcomes for bipolar disorder have dramatically worsened in the pharmacotherapy era. The only surprising thing is that this failure was so openly discussed at the APA meeting. Given what the scientific literature revealed about the long-term outcomes of medicated schizophrenia, anxiety, and depression, it stood to reason that the drug cocktails used to treat bipolar illness were not going to produce good long-term results. The increased chronicity, the functional decline, the cognitive impairment, and the physical illness—all of these can be expected to show up in people treated with a cocktail that often includes an antidepressant, an antipsychotic, a mood stabilizer, a benzodiazepine, and perhaps a stimulant, too. This was a medical train wreck that could have been anticipated, and unfortunately, as we trace the history of this story, the details will seem all too familiar.
Although "bipolar" illness is a diagnosis of recent origin, first showing up in the APA's Diagnostic and Statistical Manual in 1980 (DSM-III), medical texts dating back to Hippocrates contain
outcomes literature for this disorder, we need to try to understand this astonishing increase in its prevalence. fn 9
Although the quick-andeasy explanation is that psychiatry has greatly expanded the diag-nostic boundaries, that is only part of the story. Psychotropic drugs—both legal and illegal—have helped fuel the bipolar boom.
In studies of first-episode bipolar patients, investigators at McLean Hospital, the University of Pittsburgh, and the University of Cincinnati Hospital found that at least one-third had used marijuana or some other illegal drug prior to their first manic or psy-chotic episode." This substance abuse, the University of Cincinnati investigators concluded, may "initiate progressively more severe affective responses, culminating in manic or depressive episodes, that then become self-perpetuating."11 Even the one-third figure may be low; in 2008, researchers at Mt. Sinai Medical School reported that nearly two-thirds of the bipolar patients hospitalized at Silver Hill Hospital in Connecticut in 2005 and 2006 experienced their first bout of "mood instability" after they had abused illicit drugs.12 Stimulants, cocaine, marijuana, and hallucinogens were common culprits. In 2007, Dutch investigators reported that marijuana use "is associated with a fivefold increase in the risk of a first diagnosis of bipolar disorder" and that one-third of new bipolar cases in the Netherlands resulted from it.13
Antidepressants have also led many people into the bipolar camp, and to understand why, all we have to do is return to the discovery of this class of drugs. We see tuberculosis patients treated with iproniazid dancing in the wards, and while that magazine report was probably a bit exaggerated, it told of lethargic patients suddenly behaving in a manic way. In 1956, George Crane published the first report of antidepressant-induced mania, and this problem has remained present in the scientific literature ever since.14 In 1985, Swiss investigators tracking changes in the patient mix at Burgholzli psychiatric hospital in Zurich reported that the percentage with manic symptoms jumped dramatically following the introduction of antidepressants. "Bipolar disorders increased; more patients were admitted with frequent episodes," they wrote.15 In a 1993 practice guide to depression, the APA confessed that "all anti- depressant treatments, including ECT [electroconvulsive therapy],
THE BIPOLAR BOOM •
may provoke manic or hypomanic episodes."16 A few years later, researchers at Yale University School of Medicine quantified this risk. They reviewed the records of 87,290 patients diagnosed with depression or anxiety between 1997 and 2001 and determined those treated with antidepressants converted to bipolar at the rate of 7.7 percent per year, which was three times greater than for those not exposed to the drugs.17 As a result, over longer periods, 20 to 40 percent of all patients initially diagnosed with unipolar depression today eventually convert to bipolar illness.18 Indeed, in a recent survey of members of the Depressive and Manic-Depressive Association, 60 percent of those with a bipolar diagnosis said they had initially fallen ill with major depression and had turned bipolar after exposure to an antidepressant.19
This is data that tells of a process that routinely manufactures bipolar patients. "If you create iatrogenically a bipolar patient," explained Fred Goodwin, in a 2005 interview in Primary Psychiatry, "that patient is likely to have recurrences of bipolar illness even if the offending antidepressant is discontinued. The evidence shows that once a patient has had a manic episode, he or she is more likely to have another one, even without the antidepressant stimulation." fn 20, p181
Italy's Giovanni Fava put it this way: "Antidepressant-induced mania is not simply a temporary and fully reversible phenomenon, but may trigger complex biochemical mechanisms of illness deterioration."fn 21, p181
“With illegal and legal drugs greasing the road to bipolar illness, it is little wonder that a rare disorder in 1955 has become commonplace today. SSRIs took the country by storm in the 1990s, and from 1996 to 2004, the number of adults diagnosed with bipolar illness rose 56 percent. At the same time, psychiatry's steady expansion of diagnostic boundaries over the past thirty-five years has helped fuel the bipolar boom too.” p 181
When bipolar disorder was first separated from manic-depressive illness, the diagnosis required a person to have suffered bouts of mania and depression so severe that each type had resulted in hospitalization. Then, in 1976, Goodwin and others at the NIMH suggested that if a person had been hospitalized for depression but not for mania, and yet had experienced a mild episode of mania
As Moncrieff wrote in 1997, summing up lithium's record of efficacy: "There are indications that it is ineffective in the long-term outlook of bipolar disorders, and it is known to be associated with various forms of harm." fn 37
188 • ANATOMY OF AN EPIDEMIC
study," wrote Ghaemi, in an editorial that appeared in the American Journal of Psychiatry, "may be one more nail in the coffin of antidepressant use in bipolar disorder."
During the past ten years, several large studies have documented just how constantly symptomatic bipolar patients are today. In a long-term follow-up of 146 bipolar I patients who enrolled in an NIMH study in 1978-81, Lewis Judd found that they were depressed 32 percent of the time, manic or hypomanic 9 percent of the time, and suffering from mixed symptoms 6 percent of the time.48 The bipolar II patients in that study arguably fared even worse: They were depressed 50 percent of the time. "The nature of this de-ceptively 'milder' form of manic-depressive illness is so chronic as to seem to fill the entire life," Judd wrote.49 Russell Joffe, at the New Jersey Medical School, reported in 2004 that 33 percent of the bipolar I patients and 22 percent of the bipolar II patients he studied were rapid cyders, and both groups were symptomatic nearly half of the time.5° Meanwhile, Robert Post announced that nearly two-thirds of the 258 bipolar patients he studied had four or more episodes per year.51
All of these studies showed the same bottom-line result: "It is now well established that bipolar disorders are chronic, with a course characterized by frequent affective episode recurrence," Judd said.52
The Harm Done
In a 2000 paper published in the Psychiatric Quarterly, a Harvard Medical School psychiatrist, Carlos Zarate, and a psychiatrist who worked for Eli Lilly, Mauricio Tohen, opened up a new line of concern: Bipolar patients today aren't just much more symptomatic than in the past, they also don't function as well. "In the era prior to pharmacotherapy, poor outcome in mania was considered a relatively rare occurrence," Zarate and Tohen wrote. "However, modern outcome studies have found that a majority of bipolar patients evidence high rates of functional impairment." What, they wondered, could explain "these differences"? fn 53, p188
The remarkable decline in the functional outcomes of bipolar patients is easy to document. In the pre-lithium era, 85 percent of mania patients would return to work or to their "pre-morbid" social role (as a housewife, for example). As Winokur wrote in 1969, most patients had "no difficulty resuming their usual occupations." But then bipolar patients began cycling through emergency rooms more frequently, employment rates began to decline, and soon investigators were reporting that fewer than half of all bipolar patients were employed or otherwise "functionally recovered." In 1995, Michael Gitlin at UCLA reported that only 28 percent of his bipolar patients had a "good occupational outcome" at the end of five years.54 Three years later, psychiatrists at the University of Cincinnati announced that only 24 percent of their bipolar patients were "functionally recovered" at the 'end of one year.55 David Kupfer at the University of Pittsburgh School of Medicine, in a study of 2,839 bipolar patients, discovered that even though 60 percent had attended college and 30 percent had graduated, two-thirds were unemployed.% "In summary," wrote Ross Baldessarini in a 2007 review article, "functional status is far more impaired in type I bipolar patients than previously believed, [and] remarkably, there is some evidence that functional outcome in type II bipolar patients may be even worse than in type I.757
The antidepressants, by increasing the frequency of episodes that bipolar patients suffer, naturally reduce their ability to return to work. But, as has become evident in recent years, the problem runs much deeper than that. One of the hallmarks of manic-depressive illness, dating back to Kraepelin, was that once people recovered from their episodes of mania and depression, they were as smart as they had been before they became ill. As Zarate and Tohen noted in their 2000 paper, "studies conducted prior to 1975 found no consistent findings in cognitive deficits in bipolar patients." But lithium was known to slow thinking, and suddenly researchers began reassessing this belief. In 1993, NIMH investigators compared cognitive function in bipolar and schizophrenia
190 • ANATOMY OF AN EPIDEMIC
patients, and they concluded that while the bipolar patients showed signs of impairment, the deficits were "more severe and extensive in schizophrenia."'"
This was something of a glass-half-full finding. You could interpret it to mean that cognitive impairment was not that bad in bipolar patients, or, if you remembered the pre-lithium days, you might wonder why these patients were suddenly showing signs of mental decline. But this was just the beginning salvo of a tragic story. Once lithium monotherapy fell from favor, psychiatrists began to turn to "drug cocktails" to treat their patients, and soon investigators had this to report: "Cognitive impairments [that] exist in schizophrenia and affective disorders . . . cannot be qualitatively distinguished with sufficient reliability."59 The degree of impairment in these two illnesses was suddenly converging, and in 2001, Faith Dickerson at the Sheppard Pratt Health. System in Baltimore provided a more detailed picture of that convergence. She ran seventy-four medicated schizophrenia patients and twenty-six medicated bipolar patients through a series of tests that assessed forty-one cognitive and social-functioning variables, and found that the bipolar patients were as impaired as the schizophrenia patients on thirty-six of the forty-one measures. There was "a similar pattern of cognitive functioning in patients with bipolar disorder as compared to those with schizophrenia," she wrote. "On most measures of social functioning, our patients with bipolar disorder were not significantly different from those in the schizophrenia group.” 60
After that, reports of significant cognitive decline in bipolar patients seemed to pour in from psychiatric researchers around the globe—English, Swedish, German, Australian, and Spanish investigators all told of it. The Australians reported in 2007 that even when bipolar patients are only mildly symptomatic, they are "neuropsychologically scarred"—impaired in their decision-making skills, their verbal fluency, and their ability to remember things.61 Meanwhile, Spanish investigators, after noting that cognitive function in their bipolar and schizophrenia patients "did not differ over time in any test," concluded that both groups suffered from dysfunction in the "prefrontal cortex and temporolimbic structures." They also observed that "the more medications the patients received, the greater the psychosocial functioning impairment." fn 62, p190
Finally, English researchers who looked at the daily lives of bipolar patients found that more than two-thirds "rarely or never engaged in social activities with friends," their social lives nearly as impoverished as those diagnosed with schizophrenia. fn 63, p191
This was an astonishing convergence in long-term outcomes between the two diagnostic groups, and while the psychiatrists in the United States and abroad who documented it mostly tried, in their discussion of the phenomenon, to ignore the medication elephant in the room, several did confess that it was possible that psychiatric drugs were to blame. Conventional antipsychotics, said Zarate in one of his papers, "may have a negative impact on the overall course of the illness."64 Late; he and Tohen wrote that "medication induced changes may be yet another factor in explaining the discrepancies in recovery rates between earlier and more recent studies." The antidepressants, they noted, might cause a "worsening of the course of illness," while the antipsychotics might lead to more "depressive episodes" and "lower functional recovery rates." Cognitive impairment was a primary reason that medicated schizophrenia patients fared so poorly over the long term, they said, and "it has been suggested that drug side effects may in part explain the cognitive deficits in bipolar disorder patients."65 Baldessarini, in his 2007 review, also acknowledged that "neuropharmacological-neurotoxic factors" might be causing "cognitive deficits in bipolar disorder patients."
Finally, Kupfer threw one more concern into the mix. He detailed all the physical illnesses that now struck bipolar patients—cardiovascular problems, diabetes, obesity, thyroid dys-function, etc.—and wondered whether "treatment factors such as toxicity from medications" could be causing these devastating ailments, or at least contributing to them. fn 66
All of these writers put their concerns into a conditional context,
* In this study, the investigators reported that cognitive impairment, from least to most, was as follows, according to drug treatment received: lithium monotherapy, untreated, neuroleptic monotherapy, and then combination drug therapy. However, no details are given about the "untreated" group and whether they had previous exposure to psychiatric medications.
192 • ANATOMY OF AN EPIDEMIC
stating that the drugs might be causing this mental and physical deterioration in theirpatients. But it's easy to see that their hesi- tancy was scientifically unwarranted. Schizophrenia and manic-depressive illness had been diagnostically born as distinct in kind precisely because those with schizophrenia deteriorated cognitively over time, into dementia, while the manic-depressive group did not.* The convergence, in outcomes developed once both groups were treated with similar drug cocktails (which usually included an antipsychotic). "The field is witnessing a convergence of pharmacological approaches to the treatment of schizophrenia and bipolar disorder," wrote Stephen Stahl, author of Antipsychotics and Mood Stabilizers, in 2005. It was adopting "similar blended treatments for these two disease states."67 Psychiatric drugs, of course, perturb various neurotransmitter pathways in the brain, and thus once schizophrenia and bipolar patients are on similar drug cocktails, they suffer from similar abnormalities in brain function. The convergence of outcomes in the two groups reflects an iatrogenic process at work: The two groups, apart from whatever "natural" problems they may have, both end up suffering from what could be dubbed "polypharmacy psychiatric drug illness."
“Today, bipolar illness is a far cry from what it once was. Prior to the psychopharmacology era, it had been a rare disorder, affecting perhaps one in ten thousand people. Now it affects one in forty (or by some counts, one in twenty). And even though most patients today—at initial diagnosis—are not nearly as ill as the hospitalized patients of the past, their long-term outcomes are almost incomprehensibly worse.” p192 (good summary statement for book)
In his 2007 review, Baldessarini even detailed, step by step, this remarkable deterioration in outcomes. In the pre-drug
* The schizophrenia patients who routinely deteriorated into dementia were Kraepelin's dementia praecox patients. That group of patients presented with symptoms very different in kind from schizophrenia patients today, and as we saw in Martin Harrow's fifteen-year study, many unmedicated schizophrenia patients recover. Courtenay Harding reported the same thing in her long-term study—many of the unmedicated patients had completely recovered. So it's unclear what percentage of people diagnosed with schizophrenia today, if not continually medicated, would deteriorate cognitively over time.
THE BIPOLAR BOOM • 193
The Transformation of Bipolar Disorder in the Modern Era
Pre-Lithium Bipolar - . Medicated Bipolar.Today
Prevalence 1 in 5,000 to 20,000 1 in 20 to 50
Good long-term functional outcomes 75% to 90% 33%
Symptom course Time-limited acute episodes of mania and major depression with recovery to euthymia and a fav- orable functional adaptation between episodes Slow or incomplete recovery from acute episodes, con-tinued risk of recurrences, and sustained morbidity over time
Cognitive function No impairment between epiT sodes or long-term impairment Impairment even between episodes; long-term impair-ment in many cognitive domains; impairment is similar to what is observed in medicated schizophrenia
This information is drawn from multiple sources. See in particular Huxley, N."Disability and its treatment in bipolar disorder patients." Bipolar Disorders 9 (2007): 183-96.
era, there was "recovery to euthymia [no symptoms] and a favorable functional adaptation between episodes." Now there is "slow or incomplete recovery from acute episodes, continued risk of recurrences, and sustained morbidity over time." Before, 85 percent of bipolar patients would regain complete "premorbid" functioning and return to work. Now only a third achieve "full social and occupational functional recovery to their own premorbid levels." Before, patients didn't show cognitive impairment over the long term. Now they end up nearly as impaired as those with schizophrenia. This all tells of an astonishing medical disaster, and then Baldessarini penned what might be considered a fitting epitaph for the entire psychopharmacology revolution:
Prognosis for bipolar disorder was once considered relatively favorable, but contemporary findings suggest that disability and poor outcomes are prevalent, despite major therapeutic advances."
194 • ANATOMY OF AN EPIDEMIC
The Graphic That Tells It All
We are now coming to the close of our examination of the outcomes literature for the major psychiatric disorders (for adults), and a return to Martin Harrow's fifteen-year study on schizophrenia outcomes brings it to a climactic end. In addition to following schizophrenia patients, Harrow studied a group of eighty-one patients with "other psychotic disorders" that would have been described by Kraepelin as a manic-depressive cohort. There were thirty-seven bipolar and twenty-eight unipolar patients in this group, and the remaining sixteen had various milder psychotic disorders. Nearly half of this group stopped taking psychiatric medications during the study, and thus Harrow really had four groups he followed: schizophrenia patients on and off meds and manic-depressive patients on and off meds. Before we review the results, we can run a quick check of our own thoughts: How should we expect the long-term outcomes of all four groups to stack up?
Go ahead—take out a pencil and jot down what you believe the results will be.
Here are his findings. Over the long term, the manic-depressive patients who stopped taking psychiatric drugs fared pretty well. But their recovery took time. At the end of two years, they were still struggling with their illness. Then they began to improve, and by the end of the study their collective scores fell into the "recovered" category (a score of one or two on Harrow's global assessment scale). The recovered patients were working at least part-time, they had "acceptable" social functioning, and they were largely asymptomatic. Their outcomes fit with Kraepelin's understanding of manic-depressive illness.
The manic-depressive patients who stayed on their psychiatric medications did not fare so well. At the end of two years, they remained quite ill, so much so they were now a little bit worse than the schizophrenia patients off meds. Then, over the next two-andone-half years, while the manic-depressive and schizophrenia patients who were off meds improved, the manic-depressive patients who kept taking their pills did not, such that by the end of 4.5
THE BIPOLAR BOOM • 195
years, they were doing markedly worse than the schizophrenia offmed group. That disparity remained through the rest of the study, and thus here is how the long-term outcomes stacked up, from best to worst: manic-depressive off meds, schizophrenia off meds, manic-depressive on meds, and then schizophrenia on meds.69
Schizophrenia, of course, has long been the psychiatric diagnosis with the worst long-term prognosis. It is the most severe mental illness that nature has to offer. But in this NIMH-funded study, two groups of medicated patients fared worse than the unmedicated schizophrenia patients. The results tell of a medical treatment gone horribly awry, and yet they do not come as a surprise. Anyone who knew the history of the outcomes literature in psychiatry, a history that began to unfold more than fifty years ago, could have predicted that the outcomes would stack up in this way.
In terms of contributing to our modern-day epidemic of disabling mental illness, the bipolar numbers are .staggering. In 1955, there were about 12,750 people hospitalized with bipolar illness. Today, according to the NIMH, there are nearly six million adults in the
15-Year Outcomes for Schizophrenia and Manic-Depressive Patients
In this graphic, the group labeled "manic depressive" consisted of psychotic patients with bipolar illness, unipolar depression, and milder psychotic disorders. Source: Harrow, M."Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications!' The Journal of Nervous and Mental Disease, 195 (2007): 406-14.
5 4 3 2 1
0
Best outcomes
2
Year
Follow-up
4.5 7.5
Year Year
Follow-up Follow-up
Schizophrenia On Meds Manic-
Depressive On Meds
Schizophrenia Off Meds
Manic-Depressive Off Meds
Worst outcomes
7
6
10
Year
Follow-up
Global Assessment Scale
15
Year
Follow-up
196 • ANATOMY OF AN EPIDEMIC
United States with this diagnosis, and according to researchers at the Johns Hopkins School of Public Health, 83 percent are "severely impaired" in some facet of their lives.70 Bipolar illness is now said to be the sixth leading cause of medical-related disability in the world, right behind schizophrenia, and in the near future, as more and more people are diagnosed with this condition and put on drug cocktails, we can expect that bipolar will climb past schizophrenia and take its place behind major depression as the mental illness that fells the most people in the United States. Such is the fruit, bitter in kind, born from the psychopharmacology revolution.
Bipolar Narratives
I interviewed more than sixty people with psychiatric diagnoses for this book, and roughly half at some point had been diagnosed as bipolar. Yet of the thirty or so who got that diagnosis, only four suffered from what might be called "organic" bipolar illness, and that is to say they were hospitalized for a manic episode and had no prior exposure to illicit drugs or antidepressants. Now that we know what science has to tell us about the modern bipolar boom, we can revisit the stories of three people we met in Chapter 2, and see how their stories fit into that story of science. Then we can hear from two people diagnosed with 'bipolar who, if they had been enrolled in Harrow's fifteen-year study, would have fallen into his "off-meds" group.
Dorea Vierling-Clausen
If we look at Dorea Vierling-Clausen's story now, we can see that she has good reason to believe that she should never have been diagnosed with bipolar illness. She went to see a therapist in Denver because she cried too much. She had no history of mania. But then she was prescribed an antidepressant and starting having trouble sleeping, and soon she had a bipolar diagnosis and a prescription for a drug cocktail that included an antipsychotic. A bright teenager
THE BIPOLAR BOOM • 197
had been turned into a mental patient, and Dorea would have continued to be one for the rest of her life if she had not weaned herself from the drugs. When I last spoke to her, in the spring of 2009, she was aglow with the blush of motherhood, as she had recently given birth to a son, Reuben. She and Angela were busily raising their children, with Dorea planning shortly to resume her postdoctoral research at Massachusetts General Hospital, the memory of her "bipolar" days receding into an ever-more-distant past.
Monica Briggs
During the time that I worked on this book, Monica Briggs was the one person who, after an initial interview, got off SSDI (or SSI). She secured a full-time position with the Transformation Center, a peer-run organization in Boston that focuses on helping people "recover" from mental illness, and if you parse her medical story, it's easy to see that her return to work was related to a change in her medication.
When we first met, I mentioned to Monica the risk of antidepressant-induced mania, and as she remembered back to her breakdown at Middlebury College, a light went on: "I got manic within six weeks of being put on desipramine," she said. "I'm sure that's what happened to me." After that initial manic episode, she was prescribed a drug cocktail that included an antidepressant, and she spent the next twenty years cycling in and out of hospitals, struggling constantly with depression, manic episodes, and suicidal impulses. Psychiatrists put her on eight or nine different antidepressants, and she also went through a series of electroshock treatments. None of this worked. Then, in 2006, she "casually" stopped taking an antidepressant. For the first time, she was on lithium alone, and bingo—the suicidal feelings went away, as did the depression and mania. That symptom relief is what enabled her to work full-time, and now, as she looks back on the horrible twenty years, she is stunned by what she sees: "I have not yet recovered from the immensity of the likelihood that my roulette game with antidepressants exacerbated my illness."
198 • ANATOMY OF AN EPIDEMIC
Steve Lapp en
Steve Lappen, who is a leader of the Depressive and Bipolar Support Alliance in Boston, was diagnosed with manic-depressive illness in 1969, when he was nineteen years old. He was one of the four people I interviewed whose manic-depressive illness was "organic" in kind, and on the first day we met, he was in something of a hyper state, talking so fast that I quickly put my pen away and took out a tape recorder instead. "OK," I told him, "fire away."
Raised in Newton, Massachusetts, in a family he describes as dysfunctional, Steve got tagged with the "bad apple" label early in life, both by his teachers at school and his parents at home. "I was disruptive in class," he says. "Every day, during the pledge of alle-giance to the flag, I would go sharpen my pencil. I would also get up without provocation and just spin around until I was overcome with dizziness. I would announce that I was a tornado." He struggled with mood swings even as a kid, and at age sixteen, while hos-pitalized for fainting spells, he jumped out of bed one night and donned a white coat. "I went around to patient rooms and had conversations as if I were a doctor. I was manic."
During his first year at Boston College, he was hit by a bout of severe depression. His was a classic case of true manic-depressive illness, and Kraepelin would have recognized the course his illness took over the next five years. "I didn't take medication," he explains, and while he suffered several bouts of depression, he did well in between those episodes, particularly when he was in a slightly hypomanic state. "When I was feeling well, I would read more, and I would write papers that weren't due for two or three months," he says. "When you are hypomanic, your output is remarkable." He graduated with a double major in philosophy and English, with nearly a straight-A average.
However, in his first year of graduate school at Stony Brook in Long Island, he had a full-blown manic episode followed by a plunge into depression that left him suicidal. It was then that he was put on lithium and a tricyclic antidepressant for the first time. "I didn't have mood swings after that, but instead of having a baseline of functioning normally, I was depressed. I was in a state of depres-
THE BIPOLAR BOOM • 199
sion the entire time I was on the medication. I stayed on it for a year and said, 'No more.' "
Over the next two decades, Steve mostly stayed away from psychiatric medications. He married, had two sons, and divorced. He worked, but skipped from job to job. His life was proceeding down a chaotic path, a chaos that was clearly related to his manic-depressive illness, and yet his life was not marked by vocational disability—he always found work.
In 1994, seeking relief from the mood swings that plagued him, he [Steve Lappen] began taking psychiatric medications regularly. He cycled through an endless number of anti-depressants and mood stabilizers, none of which worked for long. Those drug failures led to fourteen electroshock treatments, which in turn left his memory so impaired that when he returned to his job as a financial planner, "I could no longer recognize my best client." p199
In 1998, he was put on the tricyclic desipramine, which promptly turned him into a rapid cycler. "I'd wake up and feel great, completely emancipated from the demon of depression, and then two days later, I am back into depression," he explains. "Two days after that, I'm feeling well again. And there is nothing in my external environment that would account for that change in mood."
He has been on SSDI ever since. The good news is that he hasn't been hospitalized since 2000, and, as he rightly points out, in spite of his constant battle with bipolar symptoms, he leads a productive life. Remarried now, he volunteers as a "reader" for people who are physically disabled, gives talks about bipolar illness to community groups, and is one of the leaders of DBSA Boston. He also has published essays and poetry in various small publications. But when I last spoke to him, in the spring of 2009, he was cycling through multiple mood swings every day, his symptoms apparently continuing to worsen.
"I would say in the main, I have been worse when taking medication. The medication I am taking now is neutral at best. I wish I could clone myself. I could be my own control group in a trial. I'd like to know if I'd be better, the same, or worse without it."
200 • ANATOMY OF AN EPIDEMIC
Brandon Banks
Brandon Banks can identify the precise moment he became "bipolar," and while it did involve an antidepressant, there was a series of life events that led up to it. He grew up poor in Elizabethtown, Kentucky, without a father at home, and he has painful memories of sexual abuse, physical abuse, and of a horrible car wreck that killed his aunt, uncle, and another relative. At school, other kids regularly taunted him about a facial birthmark, which so traumatized him that he began wearing a hat pulled low on his head to cover it up. After graduating from high school in 2000, he moved to Louisville, where he went to college part-time and worked nights at United Parcel Service. Soon he noticed that he "wasn't feeling right," and when he went back home, his family doctor diagnosed him with "moderate depression" and prescribed an antidepressant. "I went manic in three days," Brandon says. "It was fast."
His doctor explained that since he'd had that reaction to the drug, he must be bipolar, rather than just depressed. The drug had "unmasked" the illness, which Brandon took as a positive thing. "I'm thinking, This isn't so bad, I could have stayed in the system a long time without getting immediate confirmation that I'm bipolar like that." He was put on a cocktail composed of a mood stabilizer, an antidepressant, and an antipsychotic, and then it hit him. "This was a serious shove into seriousness."
Over the next four years, his psychiatrists constantly changed his prescriptions. "It was like musical chairs with the cocktails," he says. "They would tell me, 'Let's take this drug out and put this one in.' " He took Depakote, Neurontin, Risperdal, Zyprexa, Seroquel, Haldol, Thorazine, lithium, and an endless succession of antidepressants, and as time went on he became a rapid cycler who suffered from mixed states. His medical records also document the development of new psychiatric symptoms: worsening anxiety, panic at-tacks, obsessive-compulsive behaviors, voices, hallucinations. He was hospitalized several times, and at one point he climbed up on top of a parking garage and threatened to jump off. His ability to concentrate declined so severely that Kentucky took away his driver's license. "What my life became was staying at home all day, get-
THE BIPOLAR BOOM • 201
ting up in the morning and laying my pills out on the counter, taking them, and then going back to sleep because I couldn't stay awake if I tried. Then I would get up, play some video games, and hang out with my family."
Twenty-four years old, he felt like a total failure, and one day, after a fight with his mother, he moved out and stopped taking his meds. "I deteriorated badly," he recalls. "I wasn't bathing and I wasn't eating." However, as the weeks turned into months, his bipolar symptoms lessened, and "I began to think that it's more like I'm just fucked up," he says. This was a thought that gave him hope, because now there was the possibility of change, and he took off traveling around the South. "I might as well be homeless," he told himself, and that journey ultimately turned into a transformative experience. By the time he returned home, he had sworn off eating meat and drinking alcohol, on his way to becoming a "health freak" who practices yoga. "I came back from that trip, and man, I was on top of it. I felt like a million dollars, and everyone in my family—cousins, relatives, aunts and uncles—said that they hadn't seen me glow like this since I was a kid."
Since then, Brandon has stayed off psychiatric medications. But it hasn't been easy, and the up-and-down nature of his life came into sharp relief during his 2008-2009 year at Elizabethtown Community and Technical College. He enrolled there in January of 2008 with dreams of becoming a journalist and a writer, and in the fall, he became managing editor of the school's newspaper. Under his leadership, the newspaper won twenty-four awards from the Kentucky Intercollegiate Press Association during the 2008-2009 year, and Brandon personally garnered ten such honors for the articles he'd written, including first place in a deadline-writing competition. Incredibly, during those nine months, Brandon racked up other successes too. One of his short stories won second place in a competition and was published in a Louisville weekly; one of his photos was picked as cover art for a literary journal; a short film he shot was nominated for a best documentary award in a local film festival. In May of 2009, his school honored him with its "outstanding sophomore" award. Yet, even during this season of remarkable accom-plishment, Brandon suffered several hypomanic and depressive
202 • ANATOMY OF AN EPIDEMIC
episodes that left him feeling deeply suicidal. "I spent several weekends reading depressive authors with a gun in my hand," he says. "My accomplishments at these moments just seem to make everything worse. It never seems like enough."
That is where matters stood in his life in the summer of 2009. He was thriving and struggling at the same time, and his struggles were such that if psychiatric medications had worked for him the first time, he would gladly have turned to them for relief. "I'm still pretty isolated from other people," he explains. "I stick out because of the birthmark. I'm different. I can't blend in. It becomes an issue with people. But I'm trying to integrate myself more into life. I have more people in my life now than I have had in a long time. I'm starting to make more contacts. I had lunch with a friend the other day. Doing this is hard for me, and that's because it's just not easy for me to deal with people and deal with my emotions. I am trying to get better at it."
Greg
A math and science whiz, Greg, who asked that I not use his last name, was the sort of child who, when he was in junior high, built a Van de Graaff generator from scrounged parts (which included a vacuum cleaner and a salad bowl, to be precise). However, he had a troubled relationship with his parents, and at the start of his senior year, he began to slide into a mad state (and without having used illegal drugs). "I was delusional, very paranoid, and full of anxiety," he says. "I was convinced that my parents were trying to kill me."
Hospitalized for six weeks, Greg was told he was schizoaffective with bipolar tendencies (a "manic-depressive" type diagnosis), and he was discharged on a cocktail composed of two antipsychotics and an antidepressant. But the drugs didn't chase away his paranoid thoughts, and after he was hospitalized a second time, his psychiatrists added a mood stabilizer and a benzodiazepine to the cocktail and told him he needed to give up his scholastic dreams. "They told me I would be on medication for the rest of my life, and that I would probably be a ward of the state, and that maybe, by the time I was twenty-five or thirty, I could think about getting a part-time
THE BIPOLAR BOOM • 203
job. And I believed it, and so I began trying to figure out how to live with the crushing hopelessness that they are telling you is going to be your life."
The next five years passed pretty much as his psychiatrists had predicted. Although Greg entered Worcester Polytechnic Institute (WPI) in Massachusetts, he was so heavily medicated that, he says, "I was living in a haze most of the time. Your mind is just a bag of sand. And so I did really poorly in school. I rarely even left my room, and I was kind of out of touch with reality." He petered along in school for a couple of years, not really making much progress, and then, from 2004 to 2006, he dropped out and mostly stayed in his apartment, smoking marijuana constantly, as "it helped me accept the condition I was forced into." Six feet, five inches tall, Greg's weight went from 255 pounds to nearly 500 pounds. "Finally, I said to myself, this is ridiculous. I'd rather be crazy and have a life than not be crazy and not have a life."
“The next five years passed pretty much as his psychiatrists had predicted. Although Greg entered Worcester Polytechnic Institute (WPI) in Massachusetts, he was so heavily medicated that, he says, "I was living in a haze most of the time. Your mind is just a bag of sand. And so I did really poorly in school. I rarely even left my room, and I was kind of out of touch with reality." … He [Greg] went for a medical checkup, thinking this would be a first step toward reducing his medications, only to be informed that he needed to stop taking Depakote and Geodon right away, as his liver was shutting down. The abrupt withdrawal induced such physical pain—"sweats, joint and muscle pain, nausea, dizziness," he says—that he didn't even pay attention to whether his paranoia was coming back. But in very short order, he was off all of his psychiatric drugs, except for occasional use of a stimulant, and he had also stopped smoking marijuana. "Honestly, it felt like I was waking up for the first time in five years," he says. "It felt like I had been turned off all those years and had just been rolling through life and I was being pushed around in a wheelchair and finally I had woken up and had gotten back to being myself again. I felt like the drugs took away everything that was me, and then when I went off the drugs, my brain woke up and started working again."” p 202
In late 2007, Greg went back to school. We met in the spring of 2009, and after he had told me the story of his bout with mental illness, he showed me around his research laboratory at WPI, where he now spent eighty hours a week, designing and constructing a robot capable of conducting brain surgery inside an MRI. In a few weeks, he would receive an undergraduate degree in mechanical en-
204 • ANATOMY OF AN EPIDEMIC
gineering, and since he'd entered a master's program while still doing undergraduate work, later that summer he would receive a master's degree in mechatronics, which is a fusion of mechanical and electrical engineering. The day before my visit, his robotics research had won second prize in a competition that featured 187 entries by graduate students at WPI. Already he had published three papers in academic journals on his project, and in a few weeks he was scheduled to fly to Japan to give a talk about it. He was doing this project under the guidance of a WPI professor, and they expected to conduct animal and cadaver trials with the robot in the fall of 2009. If all went well, clinical trials with humans would begin in two years.
While in his laboratory, Greg showed me the robot and the computer drawings of its circuit boards, which seemed impossibly complex.
Naturally, I thought of John Nash, the Princeton mathematician whose inspiring story of recovering from schizophrenia, and doing so while off medication, was told in the book A Beautiful Mind.
"I still feel that I have some bad habits to get out of and some better habits to get into before I get into the professional life, but I really do feel that I have left that [mentally ill] part of my life behind," says Greg, who has lost more than one hundred pounds. "Honestly, I almost never think of it. I now think of myself as a person who is susceptible to building anxiety, but when I start feeling this anxiety, or start feeling negative about things, I stop and say to myself, 'Are these really reasonable feelings to feel, or is it just insecurity?' I just have to take the time to check myself." He is, he concluded, "pretty optimistic about my future now."
I 0
An Epidemic Explained
"With psychiatric medications, you solve one
problem for a period of time, but the next thing you
know you end up with two problems. The treatment
turns a period of crisis into a chronic mental illness."
-AMY UPHAM (2009 fn 1)
There is a famous optical illusion called the young lady and the old hag, and depending on how you look at it, you see either a beautiful young woman or an old witch. The drawing illustrates how one's perception of an object can suddenly flip, and in a sense, the dueling histories that we have fleshed out in this book have that same curious quality. There is the "young woman" picture of the psycho-pharmacology era that most of American society believes in, which tells of a revolutionary advance in the treatment of mental disorders, and then there is the "old hag" picture that we have sketched out in this book, which tells of a form of care that has led to an epidemic of disabling mental illness.
The young-lady picture of the psychopharmacology era arises from a powerful combination of history, language, science, and clinical experience.
Prior to 1955, history tells us, the state mental hospitals Were bulging with raving lunatics. But then researchers discovered an antipsychotic medication, Thorazine, and that drug made it possible for the states to close their decrepit hospitals and to treat schizophrenics in the community. Next, psychiatric researchers discovered anti-anxiety agents, antidepressants, and a magic bullet—lithium--for bipolar disorder. Science then proved that the drugs worked: In clinical trials, the drugs were found to ameliorate a target symptom over the short term better than placebo. Finally, psychiatrists regularly saw that their drugs were effective. They gave them to their distressed patients, and their symptoms often abated. If their patients stopped taking the drugs, their symptoms frequently returned. This clinical course—initial symptom reduction and relapse upon drug withdrawal—also gave patients reason to say: "I need my medication. I can't do well without it." p 206
Young or old woman? If you shift your eyes slightly, your perception of the image will change from one to the other. Courtesy of Exploratorium.
The old-hag picture of the psychopharmacology era arises from a more careful reading of history and a more thorough review of the science. When we reviewed the history of deinstitutionalization, we found that the discharge of chronic schizophrenia patients resulted from the enactment of Medicare and Medicaid legislation in the mid-1960s, as opposed to from Thorazine's arrival in asylum medicine. As for the drugs, we discovered that there was no scientific breakthrough that led to the introduction of Thorazine and other first-generation psychiatric medications. Instead, scientists studying compounds for use as anesthetics and as magic bullets for infectious
AN EPIDEMIC EXPLAINED • 207
diseases stumbled upon several agents that had novel side effects. Then, over the course of the next thirty years, researchers determined that the drugs work by perturbing the normal functioning of neuronal pathways in the brain. In response, the brain undergoes "compensatory adaptations" to cope with the drug's mucking up of its messaging system, and this leaves the brain functioning in an "abnormal" manner. Rather than fix chemical imbalances in the brain, the drugs create them. We then combed through the outcomes literature, and we found that these pills worsen long-term outcomes, at least in the aggregate. Researchers even put together biological explanations for why the drugs had this paradoxical long-term effect.
Those are the dueling visions of the psychopharmacology era. If you think of the drugs as "anti-disease" agents and focus on short-term outcomes, the young lady springs into sight. If you think of the drugs as "chemical imbalancers" and focus on long-term outcomes, the old hag appears. You can see either image, depending on where you direct your gaze.
A Quick Thought Experiment
Just for a moment, before we examine whether we have solved the puzzle that we set forth in the opening of this book, here is a quick way to see the old-hag picture a bit more clearly. Imagine that a virus suddenly appears in our society that makes people sleep twelve, fourteen hours a day. Those infected with it move about somewhat slowly and seem emotionally disengaged. Many gain huge amounts of weight—twenty, forty, sixty, and even one hundred pounds. Often, their blood sugar levels soar, and so do their cholesterol levels. A number of those struck by the mysterious illness—including young children and teenagers—become diabetic in fairly short order. Reports of patients occasionally dying from pancreatitis appear in the medical literature. Newspapers and magazines fill their pages with accounts of this new scourge, which is dubbed metabolic dysfunction illness, and parents are in a panic over the thought that their children might contract this horrible disease. The federal government gives hundreds of millions of dollars to scientists at the best universities to decipher the inner workings of this virus, and they report that the reason it causes such global dysfunction is that it blocks a multitude of neurotransmitter receptors in the brain—dopaminergic, serotoninergic, muscarinic, adrenergic, and histaminergic. All of those neuronal pathways in the brain are compromised. Meanwhile, MRI studies find that over a period of several years, the virus shrinks the cerebral cortex, and this shrinkage is tied to cognitive decline. A terrified public clamors for a cure. Now such an illness has in fact hit millions of American children and adults. We have just described the effects of Eli Lilly's bestselling antipsychotic, Zyprexa. A Mystery Solved. , p208
Entitlement trap, expanding diagnostic boundaries, drugs cause debilitation
We began this book by raising a question: Why have we seen such a sharp increase in the number of disabled mentally ill in the United States since the "discovery" of psychotropic medications? At the very least, I think we have identified one major cause. In large part, this epidemic is iatrogenic in kind.
Now there may be a number of social factors contributing to the epidemic. Our society may be organized in a way today that leads to a great degree of stress and emotional turmoil. For instance, we may lack the close-knit neighborhoods that help people stay well. Relationships are the foundation of human happiness, or so it seems, and as Robert Putnam wrote in 2000, we spend too much time "bowling alone." We also may watch too much television and get too little exercise, a combination that is known to be a prescription for becoming depressed. The food we eat—more processed foods and so on—might be playing a role too. And the common use of illicit drugs—marijuana, cocaine, and hallucinogens—has clearly contributed to the epidemic. Finally, once a person goes on SSI or SSDI, there is a tremendous financial disincentive to return to work.
AN EPIDEMIC EXPLAINED • 209
People on disability call it the "entitlement trap." Unless they can get a job that pays health insurance, they will lose that safety net if they go back to work, and once they start working, they may lose their rent subsidy, too.
However, in this book, we have been focusing on the role that psychiatry and its medications may be playing in this epidemic, and the evidence is quite clear. First, by greatly expanding diagnostic boundaries, psychiatry is inviting an ever-greater number of children and adults into the mental illness camp. Second, those so diagnosed are then treated with psychiatric medications that increase the likelihood they will become chronically ill. Many treated with psychotropics end up with new and more severe psychiatric symptoms, physically unwell, and cognitively impaired. That is the tragic story writ large in five decades of scientific literature.
The record of disability produced by psychiatric medications can be easily summarized. With schizophrenia, in the decade prior to the introduction of Thorazine, roughly 70 percent of people suffering a first episode of psychosis were discharged from the hospital within eighteen months, and the majority didn't return to the hospital during fairly lengthy follow-up periods. Researchers in the postThorazine era reported similar results for unmedicated patients. Rappaport, Carpenter, and Mosher all found that perhaps half of those diagnosed with schizophrenia would do fairly well if they were not continuously medicated. But that is now the standard of care, and as Harrow's study showed, only 5 percent of medicated patients recover over the long term. Today, there are an estimated 2 million adults disabled by schizophrenia in the United States, and this disability number could perhaps be halved if we adopted a paradigm of care that employed antipsychotic medications in a selective, cautious manner.
With the affective disorders, the iatrogenic effects of our drug-based paradigm of care are even more apparent. Anxiety used to be viewed as a mild disorder, one that rarely required hospitalization. Today, 8 percent of the younger adults on the SSI and SSDI roles due to a psychiatric disability have anxiety as a primary diagnosis. Similarly, outcomes for major depression used to be good. In 1955, there were only thirty-eight thousand people hospitalized with de-
2I0 • ANATOMY OF AN EPIDEMIC
pression, and the illness could be expected to remit. Today, major depression is the leading cause of disability in the United States for people fifteen to forty-four years old. It is said to strike 15 million adults, and according to researchers at Johns Hopkins School of Public Health, 60 percent are "severely impaired." As for bipolar disorder, an extremely rare illness has become a common one. According to the NIMH, nearly 6 million adults suffer from it today. Whereas 85 percent of those struck by it used to recover and go back to work, now only about a third of bipolar patients function this well, and over the long term those bipolar patients who reliably take their medications end up nearly as impaired as those with schizophrenia who stay on neuroleptics. The Johns Hopkins investigators concluded that 83 percent are "severely impaired."
In sum, there were fifty-six thousand people hospitalized with anxiety and manic-depressive illness in 1955. Today, according to the NIMH, at least 40 million adults suffer from one of these affective disorders.
More than 1.5 million people are on SSI or SSDI because they are disabled by anxiety, depression, or bipolar illness, and, according to the Johns Hopkins data, more than 14 million people who have these diagnoses are "severely impaired" in their ability to function in society. That is the astonishing bottom-line result produced by a medical specialty that has dramatically expanded diagnostic boundaries in the past fifty years and treated its patients with drugs that perturb normal brain function. p 210
Moreover, the epidemic continues its march. In the eighteen months it took me to research and write this book, the Social Security Administration released its 2007 reports for its SSI and SSDI programs, and the numbers were as expected. There were 401,255 children and adults under sixty-five years old added to the SSI and SSDI rolls in 2007 because of a psychiatric disability. Imagine a large auditorium filling up every day with 250 children and 850 adults newly disabled by mental illness, and you get a visual sense of the horrible toll exacted by this epidemic.
AN EPIDEMIC EXPLAINED • 211
Physical Illness, Cognitive Impairment, and Early Death
Fleshing out the nature of a disease usually involves identifying all the symptoms that may develop, and then following their course over time. In the previous chapters, we mostly focused on studies that showed that psychiatric medications worsen target symptoms over the long run, and only briefly noted that the drugs may cause physical problems, emotional numbing, and cognitive impairment. This is also a form of care that leads to early death. The seriously mentally ill are now dying fifteen to twenty-five years earlier than normal, with this problem of early death having become much more pronounced in the past fifteen years.2 They are dying from cardiovascular ailments, respiratory problems, metabolic illnesses, diabetes, kidney failure, and so forth—the physical ailments tend to pile up as people stay on antipsychotics (or drug cocktails) for years on end.'
Here are three stories that bear witness to these various longterm risks.
Amy Upham
Amy Upham lives in a small one-bedroom apartment in Buffalo, and as I enter the living room, she points to a table cluttered with papers. "This is me on psychiatric drugs," she says and hands me a stack of medical documents. They tell of a drug-induced swelling of the brain, faltering kidneys, a swollen liver, a swollen gallbladder, thyroid problems, gastritis, and cognitive abnormalities. A little over five feet tall, with frizzy reddish brown hair, Amy, who is thirty years old, weighs ninety pounds. She squeezes a fold of loose skin near her elbow, the muscle underneath having wasted away. "This is like what you see with heroin users."
Amy first took a psychiatric medication at age sixteen when she contracted Lyme disease and suffered a bout of depression. Twelve years later, she was still on antidepressants, and as she reviews that history, she identifies several instances when the drugs stirred
214 • ANATOMY OF AN EPIDEMIC
says, shaking her head at the memory. "It caused vasoconstriction in my brain, and this caused brain damage. I ended up in a wheelchair, and I couldn't think, speak, or walk. Those centers of the brain need a lot of juice."
Since then, her life has had its ups and downs. She takes comfort in her volunteer work with M-Power, the Boston peer advocacy group, and in the spring of 2008, she was working sixteen hours a week for Advocates, Inc., which provides services to the deaf. But she also has battled ovarian cancer, and it's possible that illness was related to the psychiatric medications. She does find such drugs useful today, but when she looks back at her life, she sees a paradigm of care that utterly failed her. "It's really a travesty," she says.
Scott Sexton
In the spring of 2005, Scott Sexton received his MBA from Rice University. A bright future lay ahead at that moment, but then he broke up with the woman he had intended to marry, and he was hospitalized for depression. This was his second bout of major de-pression (he'd suffered a first episode five years earlier, when his parents divorced), and since Scott's father had suffered from bipolar illness, he was now diagnosed with that disorder. He was put on a cocktail that included Zyprexa.
That fall, he began working as a consultant for Deloitte, the big accounting firm. Although his first few months on the job went fine, by early 2006 he was sleeping twelve to sixteen hours a day, zonked out by the Zyprexa. He soon needed another pill to get up in the morning, and he began "putting on weight like gangbusters," his mother, Kaye, recalls. "He was five feet, ten inches tall and he went from 185 pounds to 250 pounds. He had a beer belly, and his cheeks looked like he was a chipmunk. We knew that Zyprexa caused weight gain, and he was alarmed, and so was I."
By the fall of 2006, Scott was sleeping so much that on weekends he wouldn't get up until the afternoon. He stopped going into the office and told Deloitte he was working from home. On Thanksgiving, he called his mother to tell her that he was suffering severe stomach pains, and the next day he was admitted to St. Luke's
AN EPIDEMIC EXPLAINED • 215
Episcopal Hospital in Houston. His mother flew in from Midland. "Scott is beet red, he's sweating, and his hands are so swollen that they have trouble getting his ring off. He is burning up, and his [laboratory] tests are wacko. They are off the wall. His cholesterol is sky-high. His triglycerides are off the charts."
Scott's pancreas was shutting down. Zyprexa was known to cause pancreatitis, but the doctors at St. Luke's didn't connect the dots. They kept Scott on that drug until his death on December 7. "I had always told him to take his meds," his mother says. "I said, `Scott, if I ever find out you are off your meds, I will come to Houston and shoot you.' That's what I said to him. And here he is doing everything he thinks he needs to do to be functional in our society, to be a productive member of society, and it kills him."
220 • ANATOMY OF AN EPIDEMIC
dysfunction" was small. However, psychiatry's use of Ritalin slowly began to climb during the 1970s, such that by the end of the decade perhaps 150,000 children in the United States were taking the drug. Then, in 1980, the field published a third edition of its Diagnostic and Statistical Manual (DSM-III), and it identified "attention-deficit disorder" as a disease for the first time. The cardinal symptoms were "hyperactivity," "inattention," and "impulsivity," and given that many children fidget in their seats and have trouble paying attention in school, the diagnosis of ADD began to take off. In 1987, psychiatry further loosened the diagnostic boundaries, renaming it attention-deficit/hyperactivity disorder in a revised edition of DSMIII. Next, Ciba-Geigy helped fund Children and Adults with Attention Deficit Hyperactivity Disorder (CHADD), a "patient-support group" that immediately began promoting public awareness of this "disease." Finally, in 1991, CHADD successfully lobbied Congress to include ADHD as a disability that would be covered by the Individuals with Disabilities Education Act. Children diagnosed with ADHD were now eligible for special services, which were to be funded with federal money, and schools regularly began identifying children who seemed to have this condition. As the Harvard Review of Psychiatry noted in 2009, even today the diagnosis of ADHD arises primarily from teacher complaints, as "only a minority of children with the disorder exhibit symptoms during a physician's office visit."8
Suddenly, ADHD children could be found in every classroom. The number of children so diagnosed rose to nearly 1 million in 1990, and more than doubled over the next five years. Today, perhaps 3.5 million American children take a stimulant for ADHD, with the Centers for Disease Control reporting in 2007 that one in every twenty-three American children four to seventeen years old is so medicated. This prescribing practice is mostly a U.S. phenomenon—children here consume three times the quantity of stimulants consumed by the rest of the world's children combined.
Although the public often hears that research has shown that ADHD is a "brain disease," the truth is that its etiology remains unknown. "Attempts to define a biological basis for ADHD have been consistently unsuccessful," wrote pediatric neurologist Gerald Golden in 1991. "The neuroanatomy of the brain, as demonstrated by imaging studies, is normal. No neuropathologic substrate has been demonstrated." fn 9 p 220
Seven years later, a panel of experts convened by the National Institutes of Health reiterated this same point: "After years of clinical research and experience with ADHD, our knowledge about the cause or causes of ADHD remains largely speculative." fn 10
During the 1990s, CHADD advised the public that children with ADHD suffered from a chemical imbalance, characterized by an underactive dopamine system, but that was simply a drug-marketing claim. Ritalin and other stimulants increase dopamine levels in the synaptic cleft, and thus CHADD was attempting to make it seem that such drugs "normalized" brain chemistry, but, as the
American Psychiatric Press's 1997 Textbook of Neuropsychiatry confessed, "efforts to identify a selective neurochemical imbalance [in ADHD children] have been disappointing." fn 11
So we see in this history that nothing new was discovered that told of a "mental illness" called ADHD. There was a long record of speculation within medicine that extremely hyperactive children suffered from brain dysfunction of some kind, which was certainly a reasonable thought, but the nature of that dysfunction was never discerned, and then, in 1980, psychiatry simply created, with a stroke of its pen in DSM-III, a dramatically expanded definition of "hyperactivity." The fidgety seven-year-old boy who might have been dubbed a "goof-off" in 1970 was now suffering from a psychiatric disorder.
Given that the biology of ADHD remains unknown, it is fair to say that Ritalin and other ADHD drugs "work" by perturbing neurotransmitter systems. Ritalin could best be described as a dopamine reuptake inhibitor. At a therapeutic dose, it blocks 70 percent of the "transporters" that remove dopamine from the synaptic cleft and bring it back into the presynaptic neuron. Cocaine acts on the brain in the same way. However, methylphenidate clears much more slowly from the brain than cocaine does, and thus it blocks dopamine reuptake for hours, as opposed to cocaine's relatively brief disruption of this function."
* The fact that cocaine is so short-acting is why it is more addictive than
methylphenidate, for as soon as it leaves the brain, the addict may want to
222 • ANATOMY OF AN EPIDEMIC
In response to methylphenidate, the child's brain goes through a series of compensatory adaptations. Dopamine is now remaining in the synaptic cleft too long, and so the child's brain dials down its dopamine machinery. The density of dopamine receptors on the postsynaptic neurons declines. At the same time, the amount of dopamine metabolites in the cerebrospinal fluid drops, evidence that the presynaptic neurons are releasing less of it. Ritalin also acts on serotonin and norepinephrine neurons, and that causes similar com-pensatory changes in those two pathways. Receptor densities for serotonin and norepinephrine decline, and the output of those two chemicals by presynaptic neurons is altered as well.
The child's brain is now operating, as Steven Hyman said, in a manner that is "qualitatively as well as quantitatively different from the normal state." fn 12
Now we can turn our attention to the outcomes data. Does this treatment help children diagnosed with ADHD over the long term? What does the scientific literature show?
Passive, Sitting Still, and Alone
Ritalin and other ADHD drugs do reliably change a child's behavior, and in his 1937 report, Charles Bradley set the stage for the efficacy story that eventually emerged: "Fifteen of the thirty children responded to Benzedrine by becoming distinctly subdued in their emotional responses. Clinically in all cases this was an improvement from the social viewpoint."13 Ritalin, which the FDA approved for use in children in 1961, was found to have a similar subduing effect. In a 1978 double-blind study, Ohio State University psychologist Herbert Rie studied twenty-eight "hyperactive" children for three months, half of whom were prescribed methylphenidate. Here is what he wrote:
experience again the "rush" that comes when dopaminergic pathways are first sent into a hyperactive state.
“Children who were retrospectively confirmed to have been on active drug treatment appeared, at the times of evaluation, distinctly more bland or "flat" emotionally, lacking both the age-typical variety and frequency of emotional expression. They responded less, exhibited little or no initiative or spontaneity, offered little indication of either interest or aversion, showed virtually no curiosity, surprise, or pleasure, and seemed devoid of humor. Jocular comments and humorous situations passed unnoticed. In short, while on active drug treatment, the children were relatively but unmistakably affectless, humorless, and apathetic. fn 14 (. In a 1978 double-blind study, Ohio State University psychologist Herbert Rie studied twenty-eight "hyperactive" children for three months, half of whom were prescribed methylphenidate.)
Numerous investigators reported similar observations.
Children on Ritalin show "a marked drug-related increase in solitary play and a corresponding reduction in their initiation of social interactions," announced Russell Barkley, a psychologist at the Medical College of Wisconsin, in 1978. fn 15
This drug, observed Bowling Green State University psychologist Nancy Fiedler, reduced a child's "curiosity about the environment."fn 16
At times, the medicated child "loses his sparkle," wrote Canadian pediatrician Till Davy in 1989.fn 17
Children treated with a stimulant, concluded a team of UCLA psychologists in 1993, often become "passive, submissive" and "socially withdrawn." fn 18
Some children on the drug "seem zombie-like," noted psychologist James Swanson, director of an ADHD center at the University of California, Irvine.fn 19
Stimulants, explained the editors of the Oxford Textbook of Clinical Psychophamacology and Drug Therapy, curb hyperactivity by "reducing the number of behavioral responses."2°
All of these reports told the same story. On Ritalin, a student who previously had been an annoyance in the classroom, fidgeting too much in his or her chair or talking to a nearby classmate while the teacher scribbled on the blackboard, would be stilled. The student wouldn't move around as much and wouldn't engage as much socially with his or her peers. If given a task like answering arithmetic problems, the student might focus intently on it. Charles Bradley thought this change in behavior was "an improvement from the social viewpoint," and it is that perspective that shows up
224 • ANATOMY OF AN EPIDEMIC
in efficacy trials of Ritalin and other ADHD drugs. Teachers and other observers fill out rating instruments that view a reduction in the child's movements and engagement with others as positive, and when the results are tabulated, 70 to 90 percent of the children are reported to be "good responders" to ADHD medications. These drugs, NIMH investigators wrote in 1995, are highly effective in "dramatically reducing a range of core ADHD symptoms such as task-irrelevant activity (e.g., finger tapping, fidgetiness, fine motor movement, off-task [behavior] during direct observation) and classroom disturbance."21 ADHD experts at Massachusetts General Hospital summed up the scientific literature in a similar way: "The extant literature clearly documents that stimulants diminish behaviors prototypical of ADHD, including motoric overactivity, impulsivity, and inattentiveness."22
However, none of this tells of drug treatment that benefits the child. Stimulants work for the teacher, but do they help the child?
Here, right from the start, researchers ran into a wall. "Above all else," wrote Esther Sleator, a physician at the University of Illinois who asked fifty-two children what they thought of Ritalin,
"we found a pervasive dislike among hyperactive children for taking stimulants. " fn 23
Children on Ritalin, University of Texas psychologist Deborah Jacobvitz reported in 1990, rated themselves as "less happy and [less] pleased with themselves and more dysphoric." When it came to helping a child make friends and sustain friendships, stimulants produced "few significant positive effects and a high incidence of negative effects," Jacobvitz said. fn 24
Other researchers detailed how Ritalin harmed a child's self-esteem, as the children felt they must be "bad" or "dumb" if they had to take such a pill. "The child comes to believe not in the soundness of his own brain and body, not in his own growing ability to learn and to control his behavior, but in 'my magic pills that make me into a good boy,' " said University of Minnesota psychologist Alan Sroufe.25
All of this told of harm done, of a drug that made a child depressed, lonely, and filled with a sense of inadequacy, and when researchers looked at whether Ritalin at least helped hyperactive children fare well academically, to get good grades and thus succeed as students, they found that it wasn't so. Being able to focus intently
THE EPIDEMIC SPREADS TO CHILDREN • 225
on a math test, it turned out, didn't translate into long-term academic achievement. This drug, Sroufe explained in 1973, enhances performance on "repetitive, routinized tasks that require sustained attention," but "reasoning, problem solving and learning do not seem to be [positively] affected."26
Five years later, Herbert Rie was much more negative. He reported that Ritalin did not produce any benefit on the students' "vocabulary, reading, spelling, or math," and hindered their ability to solve problems. "The reactions of the children strongly suggest a reduction in commitment of the sort that would seem critical for learning." fn 27
That same year, Russell Barkley at the Medical College of Wisconsin reviewed the relevant scientific literature and concluded "the major effect of stimulants appears to be an improvement in classroom manageability rather than academic performance." fn 28
Next it was James Swanson's turn to weigh in. The fact that the drugs often left children "isolated, withdrawn and overfocused" could "impair rather than improve learning," he said. fn 29
Carol Whalen, a psychologist from the University of California at Irvine, noted in 1997 that "especially worrisome has been the suggestion that the unsalutary effects [of Ritalin] occur in the realm of complex, high-order cognitive functions such as flexible problem-solving or divergent thinking." fn 30
Finally, in 2002, Canadian investigators conducted a meta-analysis of the literature, reviewing fourteen studies involving 1,379 youths that had lasted at least three months, and they determined that there was "little evidence for improved academic performance." fn 31
There was one other disappointment with Ritalin. When researchers looked at whether stimulants improved a child's behavior over the long term, they couldn't find any benefit. When a child stopped taking Ritalin, ADHD behaviors regularly flared up, the "excitability, impulsivity, or talkativeness" worse than ever. "It is often disheartening to observe how rapidly behavior deteriorates when medication is discontinued," Whalen confessed.32 Nor was there evidence that staying on a stimulant led to a sustained im-provement in behavior. "Teachers and parents should not expect long-term improvement in academic achievement or reduced antisocial behavior," Swanson wrote in 1993.33 The 1994 edition of the APA's Textbook of Psychiatry admitted to the same bottom-line
•
226 • ANATOMY OF AN EPIDEMIC
conclusion: "Stimulants do not produce lasting improvements in aggressivity, conduct disorder, criminality, education achievement, job functioning, marital relationships, or long-term adjustment."34 Thirty years of research had failed to provide any good-quality evidence that stimulants helped "hyperactive" children thrive, and in the early 1990s, a team of prominent ADHD experts picked to lead a long-term NIMH study, known as the Multisite Multimodal Treatment Study of Children with ADHD, acknowledged that this was so. "The long-term efficacy of stimulant medication has not been demonstrated for any domain of child functioning," they wrote.35
Stimulants Flunk Out
The NIMH touted its ADHD study as "the first major clinical trial" the institute had ever conducted of "a childhood mental disorder." However, it was a rather flawed intellectual exercise right from the start. Although the investigators, led by Peter Jensen, associate di-rector of child and adolescent research at the NIMH, acknowledged during the planning stages that there was no evidence in the scientific literature that stimulants improved long-term outcomes, they did not include a placebo control in the study, reasoning that it would have been "unethical" to withhold "treatment of known efficacy" for an extended period. The study basically compared drug treatment to behavioral therapy, but in that latter group, 20 percent were on a stimulant at the start of the trial, and there never was a time during the fourteen months that all of the children in that group were off such medication.36
Despite this obvious design flaw, the NIMH-funded investigators declared victory for the stimulants at the end of fourteen months. "Carefully crafted medication management" had proven to be "superior" to behavioral treatment in terms of reducing core ADHD symptoms. There was also a hint that the medicated children had fared better on reading tests (although not in other academic subjects), and as a result, psychiatry now had a long-term study that documented the continuing benefits of stimulants. "Since ADHD is
THE EPIDEMIC SPREADS TO CHILDREN • 227
now regarded by most experts as a chronic disorder, ongoing treatment often seems necessary," the researchers concluded.37
After that initial fourteen-month period of treatment, the investigators followed up periodically with the students, assessing how they were doing and whether they were taking an ADHD medication. This was now a naturalistic study much like the one that Martin Harrow had conducted of schizophrenia outcomes, and readers of this book, having become familiar with the scientific literature, can easily guess what is coming next. At the end of three years, Jensen and the others discovered that "medication use was a significant marker not of beneficial outcome, but of deterioration. That is, participants using medication in the 24-to-36 month period actually showed increased symptomatology during that interval relative to those not taking medication."38
In other words, those on medications saw their core ADHD symptoms—the impulsiveness, the inattentiveness, the hyperactivity—worsen, at least in comparison to those not on drugs. In addition, those on meds had higher "delinquency scores" at the end of three years, which meant they were more likely to get into trouble in school and with the police.39 They were also now shorter and weighed less than their off-med counterparts, evidence that the drugs suppressed growth. These results told of a drug therapy causing long-term harm, and when the NIMH-funded investigators reported on six-year outcomes, the findings remained the same. Medication use was "associated with worse hyperactivity-impulsivity and oppositional defiant disorder symptoms" and with greater "overall functional impairment."4°
Controversy has long raged over whether ADHD is a "real" disease, but this study showed that when it comes to using stimulants to treat it, the controversy is moot. Even if ADHD is real, stimulants aren't going to provide long-term help. "We had thought that children medicated longer would have better outcomes. That didn't happen to be the case," said William Pelham from the State University of New York at Buffalo, who was one of the principal investigators. "There were no beneficial effects, none. In the short term, [medica-tion] will help the child behave better, in the long run it won't. And that information should be made very clear to parents." fn 41
228 • ANATOMY OF AN EPIDEMIC
Tallying Up the Harm
With any medication, there is a benefit-risk assessment to be made, and the expectation is that the benefit will outweigh the risks. But in this case, the NIMH found that over the long term there was nothing to be entered on the benefit side of the ledger. That leaves only risks to be tallied up, and so now we need to look at all the ways that stimulants can harm children.
Ritalin and the other ADHD medications cause a long list of physical, emotional, and psychiatric adverse effects. The physical problems include drowsiness, appetite loss, lethargy, insomnia, headaches, abdominal pain, motor abnormalities, facial and vocal tics, jaw clenching, skin problems, liver disorders, weight loss, growth suppression, hypertension, and sudden cardiac death. The emotional difficulties include depression, apathy, a general dullness, mood swings, crying jags, irritability, anxiety, and a sense of hostility toward the world. The psychiatric problems include obsessive-compulsive symptoms, mania, paranoia, psychotic episodes, and hallucinations. Methylphenidate also reduces blood flow and glucose metabolism in the brain, changes that usually are associated with "neuropathologic states." fn 42 p 228
Animal studies of stimulants are also cause for alarm. Repeated exposure to amphetamines, scientists at the Yale School of Medicine reported in 1999, caused monkeys to exhibit "aberrant behaviors" that remained long after the drug exposure had stopped.43 Various rat studies suggested that lengthy exposure to methylphenidate might cause dopaminergic pathways to become permanently desensitized, and since dopamine is the brain's "reward system," medicating the child may produce an adult with a "reduced ability to experience pleasure. "44 Scientists at Texas Southwestern Medical Center in Dallas found that "preadolescent" rats exposed to methylphenidate for fifteen days turned into anxious, depressed "adult" rats. The adult rats moved around less, were less responsive to novel environments, and showed a "deficit in sexual behavior." They concluded that "administration of methylphenidate" while
THE EPIDEMIC SPREADS TO CHILDREN • 229
the brain is still developing "results in aberrant behavioral adaptations during adulthood.""
Such is the outcomes literature for Ritalin and other ADHD medications. The drugs alter a hyperactive child's behavior over the short term in a manner that teachers and some parents find helpful, but other than that, the medications diminish a child's life in many ways, and they may turn a child into an adult with a reduced physiological capacity to experience joy. And, as we'll see later in this chapter, there is one other heartbreaking risk with stimulants that remains to be explored.
Depressing Results
As recently as 1988, the year that Prozac came to market, only one in 250 children under nineteen years of age in the United States was taking an antidepressant.46 That was partly due to a cultural belief that youth were naturally moody and recovered quickly from de-pressive episodes, and partly because study after study had shown that tricyclics worked no better than placebo in this age group. "There is no escaping the fact that research studies certainly have not supported the efficacy of tricyclic antidepressants in treated depressed adolescents," a Journal of Child and Adolescent Psycho-pharmacology editorial acknowledged in 1992.47
However, when Prozac and other SSRIs were brought to market and touted as wonder drugs, the prescribing of antidepressants to children took off. The percentage of children so medicated tripled between 1988 and 1994, and by 2002 one in every forty children under nineteen years of age in the United States was taking an antidepressant." Presumably these drugs provide a short-term benefit to children and adolescents that the tricyclics fail to provide, but unfortunately, we can't review the scientific literature to see if that is true because, as is widely acknowledged today, the literature is hopelessly poisoned. The trials were biased by design; the results that were published in the scientific journals didn't square with the actual
230 • ANATOMY OF AN EPIDEMIC
data; adverse events were downplayed or omitted; and negative studies went unpublished or were spun into positive ones. "The story of research into selective serotonin reuptake inhibitor use in childhood depression is one of confusion, manipulation, and institutional failure," the Lancet wrote in a 2004 editorial. The fact that psychiatrists at leading medical schools had participated in this scientific fraud constituted an "abuse of the trust patients place in their physicians."49
However, a somewhat accurate picture of the merits of the drugs' efficacy in children has emerged through a roundabout process. During the course of SSRI-related lawsuits, expert witnesses for the plaintiffs—most notably David Healy in England and Peter Breggin in the United States—got a look at some of the trial data, and they observed that the drugs increased the suicide risk. They spoke out about what they had. found, and with an increasing number of an- guished parents telling of how their children had killed themselves after going on an SSRI, the FDA was forced to hold a hearing in 2004 on this risk. That, in turn, led to a stunning admission by the FDA's Thomas Laughren about the drugs' efficacy in children. Twelve of the fifteen pediatric antidepressant trials that had been conducted had failed. The FDA, in fact, had rejected the applications of six manufacturers seeking approval to sell their antidepressants to children. "These are sobering findings," Laughren confessed.s°
The FDA did approve Prozac for use in children, as two of the three positive studies reviewed by Laughren had come from trials of this drug. But, as many critics have pointed out, from a scientific perspective, there is no reason to think that Prozac is any better than the other SSRIs. The percentage of children who responded to Prozac in the two positive trials was similar to the drug response rate in the twelve failed trials; Eli Lilly simply had been better at using biased trial designs to make it appear that its drug worked. For example, in one of the two Prozac trials, all of the children were initially put on placebo for one week, and if they got better during that period, they were excluded from the study. This helped knock down the placebo response rate. Next, the children who were randomized onto Prozac were evaluated for a week, and only those "who adapted well" to the drug were then enrolled in the study.
THE EPIDEMIC SPREADS TO CHILDREN • 231
This helped increase the drug response rate. "Before the study even started," explained Jonathan Leo, editor in chief of the journal Ethical Human Psychology and Psychiatry, "there was a mechanism in place to maximize any difference between the drug and placebo groups—the placebo group was preselected for nonresponders, while the drug group was preselected for responders."51 Yet, even with this extremely biased trial design, the Prozac-treated children still fared no better than the placebo group on self-rating scales or ratings by their parents. In addition, the trial failed to show efficacy for fluoxetine on its "primary endpoint," and thus efficacy arose entirely from a secondary "improvement" scale filled out by the psychiatrists paid by Eli Lilly to run the trial.
Such was the record of efficacy produced by the SSRIs in pediatric trials for depression. Most trials failed to show any benefit, and Eli Lilly had to use a grossly biased trial design to make Prozac appear effective. In 2003, the Medicines and Healthcare Regulatory Agency (MHRA) in the United Kingdom essentially banned the use of SSRIs, except for fluoxetine, in patients under eighteen years old. English scientists then reviewed all the relevant data and reported in the Lancet that they supported "the conclusions reached by the MHRA."52 The truth, explained the Lancet editors in an accompanying editorial, was that these drugs "were both ineffective and harmful in children. "53 Australian scientists chimed in with a similar review in the British Medical Journal, their article enlivened by descriptions of the shenanigans that American psychiatrists had employed to make the SSRIs look beneficial in the first place. The authors of the positive studies, they said, had "exaggerated the benefits, downplayed the harms, or both." The Australians also reviewed Lilly's fluoxetine trials in children and determined that the "evidence for efficacy is not convincing." As such, they concluded that "recommending [any antidepressant] as a treatment option, let alone as first line treatment, would be inappropriate."54
In the absence of any efficacy benefit, we are now left with the unhappy task of tallying up the harm done by the prescribing of antidepressants to children and teenagers. We can start with the physical problems. SSRIs may cause insomnia, sexual dysfunction, headaches, gastrointestinal problems, dizziness, tremors, nervousness, muscle cramps, muscle weakness, seizures, and a severe inner agitation known as akathisia, which is associated with an increased risk of violence and suicide. The psychiatric problems they can trigger are even more problematic. … Other physicians have told of their SSRI-treated younger patients suffering panic attacks, anxiety, nervousness, and hallucinations. p 231
Timothy Wilens and Joseph Biederman at Massachusetts General Hospital conducted a chart review of eighty-two children treated with SSRIs, and determined that 22 percent of the children had suffered an adverse psychiatric event. Ten percent had become psychotic, and another 6 percent manic. "One of the most disturbing adverse outcomes is a worsening of emotional, cognitive or behavioral symptoms," they wrote. "These psychiatric adverse events to medication can be significantly impairing."55 North Carolina psychiatrist Thomas Gualtieri determined that 28 percent of the 128 children and adolescents he treated with SSRIs developed some type of "behavioral toxicity."56 Other physicians have told of their SSRI-treated younger patients suffering panic attacks, anxiety, nervousness, and hallucinations.
Those findings tell of children and adolescents being made sick by SSRIs, and that is over the short term. To appreciate the long-term risks, we can look at the problems that have cropped up in adults and in animal studies. If the children go off the medication, they can expect to suffer withdrawal symptoms, both physical and mental. Should they remain on the drugs for years, they are at high risk of becoming chronically depressed. They may also develop—as the
American Psychiatric Association warns in one of its textbooks—an "apathy syndrome," which "is characterized by a loss of motivation, increased passivity, and often feelings of lethargy and 'flatness.' " fn 57
There is also memory loss and cognitive decline to worry about, and, as we saw earlier, animal studies suggest that the drugs may cause serotonergic neurons to become swollen and misshapen.
Yet Another Illness Appears
First there was the ADHD explosion, and then came the news that
childhood depression was rampant, and not long after that, in the
late 1990s, juvenile bipolar disorder burst into public view. News-
THE EPIDEMIC SPREADS TO CHILDREN • 233
papers and magazines ran features on this phenomenon, and once more psychiatry explained its appearance with a story of scientific discovery. "It has long been thought in the psychiatric community that children could not be given a diagnosis of bipolar disorder until the mid-to-late teens, and that mania in children was extremely rare," wrote psychiatrist Demitri Papolos, in his bestselling book The Bipolar Child. "But scientists in the research vanguard are beginning to prove that the disorder can begin very early in life and that it is far more common than was previously supposed."" Yet the rise in the number of children and adolescents with this diagnosis was so astonishing—a fortyfold increase from 1995 to 2003—that Time, in an article titled "Young and Bipolar," wondered if something else might be going on.59 "New awareness of the disorder may not be enough to account for the explosion of juvenile bipolar cases," the magazine explained. "Some scientists fear that there may be something in the environment or in modern lifestyles that is driving into a bipolar state children and teens who might otherwise escape the condition."60
That speculation made perfect sense. How could a severe mental illness have gone unrecognized for so long, with doctors only now noticing that thousands of kids were going wildly manic? But if there were something new in the environment stirring this behavior, as Time suggested to its readers, there would be a logical explanation for the epidemic. Infectious agents stir epidemics, and thus, as we trace the rise of juvenile bipolar disorder, this is what we'll want to discover: Can we identify "outside agents" that are causing this modern-day plague?
As we learned earlier, manic-depressive illness was a rare condition prior to the psychopharmacology era, affecting perhaps one in ten thousand people. Although initial onset sometimes occurred in those fifteen to nineteen years old, it usually didn't appear until people were in their twenties. But more to the point, it virtually never appeared in children under thirteen years of age, and both pediatricians and medical researchers regularly emphasized this point.
In 1945, Charles Bradley said that pediatric mania was so rare that "it is best to avoid the diagnosis of manic-depressive psychosis in children."61 An Ohio physician, Louis Lurie, reviewed the
234 • ANATOMY OF AN EPIDEMIC
literature in 1950 and found that "observers have concluded that mania does not occur in children."62 Two years later, Barton Hall reviewed the case histories of 2,200 psychiatric patients five to sixteen years old, and found only two instances of manic-depressive ill-ness. In both instances, the patients were over thirteen years of age. "These facts endorse the general belief that manic-depressive states are illnesses of the maturing or matured personality," Hall said.63 In 1960, Washington University psychiatrist James Anthony scoured the medical literature for case reports of manic-depressive illness in children and could find only three. "Occurrence of manic depression in early childhood as a clinical phenomenon has yet to be demonstrated," he wrote."
But then, slowly but surely, such case reports began to appear. In the late 1960s and early 1970s, psychiatrists began prescribing Ritalin to hyperactive children, and suddenly, in 1976, Washington University's Warren Weinberg, a pediatric neurologist, was writing in the American Journal of Diseases of Childhood that it was time for the field to realize that children could go manic. "Acceptance of the concept that mania occurs in children is important in order that affected children can be identified, the natural history defined, and appropriate treatment established and offered to these children," he wrote."
This was the moment in the medical literature that pediatric bipolar disorder was, in essence, "discovered." In his article, Weinberg reviewed the case histories of five children suffering from this previously unrecognized illness, but he rushed past the fact that at least three of the five children had been treated with a tricyclic or Ritalin prior to becoming manic. Two years later, doctors at Massachusetts General Hospital announced that they had identified nine children with manic-depressive illness, and they, too, skipped over the fact that seven of the nine had been previously treated with amphetamines, methylphenidate, or "other medications to affect behavior."66 Then, in 1982, Michael Strober and Gabrielle Carlson at the UCLA Neuropsychiatric Institute put a new twist into the juvenile bipolar story. Twelve of the sixty adolescents they had treated with antidepressants had turned "bipolar" over the course of three
THE EPIDEMIC SPREADS TO CHILDREN • 235
years, which—one might think—suggested that the drugs had caused the mania. Instead, Strober and Carlson reasoned that their study had shown that antidepressants could be used as a diagnostic tool. It wasn't that antidepressants were causing some children to go manic, but rather the drugs were unmasking bipolar illness, as only children with the disease would suffer this reaction to an antidepressant. "Our data imply that biologic differences between latent depressive subtypes are already present and detectable during the period of early adoleScence, and that pharmacologic challenge can serve as one reliable aid in delimiting specific affective syndromes in juveniles," they said.67
The "unmasking" of bipolar illness in children soon speeded up. The prescribing of Ritalin and antidepressants took off in the late 1980s and early 1990s, and as this occurred, the bipolar epidemic erupted. The number of hostile, aggressive, and out-of-control children admitted to psychiatric wards soared, and in 1995 Peter Lewinsohn from the Oregon Research Institute concluded that 1 percent of all American adolescents were now bipolar." Three years later, Carlson reported that 63 percent of the pediatric patients treated at her university hospital suffered from mania, the very symptom that doctors in the pre-psychopharmacologic era almost never saw in children. "Manic symptoms are the rule, rather than the exception," she noted.69 Indeed, Lewinsohn's epidemiological data was now already out of date. The number of children discharged from hospitals with a bipolar diagnosis rose fivefold between 1996 and 2004, such that this "ferocious mental illness" was now said to strike one in every fifty prepubertal children in America. "We don't have the exact numbers yet," University of Texas psychiatrist Robert Hirschfeld told Time in 2002, "except we know it's there, and it's underdiagnosed."7°
An epidemic had come of age, and history reveals that it rose in lockstep with the prescribing of stimulants and antidepressants to children.
236 • ANATOMY OF AN EPIDEMIC
Creating the Bipolar Child
Given that chronology, we should be able to find data that explains why stimulants and antidepressants would have that iatrogenic effect. There should be data showing that if you treat 5 million children and adolescents with these drugs, then 20 percent or so will deteriorate in ways that will lead to a bipolar diagnosis. There should be evidence of iatrogenic harm that adds up mathematically to an epidemic.
We'll start with Ritalin.
Even before the prescribing of Ritalin took hold, it was well known that amphetamines could stir psychotic and manic episodes. Indeed, amphetamines did this with such regularity that psychiatric researchers pointed to this effect as evidence supporting the dopamine hypothesis of schizophrenia. Amphetamines upped dopamine levels in the brain, suggesting that psychosis was caused by too much of this neurotransmitter. In 1974, David janowsky, a physician at the University of California at San Diego School of Medi-cine, tested this hypothesis by giving three dopamine-elevating agents—d-amphetamine, 1-amphetamine, and methylphenidate—to his schizophrenia patients. While all three drugs made them more psychotic, methylphenidate turned out to be tops in this regard, doubling the severity of their symptoms.71
Given this understanding of methylphenidate, psychiatry could expect that giving Ritalin to young children would cause many to suffer a manic or psychotic episode.
Although this risk isn't well quantified, Canadian psychiatrists reported in 1999 that nine of ninety-six ADHD children they treated with stimulants for an average of twenty-one months developed "psychotic symptoms." fn 72
In 2006, the FDA issued a report on this risk. From 2000 to 2005, the agency had received nearly one thousand reports of stimulant-induced psychosis and mania in children and adolescents, and given that these MedWatch reports are thought to represent only 1 percent of the actual number of adverse events, this suggests that 100,000 youths diagnosed with ADHD suffered psychotic and or manic episodes during that five-year period. The FDA determined that
THE EPIDEMIC SPREADS TO CHILDREN • 237
these episodes regularly occurred in "patients with no identifiable risk factors" for psychosis, meaning that they were clearly drug-induced, and that a "substantial portion" of the cases occurred in children ten years or less. "The predominance in young children of hallucinations, both visual and tactile, involving insects, snakes and worms is striking," the FDA wrote.73
Once this drug-induced psychosis occurs, the children are usually diagnosed with bipolar disorder. Moreover, this diagnostic progression, from medicated ADHD to bipolar illness, is well recognized by experts in the field. In a study of 195 bipolar children and adoles-cents, Demitri Papolos found that 65 percent "had hypomanic, manic and aggressive reactions to stimulant medications." In 2001, Melissa DelBello, at the University of Cincinnati Medical Center, reported that twenty-one of thirty-four adolescent patients hospitalized for mania had been on stimulants "prior to the onset of an affective episode." These drugs, she confessed, may "precipitate depression and/or mania in children who would not have otherwise developed bipolar disorder."
Yet there is an even bigger problem with stimulants. They cause children to cycle through arousal and dysphoric states on a daily basis. When a child takes the drug, dopamine levels in the synapse increase, and this produces an aroused state. The child may show increased energy, an intensified focus, and hyperalertness. The child may become anxious, irritable, aggressive, hostile, and unable to sleep. More extreme arousal symptoms include obsessive-compulsive and hypomanic behaviors. But when the drug exits the brain, dopamine levels in the synapse sharply drop, and this may lead to such dysphoric symptoms as fatigue, lethargy, apathy, social withdrawal, and depression. Parents regularly talk of this daily "crash." But—and this is the key—such arousal and dysphoric symptoms are the very symptoms that the National Institute of Mental Health identifies as characteristic of a bipolar child. Symptoms of mania in children, the NIMH says, include increased energy, intensified goal-directed activity, insomnia, irritability, agitation, and destructive outbursts. Symptoms of depression in children include loss of energy, social isolation, a loss of interest in activities (apathy), and a sad mood.
238 • ANATOMY OF AN EPIDEMIC
The ADHD to Bipolar Pathway
Stimulant-drug Induced effects Bipolar Diagnotic Symptoms
Arousal Dysphoric Arousal Dysphoric
Increased energy Intensified focus Hyperalertness Euphoria Agitation, anxiety Insomnia Irritability Hostility
Hypomania Mania
Psychosis Somnolence Fatigue, lethargy
Social withdrawal, isolation
Decreased spontaneity Reduced curiosity Constriction of affect Depression
Emotional lability Increased energy
Intensified goal-
directed activity
Decreased need for
sleep
Severe mood change Irritability
Agitation
Destructive outbursts Increased talking Distractibility Hypomania
Mania Sad mood Loss of energy
Loss of interest in activities
Social isolation
Poor comnnuni- cation
Feelings of worth- lessness
Unexplained crying
Stimulants used to treat ADHD induce both arousal and dysphoric symptoms. These drug-induced symptoms overlap to a remarkable degree the symptoms said to be characteristic of juvenile bipolar disorder.
In short, every child on a stimulant turns a bit bipolar, and the risk that a child diagnosed with ADHD will move on to a bipolar diagnosis after being treated with a stimulant has even been quantified. Joseph Biederman and his colleagues at Massachusetts General Hospital reported in 1996 that 15 of 140 children (11 percent) diagnosed with ADHD developed bipolar symptoms—which were not present at initial diagnosis—within four years. fn 76 This gives us our first mathematical equation for solving the juvenile bipolar epidemic: If a society prescribes stimulants to 3.5 million children and adolescents, as is the case in the United States today, it should expect that this practice will create 400,000 bipolar youth. p 238
As Time noted, most children with bipolar illness are diagnosed with a different psychiatric disorder first, with "ADHD the likeliest first
call.
Now let's look at the SSRIs.
It is well established that antidepressants can induce manic episodes in adults, and naturally they have this effect on children, too. As early as 1992, when the prescribing of SSRIs to children was just getting started, University of Pittsburgh researchers reported
THE EPIDEMIC SPREADS TO CHILDREN • 239
that 23 percent of boys eight to nineteen years old treated with Prozac developed mania or maniclike symptoms, and another 19 percent developed "drug-induced" hostility.77 In Eli Lilly's first study of Prozac for pediatric depression, 6 percent of the children treated with the drug suffered a manic episode; none in the placebo group did.78 Luvox, meanwhile, was reported to cause a 4 percent rate of mania in children under 18.79 In 2004, Yale University researchers assessed this risk of antidepressant-induced mania in young and old, and they found that it is highest in those under thirteen years of age.8°
The incidence rates cited above are from short-term trials; the risk rises when children and teenagers stay on antidepressants for extended periods.
In 1995, Harvard psychiatrists determined that 25 percent of children and adolescents diagnosed with depression convert to bipolar illness within two to four years. "Antidepressant treatment may well induce switching into mania, rapid cycling or affective instability in the young, as it almost certainly does in adults," they explained." Washington University's Barbara Geller extended the follow-up period to ten years, and in her study, nearly half of prepubertal children treated for depression ended up bipolar. fn 82 These findings give us our second mathematical equation for solving the bipolar epidemic: If 2 million children and adolescents are treated with SSRIs for depression, this practice will create 500,000 to 1 million bipolar youth. We now have numbers that tell of an iatrogenic epidemic: 400,000 bipolar children arriving via the ADHD doorway, and at least another half million through the antidepressant doorway. There is also a way that we can double-check that conclusion: When investigators survey juvenile bipolar patients, do they find that most traveled down one of those two iatrogenic paths? p 239
Here are the results. In a 2003 study of seventy-nine juvenile bipolar patients, University of Louisville psychiatrist Rif ElMallakh determined that forty-nine (62 percent) had been treated with a stimulant or an antidepressant prior to their becoming manic.83 That same year, Papolos reported that 83 percent of the 195 bipolar children he studied had been diagnosed with some other psychiatric illness first, and that two-thirds had been exposed
59
xzxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
xzxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
244 • ANATOMY OF AN EPIDEMIC
postpubertal onset bipolar to recover," he said, and it was "expected that children will be poor responders to treatment when they become adults."93 DelBello followed a group of adolescents hospitalized for a first bipolar episode and concluded that only 41 percent functionally recovered within a year." This impairment, Birmaher determined, then worsens after the first year. "Functional impairment in bipolar appears to increase during adolescence regardless of age of onset."95
Youth diagnosed with bipolar illness are typically put on drug cocktails that include an atypical antipsychotic and a mood stabilizer. This means that they now have multiple neurotransmitter pathways in their brains that are being mucked up, and naturally, this treatment does not lead them back to emotional and physical health. In 2002, DelBello reported that lithium, antidepressants, and mood stabilizers all failed to help bipolar youth fare better at the end of two years. Those who were treated with a neuroleptic, she added, "were significantly less likely to recover than those who did not receive a neuroleptic."96 Six years later, Hayes, Inc., a Pennsylvania consulting firm that conducts "unbiased" assessments of drugs for health-care providers, concluded that there was no good scientific evidence that the mood stabilizers and atypical antipsychotics prescribed for pediatric bipolar were either safe or effective. "Our findings indicate that at this time, anticonvulsants and atypical anti-psychotics cannot be recommended for children diagnosed with bipolar disorders," said Elisabeth Houtsmuller, senior analyst for Hayes.97 These reports attest to a lack of drug efficacy, but as Houtsmuller noted, the side effects from these "pharmacological treatments" are "alarming."
In particular, atypical antipsychotics may cause metabolic dysfunction, hormonal abnormalities, diabetes, obesity, emotional blunting, and tardive dyskinesia. Eventually, the drugs will induce cognitive decline, and the child who stays on the cocktails into adulthood can expect to die early as well. That is the long-term course of this iatrogenic illness: A child who may be hyperactive or depressed is treated with a drug that triggers a manic episode or some degree of emotional instability, and then the child is put on a drug cocktail that leads to a lifetime of disability. p 244
The Disability Numbers
There are no good studies yet on the percentage of "early onset" bipolar patients who, when they reach adulthood, end up on the SSI and SSDI disability rolls. However, the astonishing jump in the number of "severely mentally ill" children receiving SSI speaks volumes about the havoc that is being wreaked. There were 16,200 psychiatrically disabled youth under eighteen years old on the SSI rolls in 1987, and they comprised less than 6 percent of the total number of disabled children. Twenty years later, there were 561,569 disabled mentally ill children on the SSI rolls, and they comprised 50 percent of the total. This epidemic is even hitting preschool children. The prescribing of psychotropic drugs to two-year-olds and three-year-olds began to become more commonplace about a decade ago, and sure enough, the number of severely mentally ill children under six years of age receiving SSI has tripled since then, rising from 22,453 in 2000 to 65,928 in 2007.98
Moreover, the SSI numbers only begin to hint at the scope of the harm being done. Everywhere there is evidence of a worsening of the mental health of children and teenagers. From 1995 to 1999, psychiatric-related emergency room visits by children increased 59 percent.99 The deteriorating mental health of. the nation's children, declared U.S. surgeon general David Satcher in 2001, constituted "a health crisis."1°° Next, colleges were suddenly wondering why so many of their students were suffering manic episodes or behaving in disturbed ways; a 2007 survey discovered that one in six college students had deliberately "cut or burned self" in the prior year.101 All
246 • ANATOMY OF AN EPIDEMIC
The Epidemic Hits America's Children
551 Recipients Under 18 Years Old Disabled by Mental Illness, 1987-2007
Prior to 1992, the government's 551 reports did not break down children recipients into subgroups by age. Source: Social Security Administration reports, 1987-2007.
of this led the U.S. Government Accountability Office to investigate what was going on, and it reported in 2008 that one in every fifteen young adults, eighteen to twenty-six years old, is now "seriously mentally ill." There are 680,000 in that age group with bipolar dis-order and another 800,000 ill with major depression, and, the GAO noted, this was in fact an undercount of the problem, as it didn't include young adults who were homeless, incarcerated, or institutionalized. All of these youth are "functionally impaired" to some degree, the GAO said.102
That is where we stand as a nation today. Twenty years ago, our society began regularly prescribing psychiatric drugs to children and adolescents, and now one out of every fifteen Americans enters adulthood with a "serious mental illness." That is proof of the most tragic sort that our drug-based paradigm of care is doing a great deal more harm than good. The medicating of children and youth became commonplace only a short time ago, and already it has put millions onto a path of lifelong illness.
I 2
Suffer the Children
"You wonder all the time:
Are you helping or harming your child?"
—JASMINE'S MOM (2009)
There are an endless number of stories of medicated children that can be told, and as I worked on this book, each visit to a place where such children can be found—to a family's home or to a foster care provider or to a psychiatric hospital—offered at least a brief glimpse of this new society we have created in the past thirty years. There are, of course, many parents who will tell of how their children have been helped by psychiatric drugs, and given the spectrum of outcomes that occur with this paradigm of care, that is undoubtedly true (at least over the short term). But this book is about the epidemic of disabling mental illness that has erupted in our country, and so the stories that follow tell, at best, of ambivalent long-term outcomes, and of how diagnosis and treatment during childhood may lead to a life of disability.
1987
1992
1997
2002
2007
Total
6-12 Years Old
13-17
EM Years Old
0-5
Years Old
600,000 500,000 400,000 300,000 200,000 100,000
250 • ANATOMY OF AN EPIDEMIC
Toward the end of her junior year, Jasmine read on the Internet that Zyprexa could cause
Zyprexa could cause weight gain, hypoglycemia, and diabetes.
She suffered from the first two of those problems, but when she asked her psychiatrist about Zyprexa's side effects, he dismissed her concerns. Enraged, Jasmine "fired" him, and in June of 2005, she took herself off both medications, stopping them rather abruptly. Ten days after she took a final dose of Zyprexa, she was on an excursion with her mother when she suddenly turned ashen, sweat beading up on her lip. "This is really bad," she muttered. "Mom, fight for me."
Jasmine has been more or less lost to the world ever since. By the time they arrived at the hospital, Jasmine was screaming and tearing at her hair. She was deep into a withdrawal psychosis, and doctors began giving her one powerful drug after another, trying to get it to abate. "They put her on eleven medications in thirteen days, which essentially fried her brain," her mother says. Jasmine began cycling in and out of hospitals, and every time she was discharged home, it ended badly. At times, she was so psychotic that she would call the police to tell them that she was being kidnapped or that men were building bombs in her front yard. On several occasions, she "escaped" from her house and ran screaming into the streets. Another time she kicked and punched her mom; afterward, she ripped a soda can open and slashed at her wrist. "This is the most psychotic person we have ever seen in the history of this ER," hospital staff told Jasmine's mom after one such episode.
In late 2006, a doctor put Jasmine on a single antipsychotic, Clozaril, and that led to a brief respite. Although Jasmine rarely spoke, she calmed down and entered a school for disabled children. At night, her mother read to her for hours, seeking to nurture the spark of sanity she now saw in Jasmine. "I also noticed that if I sang to her, like to an Alzheimer's patient, she would sing back, communicating through singing." But in early 2007, Jasmine suffered another severe bout of psychosis, which ended with her screaming in the middle of a busy road. "There is no hope for her," doctors said, and soon Jasmine was placed at the residential facility, where today she passes her days, shying away from contact with other people and, except for an occasional word now and then, mute.
SUFFER THE CHILDREN • 251
"The doctors tell me she was always going to be schizophrenic," her mother says. "But no doctor ever asked about this history, about what she was like before she was put on drugs. And you know what's so hard to accept? We came in for help that summer when she was eleven years old for a minor problem that had nothing to do with psychiatry. In my mind, I can hear her laughing, like she was back then. But her life has been stolen away. We've lost her, even though her body remains. I see every minute what I've lost."
Ambivalent in Syracuse
Senior year was a good time for Andrew Stevens. Diagnosed with ADHD and put on medication when he was in first grade, he'd had up-and-down times in school until his senior year. But then he took a course in auto mechanics, and bingo, he excelled in a way he never had before. "I'm in the zone," he explains. "I enjoy it. It doesn't feel like school."
On this afternoon, Andrew, who is slight of build and perhaps five feet, six inches tall, looks very much like the skateboarder he is: short-cropped hair, black earring, and wearing a T-shirt, shorts, and tennis shoes splashed with a kaleidoscope of colors. I had met his mother, Ellen, a year earlier, at a conference in Albany, New York, and she had expressed a sentiment that, I thought, neatly summarized the moral aspect of our society's medicating of youth: "Andrew has been a guinea pig for the medical field," she'd said.
Very early on, she and her husband had realized that Andrew was different from their other two children. He had speech problems; his behavior seemed eccentric; he had "rage issues." In first grade, he was so wound up he regularly needed to go into the hallway and bounce on a mini-trampoline in order to refocus. "I remember crying when he was diagnosed with ADHD, and it wasn't because my kid was labeled," his mother says. "It was, 'Thank God, we know something real is going on with him and they know how to help him. It's not our imagination.' "
Although she and her husband worried about putting Andrew on
252 • ANATOMY OF AN EPIDEMIC
Ritalin, doctors and school authorities led her to believe that she would be "remiss as a parent" if she didn't give him the medication. And at first, "it was like a miracle," she says. Andrew's fears abated, he learned to tie his shoes, and his teachers praised his improved behavior. But after a few months, the drug no longer seemed to work so well, and whenever its effects wore off, there would'be this "rebound effect." Andrew would "behave like a wild man, out of control." A doctor increased his dosage, only then it seemed that Andrew was like a "zombie," his sense of humor reemerging only when the drug's effects wore off. Next, Andrew needed to take clonidine in order to fall asleep at night. The drug treatment didn't really seem to be helping, and so Ritalin gave way to other stimulants, including Adderall, Concerta, and dextroamphetamine. "It was always more drugs," his mother says.
Meanwhile, Andrew's success in the classroom fluctuated according to the talents of his teacher. In fourth and fifth grade, he had teachers who knew how to work with him, and he did fairly well. But his sixth-grade teacher was impatient with him, and Andrew's self-esteem took such a nosedive that his mother homeschooled him the following year. Andrew's anxieties worsened during this period, and often he would be "hyperfocused," worrying all the time that his mother might die. He also was notably smaller than his peers, and his parents thought the drugs were probably curbing his growth. "That has been the most frustrating part. I never know what is my son and what is the drug," his mother says.
“Today, her ambivalence about the medications is such that she wishes she could turn back the clock and try a different tack. "My Andrew is not a circle or a square, he is not even a triangle," she explains. "He is a rhombus trapezoid, and he will never fit into those other molds. And I do think that if we had never put him on medicine, he would have learned many more coping mechanisms, because he would have had to. And we should be able to help kids like Andrew without making them feel so different, without suppressing their appetite, and without worrying about the long-term effects of the drugs—all the things I am sitting here worrying about."” (quoting Andew Stevens mother, p 251
When Andrew was younger, he was allowed "medication breaks" now and then, and when I ask him what that was like, he
SUFFER THE CHILDREN • 253
recalls how nice it was to fall asleep without having to take clonidine. Being off meds, he says, "feels less constricted, more free." Still, he tells me, he is about to graduate from high school, and he has ended up at a good place. He has a girlfriend, he enjoys skateboarding and playing the guitar, and thanks to the auto mechanics class, he now has career plans, as he intends to one day open his own garage. "It's hard to think back to a time when it could have been different," he says, shrugging, thinking about his life on medications. "I don't think there was a right or wrong choice—this is just how it's been."
“If You're a Ward of the State, You Must Be Bipolar: The medicating of foster children in the United States took off in the late 1990s, and so I thought, in order to gain a perspective on this phenomenon, I would visit with Theresa Gately. She and her husband, Bill, took ninety-six foster children into their Boston home from 1996 to 2000, and thus she personally witnessed this change in how our society treats foster kids. The first children that Social Services sent them weren't medicated, but by the end, "it felt like all of them were on psych drugs," she says.” p 253
Over the course of several hours, we sat on her front porch, which looks out over a busy street in a fairly rough part of Boston, and nearly everyone who walked by waved and affectionately shouted hello, no matter what their ethnicity. Theresa Gately is a thin woman with straw blond hair, and she has her own history as a foster child. Born in 1964, she was sexually abused by her stepfather, and she turned so defiant as a teenager that she landed in a Maryland psychiatric hospital. There she was put on Thorazine and other neuroleptics, and, she said, it wasn't until she started "tonguing" the drugs—pretending to take them while nurses were watching and then spitting them out—that her head started to clear. However, she isn't "anti-medication" at all, and during a difficult time a few years back, she found an antidepressant and a mood stabilizer to be extremely helpful, and she remains on those drugs.
254 • ANATOMY OF AN EPIDEMIC
As a foster mother, Gately was required to follow "medical advice" and give psychiatric medications to the children who arrived on them. Most of the children were on cocktails, and it seemed to her that the drugs were primarily being used to make the children quieter and easier to manage. "One young girl, Liz, was so heavily medicated that she couldn't think at all," she recalls. "You would ask her if she wanted a pork chop and she wouldn't answer." Another was "almost mute when she came to me. The last thing you need to do is give somebody who already doesn't talk more drugs." Theresa ran through the histories of several more of her foster children, concluding that "maybe nine to eleven [of the ninety-six children] needed to have the drugs and were being helped."
She has kept track of a number of the ninety-six children, and as could be expected, many have struggled mightily as adults. Had she, I wondered, noticed a difference in the fate of those who stayed on the drug cocktails, versus those who stopped taking them?
"When I look back on the kids that stayed on the drugs and those who got off, it is the ones that are off that are the successes," she says. "Liz should never have been on the drugs. She got off the drugs and is doing great. She is a full-time student in nursing school and almost ready to graduate, and is about to get married. The thing is, if you get off the drugs, you start building these coping mechanisms. You learn internal controls. You start building these strengths. Most of these kids have had very bad stuff happen to them. But they are able to rise above their past once they are off the medications, and then they can move on. The kids who were drugged and continue to be drugged never have that opportunity to build coping skills. And because they never had that opportunity as a teenager, as an adult they don't know what to do with themselves."
Hers isn't a scientific study. But her experience does offer a peek into the toll that the medicating of foster kids is taking. Most of those who stayed on the drugs, she says, ended up "filing for disability."
Like Theresa Gately, Sam Clayborn, who is a social worker in New
Rochelle, New York, can tell from personal experience what it is
like to have been a foster kid in the United States. When he was
SUFFER THE CHILDREN • 255
born in Harlem in 1965, his mother was unable to take care of him, and by age six he was living in a residential group home. We met in his apartment in Croton-on-Hudson, and very quickly he put things into a historical context. "They weren't so hot on psychiatric diagnoses back then," he explains. "They were more into beating your ass, restraining you, and just throwing you into an empty fucking room. I'm glad I grew up when it was like that rather than what it is like today, because if I grew up now, I'd be fucking drugged up. I'd be doped out and zonked out."
For the past two decades, he and his partner Eva Dech have worked as advocates for foster children and poor youth in Westchester County. She also had a tough childhood, which included a stint in a mental hospital where she was forcibly medicated, and they see a racial aspect to this medicating of foster children. Starting around 2000, rates of black youth diagnosed with bipolar disorder soared, and based on hospital discharges, they are now said to suffer from bipolar disorder at a greater rate than whites.' The diagnosis provides a rationale for medicating the kids, and that in turn puts yet one more burden on them, Clayborn believes.
"The Tuskegee syphilis experiments were nothing compared to this. That's mild shit compared to what they are doing to black kids today. The pharmaceutical companies and the government are fucking in cahoots, and they are doing a wicked dance with a lot of people's lives. They don't give a fuck about these kids. It's all about capitalism, and they will sacrifice all the niggers in the hood. We are damaging these kids for life, and the majority of these kids will never rebound. These kids will be destroyed and they are going to make the SSI rolls more overwhelmed."
One of the area youth that Clayborn has mentored is Jonathan Barrow, who had been splayed out on the living room floor during our conversation, half sleeping and half listening. Born in 1985 in Harlem to a mother on crack, Jonathan bounced around as a child, eventually ending up at his grandfather's home in White Plains. At age seven, he was diagnosed with ADHD and put on Ritalin. In junior high, he started becoming rebellious and got into a few fights, and that led to a diagnosis of bipolar disorder and a prescription for Depakote and Risperdal. Up until that time, Jonathan had been an
256 • ANATOMY OF AN EPIDEMIC
active adolescent who spent most of his free time on the basketball court, but now he began spending most of his time "in his room isolated," Clayborn says. He went onto the SSI disability rolls before he turned eighteen, apparently "severely impaired" by this bipolar illness, and he remains on SSI today. "I'm doped up," Jonathan explains, still somewhat heavy-lidded from his afternoon nap. "I don't like it. It makes me sleepy and feel like a dope fiend."
At this, Clayborn rose from his chair, more agitated than ever. "This is happening to a lot of the brothers today, and once they are on the medication, it takes them away from themselves. They lose all the willpower to struggle, to change, to make something out of themselves and have success. They succumb to the chemical handcuffs of the motherfucking medications. It's medical bondage is what it is."
Not long after that interview, I attended a meeting of the Statewide Youth Advisory Council at Westborough State Hospital in Massachusetts. The council is composed of young adults who entered the mental health system before they were eighteen, and it provides advice to the Massachusetts Department of Mental Health on what it can do to help teenagers with psychiatric problems thrive as adults. In 2008, the coordinator of the council was Mathew McWade, who was first diagnosed when he was in the seventh grade, and it was he who made my visit possible.
At the meeting, I went around the table and asked everyone how they had gotten into the system. I thought I might hear stories of kids who were first put on a stimulant or an antidepressant and then moved on to a bipolar diagnosis, and while there was some of that, several men in this racially mixed group told of yet another societal route to psychiatric disability.
When Cal Jones" was sixteen years old, he had gotten into a violent argument that ended with his being treated in the emergency room at Children's Hospital in Boston. There he told ER staff that
* Cal Jones is a pseudonym. Hospital staff asked that I not reveal the names of the hospitalized patients.
SUFFER THE CHILDREN • 257
he "wanted to kill the other kid," a sentiment that earned him a trip to a psychiatric facility, where he was diagnosed with bipolar illness. "They didn't run any tests," he says. "They just asked me a bunch of questions and started me on a bunch of medicines." Since then, he has been hospitalized twenty-five times. He doesn't like antipsychotics, and so he regularly stops taking them when he is discharged, preferring to smoke marijuana instead, and inevitably that leads to trouble. "I get arrested and get sent back to the (psych) hos-pital, and I'm like okay, it's just a business. The more patients they have, the more the doctors make. But I hate it. I can't stand it. I feel like a slave in a Nazi camp."
At least three others at the meeting told similar stories. One young man said that shortly after he graduated from high school in 2002, he got upset over a family matter and smashed the windows of his car. "I was having a bad time. They wanted to label me as mentally ill. I don't know if I am." Another explained that six months earlier, after he had committed a minor criminal act, a judge had given him the choice of going to prison or to Westborough State Hospital. "It's safer in here than in prison," he says, explaining his choice. A third member of the council said that he had been diagnosed with bipolar illness at age thirteen after "I killed somebody."
Their stories bore witness to another pathway into the mental health system for poor youth. Delinquency and crime can get them diagnosed, medicated, and routed into a mental institution. While many of the young men on the council were on heavy-duty cock-tails, moving about and speaking in a sluggish manner, the one who had told of having killed somebody was now living in the community and not taking any medications. "If the state really wants to help us, it should put money into a jobs program," he says.
Back to Syracuse
As a last stop, I returned to visit the two Syracuse families—Jason
and Kelley Smith and Sean and Gwen Oates—that I had met in the
spring of 2008. Families, friends, therapists, and doctors had given
"It was not surprising that medical students accepted
the dogma of biomedical reductionism in psychiatry
uncritically; they had no time to read and analyze the
original literature. What took me a while to understand,
as I moved through my residency, was that psychiatrists
rarely do the critical reading either."
-COLIN ROSS, CLINICAL ASSOCIATE PROFESSOR OF
PSYCHIATRY AT SOUTHWEST MEDICAL CENTER IN
DALLAS, TEXAS (1995)'
264 • ANATOMY OF AN EPIDEMIC
the rest of medicine, and once NIMH researchers and others advanced the chemical imbalance theory of mental disorders, it seemed that these pills might indeed be antidotes to physical diseases. "American psychiatry," exclaimed former NIMH director Gerald Klerman, "accepted psychopharmacology as its domain."2 But two decades later, those heady days were long gone, and psychiatry was mired in a deep crisis, beleaguered on so many fronts that it worried about its survival. There was a sense, said American Psy-chiatric Association (APA) director Melvin Sabshin in 1980, that the "profession is under severe siege and is cut off from allies."3
The first problem that had arisen for psychiatry was an intellectual challenge to its legitimacy, an attack launched in 1961 by Thomas Szasz, a psychiatrist at the State University of New York in Syracuse. In his book The Myth of Mental Illness, he argued that psychiatric disorders weren't medical in kind, but rather labels applied to people who struggled with "problems in living" or simply behaved in socially deviant ways. Psychiatrists, he said, had more in common with ministers and police than they did with physicians. Szasz's criticism rattled the field, since even mainstream publications like the Atlantic and Science found his argument to be both cogent and important, the latter concluding that his treatise was "enormously courageous and highly informative . . . bold and often brilliant." fn 4, p 264
As Szasz later told the New York Times, "In smoke-filled rooms, time and time again, I've heard the view that Szasz has killed psychiatry. I hope so."5
His book helped launch an "antipsychiatry" movement, and other academics in the United States and Europe—Michel Foucault, R. D. Laing, David Cooper, and Erving Goffman, just to name a few—joined the fray. All questioned the "medical model" of mental disorders and suggested that madness could be a "sane" reaction to an oppressive society. Mental hospitals might better be described as facilities for social control, rather than for healing, a viewpoint crystallized and popularized in One Flew Over the Cuckoo's Nest, which swept the Oscars for 1975. Nurse Ratched was the malevolent cop in that movie, which ended with Randle McMurphy (played by Jack Nicholson) being lobotomized for failing to stay in line.
THE RISE OF AN IDEOLOGY • 265
The second problem that psychiatry faced was a growing competition for patients. In the 1960s and 1970s, a therapy industry blossomed in the United States. Thousands of psychologists and counselors began offering services to the "neurotic" patients that psychiatry had laid claim to ever since Freud had brought his couch to America. By 1975, the nonphysician therapists outnumbered the shrinks in the United States, and with benzodiazepines falling out of favor, the neurotic patients who had been content to pop "happy pills" in the 1960s were embracing primal scream therapy, Esalen retreats, and any number of other "alternative" therapies said to help heal the wounded soul. Partly as a result of this competition, the median earnings of a U.S. psychiatrist in the late 1970s were only $70,600, and while this was a good wage at the time, it still put psychiatry near the bottom of the medical profession. "Non-psychiatric mental health professionals are laying claim to some, or even all, of psychiatry's task domains," wrote Tufts University psy-chiatrist David Adler. There was reason, he said, to worry about the "death of psychiatry."'
Internal divisions also ran deep. Although the field had turned toward biological psychiatry after the arrival of Thorazine, with most psychiatrists eager to speak well of the drugs, the Freudians who dominated many medical schools in the 1950s had never com-pletely climbed on that bandwagon. While they found some use for the drugs, they still conceived of most disorders as psychological in kind. As such, during the 1970s, there was a deep philosophical split between the Freudians and those who embraced a "medical model" of psychiatric disorders. In addition, there was a third faction in the field, composed of "social psychiatrists." This group thought that psychosis and emotional distress often arose from an individual's conflict with his or her environment. If that was so, altering that environment or creating a supportive new one—as Loren Mosher had done with his Soteria Project—would be a good way to help a person heal. Like the Freudians, the social psychiatrists did not see drugs as the centerpiece of care, but rather as agents that were sometimes helpful and sometimes not. With these three approaches in conflict, the field was suffering from an "identity crisis," Sabshin said.'
268 • ANATOMY OF AN EPIDEMIC
had "produced a nightmare of dependence and addiction."12 Anti-psychotics and the benzodiazepines were the two classes of drugs that had launched the psychopharmacology revolution, and with both now seen by the public in a negative light, sales of psychiatric drugs plunged in the 1970s, from 223 million drugstore prescriptions in 1973 to 153 million in 1980.13 In its article on psychiatry's "anxious years," the New York Times explained that a primary reason that medical school graduates were avoiding the field was because its treatments were perceived to be "low in efficacy."
This was a topic that psychiatry did not like to talk about or acknowledge. Yet, at the same time, everyone understood what gave psychiatrists a competitive advantage in the therapy marketplace. New Jersey psychiatrist Arthur Platt was at a professional meeting in the late 1970s when a keynote speaker laid it out for them: "He said, 'What is going to save us is that we're physicians,' " Platt recalls.14 They could write prescriptions and the psychologists and social workers couldn't, and that was an economic landscape that presented the field with an obvious solution. If the image of psychotropic drugs could be rehabilitated, psychiatry would thrive.
Putting on the White Coat
The process that led to the rehabilitation of psychiatric drugs in the public's mind got under way in the 1970s. Threatened by Szasz's criticism that psychiatrists did not really function as "doctors," the APA argued that psychiatrists needed to more explicitly embrace this role. "A vigorous effort to remedicalize psychiatry should be strongly supported," said the APA's Sabshin in 1977.15 Numerous articles appeared in the American Journal of Psychiatry and other journals explaining what this meant. "The medical model," wrote University of Kentucky psychiatrist Arnold Ludwig, is based on the "premise that the primary identity of the psychiatrist is as a physician."16 Mental disorders, said Paul Blaney, from the University of Texas, were to be seen as "organic diseases."17 The psychiatrist's focus should be on making the proper diagnosis, which arose from
THE RISE OF AN IDEOLOGY • 269
a cataloguing of the "symptoms and signs of illness," said Samuel Guze, from Washington University. It was only psychiatrists, he added, that had the "medical training necessary for the optimal application of the most effective treatments available today for psychiatric patients: psychoactive drugs and ECT [electroshock]."18
Theirs was a model of care straight out of internal medicine. The doctor in that setting took a patient's temperature, or tested blood glucose levels, or did some other diagnostic test, and then once the illness was identified, prescribed the appropriate drug. "Remedical-ization" of psychiatry meant that the Freudian couch was to be trotted off to the Dumpster, and once that happened, psychiatry could expect to see its public image restored. "The medical model is most strongly linked in the popular mind to scientific truth," explained Tufts University psychiatrist David Adler.19
In 1974, the APA picked Robert Spitzer from Columbia University to head up the task force that would, through a revision of the APA's Diagnostic and Statistical Manual, prompt psychiatrists to treat patients in this way. DSM-II, which had been published in 1967, reflected Freudian notions of "neurosis," and Spitzer and others argued that such diagnostic categories were notoriously "unreliable." He was joined by four other biologically oriented psychiatrists on the task force, including Samuel Guze at Washington University. DSM-III, Spitzer promised, would serve as "a defense of the medical model as applied to psychiatric problems."2° The manual, said APA president Jack Weinberg in 1977, would "clarify to anyone who may be in doubt that we regard psychiatry as a spe-cialty of medicine."21
Three years later, Spitzer and his colleagues published their handiwork. DSM-III identified 265 disorders, all of which were said to be distinct in kind. More than one hundred psychiatrists had contributed to the five-hundred-page tome, authorship that indicated it represented the collective wisdom of American psychiatry. To make a DSM-III diagnosis, a psychiatrist would determine if a patient had the requisite number of symptoms said to be characteristic of the disease. For instance, there were nine symptoms common to "major depressive episode," and if five were present, then a diagnosis of this illness could be made. The new manual, Spitzer boasted, had been
270 • ANATOMY OF AN EPIDEMIC
"field tested," and those trials had proven that clinicians in different facilities, when faced with the same patient, were likely to arrive at the same diagnosis, proof that diagnosis would no longer be as subjective as before. "These [reliability] results were so much better than we had expected" they would be, he said.22
Psychiatry now had its medical-model "bible," and the APA and others in the field rushed to extol it. DSM-III is an "amazing document . . . a brilliant tour de force," Sabshin said.23 "The development of DSM-III," said Gerald Klerman, "represents a fateful point in the history of the American psychiatric profession . . . [and] its use represents a reaffirmation on the part of American psychiatry to its medical identity and its commitment to scientific medicine."24 Thanks to DSM-III, wrote Columbia University psychiatrist Jerrold Maxmen, "the ascendance of scientific psychiatry became official . . . the old [psychoanalytical] psychiatry derives from theory, the new psychiatry from fact."25
But as critics at the time noted, it was difficult to understand why this manual should be regarded as a great scientific achievement. No scientific discoveries had led to this reconfiguring of psychiatric diagnoses. The biology of mental disorders remained unknown, and the authors of DSM-III even confessed that this was so. Most of the diagnoses, they said, "have not yet been fully validated by data about such important correlates as clinical course, outcome, family history, and treatment response."26 It was also evident that the boundary lines between disease and no disease had been arbitrarily drawn. Why did it require the presence of five of nine symptoms said to be characteristic of depression for a diagnosis of the illness to be made? Why not six such symptoms? Or four? DSM-III, wrote Theodore Blau, president of the American Psychological Associa-tion, was more of "a political position paper for the American Psychiatric Association than a scientifically-based classification system." fn 27 None of that mattered, however. With the publication of DSMIII, psychiatry had publicly donned a white coat. The Freudians had been vanquished, the concept of neurosis basically tossed into the trash bin, and everyone in the profession was now expected to embrace the medical model., p 270
“Biopsychiatry” “molecular psychiatry”
"It is time to state forcefully that the
THE RISE OF AN IDEOLOGY • 271
identity crisis is over," Sabshin said.28 Indeed, the American Journal of Psychiatry urged its members to "speak with a united voice, not only to secure support, but to buttress [psychiatry's] position against the numerous other mental health professionals seeking pa-tients and prestige."29 The medical model and DSM-III, observed University of Tennessee psychiatrist Ben Bursten in 1981, had been used to "rally the troops . . . to thwart the attackers [and] to rout the enemy within. "30
Indeed, it wasn't only the Freudians who had been vanquished. Loren Mosher and his band of social psychiatrists also had been roundly defeated and sent packing.
When Mosher started his Soteria Project in 1971, everyone understood that it threatened the "medical model" theory of psychiatric disorders. Newly diagnosed schizophrenia patients were being treated in an ordinary home, staffed by nonprofessionals, without drugs. Their outcomes were to be compared with patients treated with drugs in a hospital setting. If the Soteria patients fared better, what would that say about psychiatry and its therapies? From the minute that Mosher proposed it, the leaders of American psychiatry had tried to make sure it would fail. Although Mosher headed up the Center for Schizophrenia Studies at the NIMH, he'd still needed to obtain funding for Soteria from the grants committee that oversaw NIMH's extramural research program, which was composed of psychiatrists from leading medical schools, and that committee slashed his initial request of $700,000 for five years to $150,000 for two years. This ensured that the project would struggle with finances from the outset, and then, in the mid-1970s, when Mosher began reporting good results for his Soteria patients, the committee struck back. The study had "serious flaws" in its design, it said. Evidence that Soteria patients had superior outcomes was "not compelling."31 Mosher must be biased, the academic psychiatrists concluded, and they demanded that Mosher be removed as the primary investigator. "The message was clear," Mosher said, in an interview twenty-five years later. "If we were getting outcomes this good, then I must not be an honest scientist."32 Soon after that, the grants committee shut off funding for the experiment altogether, and Mosher was pushed from his job at the NIMH, even though the
272 • ANATOMY OF AN EPIDEMIC
committee had grudgingly concluded, in its final review of the project, that "this project has probably demonstrated that a flexible, community based, non-drug residential psychosocial program manned by non-professional staff can do as well as a more conventional community mental health program."
The NIMH never funded an experiment of this type again. Furthermore, Mosher's ouster provided everyone in the field with a clear message: Those who did not get behind the biomedical model would not have much of a future.
Psychiatry's Mad Men
Once DSM-III was published, the APA set out to market its "medical model" to the public. Although professional medical organizations have always sought to advance the economic interests of their members, this was the first time that a professional organization so thoroughly adopted the marketing practices familiar to any commercial trade association. In 1981, the APA established a "division of publications and marketing" to "deepen the medical identification of psychiatrists," and in very short order, the APA transformed itself into a very effective marketing machine.33 "It is the task of the APA to protect the earning power of psychiatrists," said APA vice president Paul Fink in 1986.34
As a first step, the APA established its own press in 1981, which was expected to bring "psychiatry's best talent and current knowledge before the reading public. "35 The press was soon publishing more than thirty books a year, with Sabshin happily noting in 1983 that the books "will provide much positive public education about the profession."36 The APA also set up committees to review the textbooks it published, intent on making sure that authors stayed on message. Indeed, in 1986, as it readied publication of Treatment of Psychiatric Disorders, the APA's Roger Peele—one of the organization's elected officials—worried anew about this concern. "How do we organize 32,000 members for advocacy?" he asked. "Who should be allowed to speak to the issue of the treatment of
THE RISE OF AN IDEOLOGY • 273
psychiatric illness? Only researchers? Only the academic elite? .. . Only members appointed by APA presidents?"37
Very early on, the APA realized that it would be valuable to develop a nationwide roster of "experts" that could promote the medical-model story to the media. It established a "public affairs institute" to oversee this effort, which involved training members "in techniques for dealing with radio and television." In 1985 alone, the APA ran nine "How to Survive a Television Interview" workshops.38 Meanwhile, every district branch in the country identified "public affairs representatives" who could be called on to speak to the press. "We now have an experienced network of trained leaders who can effectively cope with all varieties of media," Sabshin said.39
Much like any commercial organization selling a product, the APA regularly courted the press and exulted when it received positive coverage. In December 1980, it held a daylong media conference on "new advances in psychiatry" that "was attended by representatives of some of the nation's most prestigious and widely circulated newspapers," Sabshin crowed.° Next, it placed "public service spots" on television to tell its story, an effort that included sponsoring a two-hour program on cable television titled Your Mental Health. It also developed "fact sheets" for distribution to the media that told of the prevalence of mental disorders and the effectiveness of psychiatric drugs. Harvey Rubin, chair of the APA's public affairs committee, taped a popular radio program that carried the medical-model message to listeners around the country.41 The APA had launched an all-out media blitz—it handed out awards to journalists whose stories it liked—and every year Sabshin detailed the good publicity this effort was generating. In 1983, he noted that "with the help and urging of the Division of Public Affairs, U.S. News and World Report published a major cover story on depression, which included substantial quotes from prominent psychiatrists."42 Two years later, Sabshin announced that "APA spokespersons were placed on the Phil Donahue program, Nightline and other network programs." That same year, it "helped develop a Reader's Digest book chapter on mental health."43
All of this paid big dividends. Newspaper and magazine head-
THE RISE OF AN IDEOLOGY • 275
all the latest advances in scientific research, and for the first time in history, providing a systematic method of diagnosis, treatment, cure and even prevention of mental suffering." In the past few years, Gold added, psychiatry had conducted "some of the most incredible medical research ever done. . . . We have probed the frontiers of science and human understanding wherein lie the ultimate comprehension and cure of all mental illnesses."46
If there was one book that cemented this belief in the public's mind, it was The Broken Brain. Published in 1984 and written by Nancy Andreasen, future editor of the American Journal of Psychiatry, it was touted as "the first comprehensive account of the biomedical revolution in the diagnosis and treatment of mental illness." In it, Andreasen concisely set forth the tenets of biological psychiatry: "The major psychiatric illnesses are diseases. They should be considered medical illnesses just as diabetes,' heart disease, and cancer are. The emphasis in this model is on carefully diagnosing each specific illness from which the patient suffers, just as an internist or neurologist would."47
The broken brain—hers was a book with a brilliant title, one that conveyed a bottom-line message that the public could easily grasp and remember. However, what most readers failed to notice was that Andreasen, in several places in her book, confessed that re-searchers had not yet actually found that people diagnosed with psychiatric disorders have broken brains. Researchers had new tools for investigating brain function, and they hoped this knowledge would come. "Nevertheless, the spirit of a revolution—the sense that we are going to change things dramatically, even if the process requires a number of years—is very much present," Andreasen explained.48
Twenty-five years later, that breakthrough moment still lies in the future. The biological underpinnings of schizophrenia, depression, and bipolar disorder remain unknown. But the public has long since been convinced otherwise, and we can see now the marketing process that got this delusion under way. At the start of the 1980s, psychiatry was worried about its future. p 275
Sales of psychiatric drugs had notably declined in the past seven years, and few medical school graduates wanted to go into the field. In response, the APA
274 • ANATOMY OF AN EPIDEMIC
lines now regularly told of a "revolution" under way in psychiatry. Readers of the New York Times learned that "human depression is linked to genes" and that scientists were uncovering the "biology of fear and anxiety." Researchers, the paper reported, had discovered "a chemical key to depression."'" Societal belief in biological psychiatry was clearly taking hold, just as the APA hoped, and in 1984, Jon Franklin of the Baltimore Evening Sun wrote a seven-part series titled "The Mind-Fixers" on the astonishing advances that were being made in the field.45 He put this revolution into a historical context:
Since the days of Sigmund Freud the practice of psychiatry has been more art than science. Surrounded by an aura of witchcraft, proceeding on impression and hunch, often ineffective, it was the bumbling and sometimes humorous stepchild of modern science. But for a decade and more, research psychiatrists have been working quietly in laborato-ries, dissecting the brains of mice and men and teasing out the chemical formulas that unlock the secrets of the mind. Now, in the 1980s, their work is paying off. They are rapidly identifying the interlocking molecules that produce human thought and emotion. . . . As a result, psychiatry today stands on the threshold of becoming an exact science, as precise and quantifiable as molecular genetics. Ahead lies an era of psychic engineering, and the development of specialized drugs and therapies to heal sick minds.
Franklin, who interviewed more than fifty leading psychiatrists for his series, called this new science "molecular psychiatry," which was "capable of curing the mental diseases that afflict perhaps 20 percent of the population." He was awarded the Pulitzer Prize for expository journalism for this work.
Books written by psychiatrists for the lay press at this time told a similar story. In The Good News About Depression, Yale University psychiatrist Mark Gold informed readers that "we who work in this new field call our science biopsychiatry, the new medicine of the mind. . . . It returns psychiatry to the medical model, incorporating
278 • ANATOMY OF AN EPIDEMIC
talking about the drawbacks of psychiatric medications, he would not be invited back. There would be no industry-sponsored symposiums on "supersensitivity psychosis," or the addictive effects of benzodiazepines, or how antidepressants were no more effective than active placebo. These speakers came to be known as "thought leaders," their presence on the symposium panels elevating them to the status of "stars" in the field, and by the early 2000s, they were getting paid $2,000 to $10,000 per speech. "Some of us," confessed E. Fuller Torrey, "believe that the present system is approaching a high-class form of prostitution."55
These "thought leaders" also became the experts regularly quoted by the media, and they wrote the textbooks publithed by the APA. Psychiatry's thought leaders shaped our society's understanding of mental disorders, and once they began serving as paid speakers, the pharmaceutical companies sent money their way through multiple channels. As the New England Journal of . Medicine observed in 2000, thought leaders "serve as consultants to companies whose products they are studying, join advisory boards and speakers' bureaus, enter into patent and royalty arrangements, agree to be the listed authors of articles ghostwritten by interested companies, promote drugs and devices at company-sponsored symposiums, and allow themselves to be plied with expensive gifts and trips to luxurious settings."56 Nor was it just a few psychiatrists from academia that pharma courted with its dollars. The drug industry understood this was a very effective way to market their drugs, and collectively the companies began paying money to virtually every well-known figure in the field. In 2000, when the New England Journal of Medicine tried to find an expert to write an
* The academic psychiatrists also began to regularly give dinner talks to local psychiatric groups, and in 2000, University of Mississippi psychiatrist John Norton confessed in a letter to the New England Journal of Medicine that after he wrote about the side effects of the sponsor's drug, "my invitations to speak suddenly dropped from four to six times per month to essentially none." Prior to that experience, he said, "I deluded myself into thinking I was educating physicians, and not being swayed by the sponsors."
THE RISE OF AN IDEOLOGY • 279
editorial on depression, it "found very few who did not have financial ties to drug companies that make antidepressants."
The NIMH also joined this storytelling coalition. The biological psychiatrists knew that they had successfully captured the NIMH when the Soteria Project was closed and Mosher was ousted, and during the 1980s the NIMH actively promoted the biological psychiatry story to the public, an effort that took wing under the leadership of Shervert Frazier. Prior to being picked to head the NIMH in 1984, Frazier directed the APA's Commission on Public Affairs, which had run the media-training workshops underwritten by pharmaceutical firms, and soon Frazier was announcing that the NIMH, for the first time in its forty-year history, would launch a major educational campaign called the Depression Awareness, Recognition and Treatment (DART) program. This educational effort would inform the public that depressive disorders are "common, serious and treatable," the NIMH said. Pharmaceutical companies would "contribute resources, knowledge and other forms of assistance to the project," which the NIMH primnised would run for at least a decade.57 As it helped expand the market for psychiatric medica-tions, the NIMH even assured the public that the broken-brain story was true. "Two decades of research have shown that [psychiatric disorders] are diseases and illnesses like any other diseases and illnesses," said NIMH director Lewis Judd in 1990, even though nobody had ever been able to explain the nature of the pathology.'"
The final group to participate in this storytelling campaign was the National Alliance for the Mentally Ill. Founded in 1979 by two Wisconsin women, Beverly Young and Harriet Shelter, it arose as a grassroots protest to Freudian theories that blamed schizophrenia on "aloof, uncaring mothers and preoccupied mothers who were unable to bond with their infants," a NAMI historian observed. fn 59 NAMI was eager to embrace an ideology of a different kind, and the message it sought to spread, said former NAMI president Agnes Hatfield in 1991, was that "mental illness is not a mental health problem; it is a biological illness. There is considerable clarity on the part of families that they are focusing on a physical disease." fn 60, p 279
For the APA and pharma companies, the emergence of NAMI could not have come at, a more opportune moment. This was a
280 • ANATOMY OF AN EPIDEMIC
parents' group eager to embrace biological psychiatry, and both the APA and pharmaceutical firms pounced. In 1983, the APA "entered into an agreement with NAMI" to write a pamphlet on neuroleptic drugs, and soon the APA was encouraging its branches across the country "to foster collaborations with local chapters of the National Alliance for the Mentally Ill."61 The APA and NAMI joined together to lobby Congress to increase funding for biomedical research, and the beneficiary of that effort, the NIMH—which saw its research budget soar 84 percent during the 1980s—thanked the parents for it. "The NIMH in a very meaningful sense is NAMI's institute," Judd told NAMI president Laurie Flynn in a 1990 letter.62 By that time, NAMI had more than 125,000 members, most of whom were middle-class, and it was busily seeking to "educate the media, public officials, healthcare providers, educators, the business community, and the general public about the true nature of brain disorders," said one NAMI leader.63 NAMI brought a powerful moral authority to the telling of the broken-brain story, and naturally pharmaceutical companies were eager to fund its educational programs, with eighteen firms giving NAMI $11.72 million from 1996 to 1999.64
In short, a powerful quartet of voices came together during the 1980s eager to inform the public that mental disorders were brain diseases. Pharmaceutical companies provided the financial muscle. The APA and psychiatrists at top medical schools conferred intellectual legitimacy upon the enterprise. The NIMH put the government's stamp of approval on the story. NAMI provided a moral authority. This was a coalition that could convince American society of almost anything, and even better for the coalition, there was one other voice on the scene that, in its own way, helped make the story bulletproof in society's eyes. p 280 (great summary verse for book)
The Critics Believe in Aliens
The story of a "psychopharmacology revolution" had first been
told in the 1950s and 1960s, and then, as we've seen in this chapter,
it was revived in the 1980s. However, the storytellers in the 1980s
THE RISE OF AN IDEOLOGY • 281
were more vulnerable to criticism than the storytellers of the earlier decades simply because there was now twenty years of research that undermined their narrative. None of the drugs had proven to help people function well over the long term, and the chemical-imbalance theory of mental disorders was in the process of flaming out. As NIMH researchers had concluded in 1984, "elevations or decrements in the functioning of serotonergic systems per se are not likely to be associated with depression." Close readers of The Broken Brain could also see that, in fact, no great new discoveries had been made. There was a Grand Canyon–sized gap between what the broken-brain storytellers were intimating was true and what was actually known, and that same gap would appear in their stories when Prozac and the other second-generation drugs came to market. But fortunately for the proponents of biological psychiatry, criticism of the medical model and of psychiatric drugs became associated, in the public mind, with Scientology.
L. Ron Hubbard, a science-fiction writer, founded the Church of Scientology in 1952. One of the church's core tenets is that the earth is populated by souls that previously lived on other planets, an "extraterrestrial" creation myth that could have been lifted directly from a sci-fi novel. In addition, Hubbard had his own ideas about how to heal the mind. Prior to founding Scientology, he had published Dianetics: The Modern Science of Mental Health, which outlined the use of an "auditing" process to eliminate painful past experiences from the mind. The scientific and medical community ridiculed dianetics as quackery and dismissed Hubbard as a huckster, and he in turn developed an intense hatred for psychiatry. In 1969, Scientology and Thomas Szasz cofounded the Citizens Commission on Human Rights, and this group began waging campaigns against lobotomy, electroshock, and psychiatric drugs.
This proved to be very fortuitous for the APA and its storytelling partners as they raised the flag of biological psychiatry. Indeed, it is easy to imagine the drug companies deciding to secretly fund Scientology's protests, eager as they were to shove money to any organ-ization that would—wittingly or unwittingly—advance their cause. For not only did Scientologists believe in extraterrestrials, they also had gained a reputation for being a secretive, litigious, and even
286 • ANATOMY OF AN EPIDEMIC
in court, the use of benzodiazepines was "scientifically bad," as it would "confound the results" and "interfere with the analysis of both safety and efficacy," but it enabled the company to continue development of fluoxetine.6
Still, even with addition of the benzodiazepines, fluoxetine failed to perform well. During the early 1980s, the company conducted a phase III trial of the drug in Germany, and in 1985, the German licensing authority, Bundesgesundheitsamt (BGA), concluded that this drug was "totally unsuitable for the treatment of depression. "7 According to the patients' "self ratings" (as opposed to the doctors' ratings), the drug produced "little response or no improvement in the clinical picture of the patients," the BGA noted.' At the same time, it had caused psychosis and hallucinations, and increased some patients' anxiety, agitation, and insomnia, "which as adverse effects exceed those which are considered acceptable by medical standards," the BGA wrote.9 Most problematic of all, this drug treatment could prove fatal. "Sixteen suicide attempts were made, two of these with success," the BGA said.1° A German Eli Lilly employee privately calculated that the incidence rate of suicidal acts for the fluoxetine patients was "5.6 times higher than under the other active medication, imipramine."11
With Germany having rejected its application, Eli Lilly naturally worried that it would be unable to gain FDA approval for fluoxetine.* It needed to hide the suicide data, and in a 1994 civil lawsuit, Nancy Lord, an expert in clinical trial design, explained how the company did it. First, Eli Lilly instructed investigators to record various drug-related adverse events as "symptoms of depression." As such, in the trial results submitted to the FDA, the problems were attributed to the disease rather than to fluoxetine. Second, when Eli Lilly scientists tabulated the data from case report forms, they changed individual reports of "suicidal ideation" to "depression." Third, Lilly employees went through the German data "and pulled out [suicide] cases that they didn't think were suicide."12
All of these shenanigans, Lord told a court in 1994, made the
* At the end of 1989, Eli Lilly obtained approval to market fluoxetine in Germany, but with a label that warned of the elevated risk of suicide.
THE STORY THAT WAS . . . AND WASN'T TOLD • 287
entire testing process scientifically "worthless." Yet even with these statistical manipulations, Eli Lilly still struggled to present a convincing case for fluoxetine in its application to the FDA. It had conducted placebo-controlled trials at eight sites, and in four of them, the fluoxetine patients had fared no better than the placebo group, and in the others, fluoxetine was only slightly better than a placebo.13 Meanwhile, when Peter Breggin reviewed Lilly's documents, he discovered that imipramine had proven to be more effective than fluoxetine in six of seven trials.14 The FDA, in its March 28, 1985, review of one large trial, made the same observation: "Imipramine was clearly more effective than placebo, whereas fluoxetine was less consistently better than placebo."15 At best, fluoxe-tine's efficacy was of a very marginal sort, and FDA reviewer Richard Kapit also worried about its safety. At least thirty-nine patients treated with fluoxetine had gone psychotic in the short trials, and slightly more than 1 percent had become manic or hypomanic. Other side effects included insomnia, nervousness, confusion, dizziness, memory dysfunction, tremors, and impaired motor coordination. Fluoxetine, Kapit concluded, "may negatively affect patients with depression."16 The FDA also understood that Eli Lilly had tried to hide many of these problems, the company having engaged in "large-scale underreporting" of the harm that fluoxetine could cause, according to reviewer David Graham.17
While the trials may have been scientifically worthless, they nevertheless proved to be an accurate forecast of what happened after Prozac was brought to market. There were numerous anecdotal accounts of Prozac-treated patients committing horrendous crimes or killing themselves, and so many adverse-events reports flowed into the FDA's MedWatch program that Prozac quickly became America's most complained about drug. By the summer of 1997, the FDA had received thirty-nine thousand such reports about Prozac, far outstripping the number received by any other drug for that nine-year period (1988-1997). The MedWatch filings told of hundreds of suicides, and of a long list of vexing side effects, which included psychotic depression, mania, abnormal thinking, hallucinations, hostility, confusion, amnesia, convulsions, tremors, and sexual dysfunction.° The FDA estimates that only 1 percent of
290 • ANATOMY OF AN EPIDEMIC
After the NIMH announced its plans for DART in 1986, it had studied the public's beliefs about depression. A survey revealed that only 12 percent of American adults would take a pill to treat it. Seventy-eight percent said they "would live with it until it passed," confident they could handle it on their own. This was an attitude consistent with what the NIMH had preached only fifteen years earlier, when Dean Schuyler, head of the depressive section, had told the public that most depressive episodes "will run their course and terminate with virtually complete recovery without specific intervention." There was epidemiological wisdom in the public's belief that depression would pass, but the NIMH—once Shervert Frazier and other biological psychiatrists took the helm—was intent on delivering a different message.
The purpose of DART, the NIMH explained in 1988, was "to change public attitudes so that there is greater acceptance of depression as a disorder rather than a weakness." The public needed to understand that it regularly went "underdiagnosed and under-treated," and that it could "be a fatal disease" if left untreated. There were 31.4 million Americans who suffered from at least a mild form of depression, the NIMH said, and it was important that they get diagnosed. The public needed to be made aware that anti-depressants produced recovery rates of "70% to 80% in comparison with 20% to 40% for placebo." The NIMH vowed to continue DART indefinitely in order to "inform" the public of these "facts."27
The NIMH officially launched DART in May 1988, five months after Prozac landed on pharmacy shelves. The NIMH enlisted "labor, religious, educational groups" and businesses to help it spread its message, and of course pharmaceutical companies and NAMI had been on board from the start. The NIMH ran advertisements in the media, and Eli Lilly helped pay for the printing and distribution of 8 million DART brochures titled "Depression: What You Need to Know." This pamphlet informed readers, among other things, of the particular merits of "serotonergic" drugs for the disease. "By making these materials on depressive illness available, accessible in physicians' offices all over the country, important information is effectively reaching the public in settings which
THE STORY THAT WAS . . . AND WASN'T TOLD • 291
encourage questions, discussion, treatment, or referral," said NIMH director Lewis Judd.28
The remaking of the American mind was under way. This selling of depression, which was being done under the guise of a "public education" campaign, turned into one of the most effective marketing efforts ever devised. Newspapers picked up on this story, sales of Prozac began to soar, and then, on December 18, 1989, the green-and-white pill officially gained celebrity status when New York magazine put it on its cover. BYE, BYE BLUES, the headline screamed. A NEW WONDER DRUG FOR DEPRESSION. In the article,
one "anonymous" user of Prozac said that on a scale of 1 to 100, he now felt "over 100." Thanks to this new miracle pill, the magazine concluded, psychiatrists felt that their "profession has been buoyed. "29
Other such glowing stories quickly followed. On March 26, 1990, Newsweek's cover featured the green-and-white capsule floating Nirvana-like over a beautiful landscape. PROZAC: A BREAKTHROUGH DRUG FOR DEPRESSION the magazine announced. Physi-
cians were now writing 650,000 prescriptions for the pill each month, and "nearly everyone has something nice to say about the new treatment," Newsweek said. Patients were loudly exclaiming, "I never felt better!"" Three days later, Natalie Angier of the New York Times, who arguably was the nation's most popular science writer, explained that antidepressants "work by restoring the balance of neurotransmitter activity in the brain, correcting an abnormal excess or inhibition of the electrochemical signals that control mood, thoughts, appetite, pain and other sensations." This new drug, Dr. Francis Mondimore told Angier, "is not like alcohol or Valium. It's like antibiotics."31 Television shows weighed in with a similar message, and on 60 Minutes, Lesley Stahl told the inspiring story of a woman, Maria Romero, who, after a decade of horrible depression, had been reborn on Prozac. "Somebody, something left my body and another person came in," Romero said. Stahl happily explained the biological cure that was at work: "Most doctors believe that chronic depression like Romero's is caused by a chemical imbalance in the brain. To correct it, the doctor prescribed Prozac."32
292 • ANATOMY OF .AN EPIDEMIC
Scientology to the Rescue
Fairly early on, there was a moment when this wonder-drug story threatened to fall apart. The problem, of course, was that fluoxetine did in fact stir suicidal and violent thoughts in some people, and during the summer of 1990, the issue of Prozac's safety burst into the news. And it was then, at that critical moment, that Scientology proved so useful to Eli Lilly and the psychiatric establishment.
By 1990, so many people had suffered bad reactions to fluoxetine that a national Prozac Survivors Support Group had formed. Many harmed by the drug had taken their complaints to lawyers, and two lawsuits in particular grabbed the public's attention. First, on July 18, newspapers reported that a Long Island woman, Rhoda Hala, was suing Eli Lilly because, after going on Prozac, she had slashed her wrists and "other parts of her body hundreds of times."33 Two weeks later, newspapers reported on a lawsuit related to a mass murder committed by a crazed Kentucky man. Five weeks after starting the drug, Joseph Wesbecker walked into a Louisville printing plant where he had worked and opened fire with an AK-47 assault rifle, killing eight and wounding twelve. The Citizens Commission on Human Rights quickly issued a press release urging Congress to ban this "killer drug," and that's when Eli Lilly pounced. These lawsuits, Eli Lilly loudly announced, "are being drummed up by the Scientology group, which has a history of criti-cizing the use of psychiatric drugs."34
This was the start of Eli Lilly's campaign to save its blockbuster drug. "Lilly can go down the tubes if we lose Prozac," wrote chief medical officer Leigh Thompson, in a harried 1990 memo." The company quickly honed a four-point message for the media: This was an issue being raised by Scientologists; extensive clinical trials had shown that Prozac was a safe drug; the suicidal and homicidal events were "in the disease, not the drug"; and "people who could be helped are being scared away from treatment, and that's the real public menace."36 The company ran media-training sessions for the academic psychiatrists it hired as consultants, getting them to practice their delivery of this message. "Frankly, I was unimpressed with
THE STORY THAT WAS . . AND WASN'T TOLD • 293
the performance of our outside professionals," company vice-president Mitch Daniels complained to Thompson after one such practice session in April 1991. The company would "mandate" that the academic psychiatrists perform better "in their future training sessions," he said.37
An article that appeared in the Wall Street Journal on April 19, 1991, showed that Eli Lilly's training sessions had paid off. "Scientology," the paper informed its readers, was a "quasi-religious/ business/paramilitary organization" that was "waging war on psychiatry." The group had attacked Prozac's safety even though "doctors unaffiliated with Lilly" had found, during the clinical trials, that there was "a lower tendency toward suicidal thinking with Prozac than with other antidepressants, or with the starch capsules given to a control group." It was, Leigh Thompson said, a "demoralizing revelation to watch twenty years of solid research by doctors and scientists shouted down in twenty-second sound bites by Scientologists and lawyers." Indeed, the Wall Street Journal reported, Eli Lilly, in response to concerns about Prozac's safety, had asked "suicide experts" to re-scrutinize the trial data, but they had "concluded that nothing in the clinical trials linked suicidal thinking—common in depression patients—to Prozac." It was the disease, not the drug, and that was the tragedy, explained Jerrold Rosenbaum, a Harvard psychiatrist at Massachusetts General Hospital. "The public's fear of Prozac as a result of this campaign has itself become a potentially serious public-health problem as people stay away from treatment.""
Rosenbaum, naturally, was one of Eli Lilly's "outside professionals." As the Boston Globe later reported, he "sat on a marketing advisory panel for Lilly before Prozac was launched," his relationship to Eli Lilly a "cozy" one." But the Wall Street Journal presented him as an independent expert, one of the nation's top depression doctors, and so readers could only draw one conclusion: This was an issue conjured up by noxious Scientologists, rather than a legitimate concern. Other newspapers and magazines framed the issue in that way, with Time, in May of that year, publishing a scathing cover story on Scientology, calling it a "criminal organization" that attracted "psychopaths."4°
294 • ANATOMY OF AN EPIDEMIC
On September 20, 1991, the FDA did convene a hearing on whether Prozac elevated the risk of suicide, but the advisory panel, which was dominated by physicians with ties to pharmaceutical companies, showed little interest in seriously investigating this question. Although more than two dozen citizens testified on the harm that the drug could cause, the panel made sure that the scientific discussion was limited to presentations that supported Eli Lilly's position that fluoxetine was perfectly safe. As the Wall Street Journal reported, the scientific data presented at the hearing proved that "fluoxetine doesn't lead to increased suicide or suicidal thinking, and, in fact, show that the drug helps alleviate these conditions." The entire controversy, one Lilly supporter told the Journal, was a "complete fiction" that had been "organized and funded by an anti-psychiatric group. '541
At that moment, Eli Lilly and all of psychiatry had achieved a public relations victory of lasting importance. The wonder-drug aura around Prozac had been restored, and the public and the media had been conditioned to associate criticism of psychiatric drugs with Scientology. The debate over the merits of these drugs now seemed to feature the nation's top scientists and doctors on one side and religious kooks on the other, and if that were so, the public could be certain where the truth lay. p 294
Other SSRIs came to market, sales of Prozac hit the $1 billion mark in 1992, and then, in 1993, Brown University psychiatrist Peter Kramer, in his book Listening to Prozac, pushed the wonder-drug story up a notch. Prozac, he wrote, was making some patients "better than well." An era of "cosmetic psychopharmacology" was dawning, Kramer suggested, with psychiatry likely to have pills in the near future that could give normal people whatever personality they wanted. His book spent twenty-one weeks on the New York Times bestseller list, and soon Newsweek was warning readers that it was time for society to start grappling with the ethical questions raised by psychiatry's new powers. "The same scientific insights into the brain that led to the development of Prozac are raising the prospect of nothing less than made-to-order, off-the-shelf personalities," Newsweek explained in 1994. Will those who refuse to "give their brain a makeover," the magazine asked, be left behind?
THE STORY THAT WAS . . . AND WASN'T TOLD • 295
Gushed neuropsychiatrist Richard Restak: "For the first time in human history, we will be in a position to design our own brains. "42
America Fooled
As the Prozac story unfolded in the media, surely the ghost of John Brinkley was smiling somewhere. He had transfixed listeners to his radio show with tales of the wonders of transplanted goat gonads, and now here was a storytelling process that had transformed a drug "totally unsuited" for treating depression into a miracle compound, with psychiatrists publicly wringing their hands over their new godlike powers to shape the human mind. Should they worry about making people "better than well"? Would our society lose something precious if everybody were happy all the time? The widespread medicating of the American mind was now under way, and—as a very quick review will reveal—it was this same storytelling process that supported the launch of Xanax as a drug for panic disorder and the atypical antipsychotics for schizophrenia. Once those "second-generation" drugs became blockbusters, the drug companies and academic psychiatrists began touting psychiatric drugs of all kinds for use in children, this storytelling sweeping millions of American youth into the "mental illness" bin.
Xanax
Xanax (alprazolam) was approved by the FDA as an anti-anxiety agent in 1981, and then Upjohn set out to get it approved for panic disorder, which had been newly identified as a discrete condition for the first time in DSM-III (1980). As a first step, it hired former NIMH director Gerald Klerman to co-chair its "steering committee" for the testing process, and it paid Daniel Freedman, editor of the Archives of General Psychiatry, to be an assistant to its "division of medical affairs."43 This was just part of the company's efforts to co-opt academic psychiatry: "The most senior psychiatrists in the world were flooded with offers of consultancies" from
296 • ANATOMY OF AN EPIDEMIC
Upjohn, said Isaac Marks, an expert in anxiety 'disorders at the Institute of Psychiatry in London."
Klerman and Upjohn designed Upjohn's Cross National Collaborative Panic Study in a manner that could be expected to produce a poor placebo response. Patients who had been on benzodiazepines were allowed into the study, which meant that many in the placebo group would in fact be going through the horrors of benzodiazepine withdrawal, and thus could be expected to be extremely anxious during the first weeks of the trial. Nearly one-fourth of the placebo patients had traces of benzodiazepines in their blood when the treatment period began.45
Benzodiazepines are known to work quickly, and that proved true in this study. At the end of four weeks, 82 percent of the alprazolam patients were "moderately improved" or "better," versus 43 percent of the placebo group. However, during the next four weeks, the placebo patients continued to improve, while the alprazolam patients did not, and by the end of the eighth week, there "was no significant difference between the groups" on most of the rating scales, at least among the patients who remained in the study. The alprazolam group also experienced a variety of troubling side effects: sedation, fatigue, slurred speech, amnesia, and poor coordination. One of every twenty-six alprazolam patients suffered a "serious" reaction to the drug, such as mania or aggressive behavior.46
At the end of eight weeks, the patients were tapered from their medication for four weeks and then followed while medication-free for another two weeks. The results were predictable. Thirty-nine percent of those withdrawn from alprazolam "deteriorated signifi-cantly," their panic and anxiety skyrocketing to such an extent they had to start taking the medication again. Thirty-five percent of the alprazolam patients suffered "rebound" panic and anxiety symptoms more severe than when the study began, and an equal percentage suffered a host of debilitating new symptoms, including confusion, heightened sensory perceptions, depression, a feeling that insects were crawling over them, muscle cramps, blurred vision, diarrhea, decreased appetite, and weight loss.47
In sum, at the end of fourteen weeks, the drug-exposed patients were worse off than the placebo group: They were more phobic,
THE STORY THAT WAS . . . AND WASN'T TOLD • 297
The Xanax Study
In Upjohn's study of Xanax, patients were treated with the drug or placebo for eight weeks. Then this treatment was slowly withdrawn (weeks 9 through 12), and during the last two weeks patients didn't receive any treatment.The Xanax patients fared better during the first four weeks, which is the result that the Upjohn investigators focused on in their journal articles. However, once the Xanax patients began withdrawing from the the drug, they suffered many more panic attacks than the placebo patients, and at the end of the study were much more symptomatic. Source: Ballenger, C."Alprazolam in panic disorder and agoraphobieArchives of General Psychiatry 45 (1988): 413-22. Pecknold, C."Alprazolam in panic disorder and agoraphobia:' Archives of General Psychiatry 45 (1988): 429-36.
more anxious, more panic stricken, and doing worse on a "global scale" that assessed overall well-being. Forty-four percent had been unable to get off the drug, on their way to a lifetime of addiction. In every way, the results painted a powerful portrait of the benzo trap: This was a drug that worked for a short time, then its efficacy over a placebo petered out, and yet when patients tried to go off the drug, they became quite sick and many couldn't kick the habit. The first few weeks of relief came at a very high long-term cost, with those stuck on the drug—as previous benzodiazepine studies had shown—likely to end up physically, emotionally, and cognitively impaired.
The Upjohn investigators published three articles in the Archives of General Psychiatry in May 1988, and anyone who carefully reviewed the data could see the harm caused by alprazolam. But in order for Xanax to be successfully marketed, Upjohn needed its in-vestigators to draw a different sort of conclusion, and so they did,
298 • ANATOMY OF AN EPIDEMIC
particularly in the abstracts of the three articles. First, they focused their attention on the four-week results (rather than the eight-week outcomes at the end of the treatment period), announcing that "alprazolam was found to be effective and well-tolerated."48 Next, they noted that 84 percent of the alprazolam patients had finished the eight-week study, which was evidence that "patient acceptance of alprazolam was high." Although their alprazolam patients regularly exhibited such problems as "slurred speech, amnesia" and other signs of "impaired mentation," they still concluded that the drug had "few side effects and is well tolerated."'" Finally, while they acknowledged that some alprazolam patients fared poorly when the drug was withdrawn, they reasoned that it had been used for too short a period and the withdrawal done too abruptly. "We recommend that patients with panic disorder be treated for a longer period, at least six months," they said.5°
In London, Isaac Marks and several of his colleagues at the Institute of Psychiatry subsequently pointed out how transparently ridiculous this all was. In a letter to the Archives of General Psychiatry, they observed that since the alprazolam patients "were in a worse state than patients receiving placebo" at the end of the study, the finding by the Upjohn investigators that the drug was effective and well tolerated could only be seen as "biased and arguable."51 The entire affair, Marks subsequently wrote, "is a classic demon-stration of the hazards of research funded by industry." fn 52
Yet the fact that the alprazolam patients came to such a bad end, with many on a path to a lifelong addiction, did not deter Upjohn, Klerman, the APA, and the NIMH from touting Xanax's benefits to the American public. The same marketing machinery that had made Prozac a bestseller was rolled out again. Upjohn sponsored a symposium at the APA's 1988 meeting where the "expert panel" highlighted the four-week results. Robert Pasnau, who had been head of the APA in 1987, sent a glossy booklet on the Consequences of Anxiety to APA members, an "educational" effort paid for by Upjohn. Both Shervert Frazier and Gerald Klerman penned a "Dear Doctor" letter that Upjohn included in the promotional literature it sent to doctors about Xanax as a treatment for panic disorder. Up-john also gave $1.5 million to the APA so that it could mount a
THE STORY THAT WAS . . . AND WASN'T TOLD • 299
DART-like campaign to "educate" psychiatrists, health-care workers, and the public about panic disorder, which was said to be "under-recognized and undertreated."53 Finally, the NIMH chipped in too, identifying panic disorder as a priority concern and sponsoring a conference in 1991 on it, with its panel of experts designating "high potency benzodiazepines"—this would be Xanax—as one of the two "treatments of choice."54
The FDA approved Xanax as a treatment for panic disorder in November 1990, and many newspapers and magazines ran the
usual features. IN A PANIC? HELP IS ON THE WAY, a St. Louis Post-
Dispatch headline announced. Treatment, the paper said, helped 70 to 90 percent of those with the debilitating condition, which afflicted "4 million adults in this country."55 The Associated Press explained that "a biochemical malfunctioning in the brain is believed to be one of the causes of panic attacks. Xanax can block the attacks by interacting with several different systems in the brain."56In the Chicago Sun-Times, Dr. John Zajecka at Rush Medical College in Chicago announced that "Xanax is the fastest acting and least toxic" of medications for the disorder.57 Once again, a very effective, safe drug had arrived on the market, and in 1992, Xanax became the fifth most frequently prescribed medication in the United States.58
Not so atypical
Even as Xanax was on the way to market as a treatment for panic disorder, Janssen was conducting tests of risperidone, a new drug for schizophrenia. By this time, the methods that pharmaceutical firms were employing to create new "blockbuster" psychotropics were becoming quite well practiced, with nearly everyone employing the Prozac model of drug development, and so Janssen, like Eli Lilly and Upjohn, designed trials that were biased in favor of its drug. In particular, Janssen compared multiple doses of risperidone to a high dose of haloperidol (Haldol), as it could then be relatively certain that one of the risperidone doses would have a good safety profile in comparison to the old "standard" neuroleptic. As FDA reviewers noted, these studies were "incapable" of providing any
300 • ANATOMY OF AN EPIDEMIC
meaningful comparison of the two drugs." In the FDA's letter of approval to Janssen, Robert Temple, director of the Office of Drug Evaluation, made this clear:
We would consider any advertisement or promotion labeling for RISPERDAL false, misleading, or lacking fair balance under section 502 (a) and 502 (n) of the ACT if there is presentation of data that conveys the impression that risperidone is superior to haloperidol or any other marketed antipsychotic drug product with regard to safety or effectiveness.60
However, while the FDA could prohibit Janssen from placing advertisements touting its drug as superior to haloperidol, it did not have authority over what the academic psychiatrists hired by Janssen could say. This was the commercial beauty of the "partner-ship" that had emerged between psychiatry and the pharmaceutical industry during the 1980s—the academic doctors could make claims, both in their medical journals and to the public, that the FDA considered false in kind. In this case, they published more than twenty articles in psychiatric journals touting risperidone as equal or superior to haloperidol in reducing positive symptoms of schizophrenia (psychosis) and superior to haloperidol in improving negative symptoms (lack of emotion). The academic doctors reported that risperidone reduced hospital stays, improved the patient's ability to function socially, and reduced hostility. "Risperidone has important advantages compared with haloperidol," they wrote in the Journal of Clinical Psychiatry. "When administered in an effective dose range, risperidone produced greater improvements on all five dimensions of schizophrenia."6'
Once again, this was a scientific story of a new and improved treatment, and in their interviews with the media, Janssen's investigators told of a wonder drug. This new agent, the Washington Post reported, "represents a glimmer of hope for a disease that until re-cently had been considered hopeless." Risperidone, it explained, did not "cause sedation, blurred vision, impaired memory or muscle stiffness, side effects commonly associated with an earlier generation of antipsychotic drugs."62 The New York Times, quoting
THE STORY THAT WAS . . . AND WASN'T TOLD • 30/
Richard Meibach, Janssen's clinical research director, reported that "no major side effects" had appeared in the two-thousand-plus patients treated with risperidone in the clinical trials.* The drug was thought to "relieve schizophrenia symptoms by blocking excessive flows of serotonin or dopamine, or both," the paper said."
The atypical revolution was on. Risperdal apparently restored sanity by balancing multiple neurotransmitters in the brain, and it seemed to cause no side effects of any note. In 1996, Eli Lilly brought Zyprexa (olanzapine) to market, and the public story of the wonders of atypicals got ramped up another notch.
As had become customary, Eli Lilly employed trials that were "biased by design" against haloperidol, the FDA concluded. As a result, its large phase III trial, which wasn't placebo controlled, provided "little useful efficacy data." As for olanzapine's safety profile, twenty patients treated with the drug during the trials died, 22 percent suffered a "serious" adverse 'event (higher than in the haloperidol patients), and two-thirds failed to complete the studies. Olanzapine, the data suggested, made patients sleepy and fat, and caused such problems as Parkinsonian symptoms, akathisia, dystonia, hypotension, constipation, tachycardia, diabetes, seizures, leaking breasts, impotence, liver abnormalities, and white blood cell disorders. Furthermore, warned the FDA's Paul Leber, since olanzapine blocked receptors for many types of neurotransmitters, "no one should be surprised if, upon marketing, events of all kinds and severity not previously identified are reported in association with olanzapine's use."64
That was the story told by the trial data. The story that Eli Lilly wanted to appear in the medical journals and newspapers was that Zyprexa was better than Janssen's Risperdal, and so that's the story that its hired guns told. Psychiatrists from academic medical schools announced that olanzapine worked in a more "comprehensive" manner than either risperidone or haloperidol. It was a well-tolerated
" In fact, eighty-four patients treated with risperidone had suffered a "serious adverse event," which the FDA defined as a life-threatening event or one that required hospitalization.
302 • ANATOMY OF AN EPIDEMIC
agent that led to global improvement—it reduced positive symptoms, caused fewer motor side effects than other antipsychotics, and improved negative symptoms and cognitive function.65 This second atypical was better than the first, and the Wall Street Journal ran with that angle. Zyprexa, it announced, "has substantial advantages" over other current therapies. "The real world," explained John Zajecka, from Rush Medical College, "is finding that Zyprexa has fewer extrapyramidal side effects than Risperdal."66 Zyprexa is "a potential breakthrough of tremendous magnitude," Stanford University psychiatrist Alan Schatzberg told the New York Times.67
The only question now seemed to be whether Zyprexa was truly better than Risperdal, and after AstraZeneca brought a third atypical to market, Seroquel, the media settled on the notion that collectively the new atypicals were a dramatic improvement over the older drugs. They were, Parade told its readers, "far safer and more effective in treating negative symptoms, such as difficulty in reasoning and speaking in an organized way."68 The newer drugs, the Chicago Tribune announced, "are safer and more effective than older ones. They help people go to work."69 Wrote the Los Angeles Times, "It used to be that schizophrenics were given no hope of improving. But now, thanks to new drugs and commitment, they're moving back into society like never before."7° NAMI chimed in, too, publishing a book titled Breakthroughs in Antipsychotic Medications, which helpfully explained that these new drugs "do a better job of balancing all of the brain chemicals, including dopamine and serotonin."71 On and on it went, and finally NAMI's executive director, Laurie Flynn, told the press that the promised land had at last been reached: "These new drugs truly are a breakthrough. They mean we should finally be able to keep people out of the hospital, and it means that the long-term disability of schizophrenia can come to an end."72
Lancet Asks a Question
That was the sequence of storytelling that led to the explosive rise in
the use of psychiatric drugs in the United States. First, American
THE STORY THAT WAS . . . AND WASN'T TOLD • 303
psychiatrists touted Prozac as a wonder drug, next they hailed Xanax as a safe and effective therapy for panic disorder, and finally they informed the public that atypical antipsychotics were "breakthrough" medications for schizophrenia. In this way, they rejuvenated the market for psychiatric medications, even though the clinical studies of the new drugs had not told of any therapeutic advance.
At least in scientific circles, the "wonder drug" glow around the second-generation psychotropics has long since disappeared. As we learned earlier, the SSRIs were reported in 2008 to provide a meaningful clinical benefit only to severely depressed patients. Xanax is now understood to be much more addictive than Valium, with various investigators determining that two-thirds of people who take it for any length of time have trouble getting off it." As for the top-selling atypicals, the hyping of these drugs is now viewed as one of the more embarrassing episodes in psychiatry's history, as one government-funded study after another failed to find that they were any better than the first-generation antipsychotics. In 2005, the NIMH's "CATIE Trial" determined that there were "no significant differences" between the atypicals and their predecessors, and even more troubling, in this study neither the new drugs nor the old ones could really be said to work. Seventy-four percent of the 1,432 patients were unable to stay on the medications, mostly because of their "inefficacy or intolerable side effects."74
A study by the U.S. Department of Veterans Affairs came to a similar conclusion about the relative merits of atypicals and the older drugs, and then, in 2007, British psychiatrists reported that schizophrenia patients, if anything, had a better "quality of life" on the old drugs than on the new ones. fn 75 All of this led two prominent psychiatrists to write in the Lancet that the story of the atypicals as breakthrough medications could now be "regarded as invention only," a tale concocted "by the drug industry for marketing purposes and only now being exposed." Yet, they wondered, "how is it that for nearly two decades we have, as some have put it, 'been beguiled' into thinking they were superior?" fn 76, p 303
History, as readers of this book can attest, reveals the answer to that question. The seed for the atypicals story was planted in the early 1980s, when the APA embraced "biological psychiatry" as a story that could be successfully marketed to the public. This was also a story that the field, as a whole, desperately wanted to believe in, and soon Nancy Andreasen and others were telling of a revolution that was under way, with mental illnesses finally giving up their biological secrets, even though nobody could precisely explain what those secrets were. That story gained steam, prepping the public to believe that therapeutic advances were on the way, and as pharmaceutical companies brought new medications to market, they hired the top psychiatrists in the country to tell of how these new wondrous drugs "balanced" brain chemistry. And it was that co-opting of academic medicine that gave the story its credibility. This was a story told by Harvard Medical School psychiatrist Jerrold Rosenbaum, by former NIMH director Gerald Klerman, and by Stanford University psychiatrist Alan Schatzberg.
Of course we, as a society, believed it.
Silencing Dissent
As we have seen, American psychiatry has told the public a false story over the past thirty years. The field promoted the idea that its drugs fix chemical imbalances in the brain when they do no such thing, and it grossly exaggerated the merits of the second-generation psychotropics. In order to keep that tale of scientific progress afloat (and to protect its own belief in that tale), it has needed to squelch talk about the harm that the drugs can cause.
Psychiatry's policing of its own ranks began in earnest in the late 1970s, when Loren Mosher was ousted from the NIMH for having run his Soteria experiment. The next prominent psychiatrist to end up on psychiatry's hit list was Peter Breggin. Although he is known today for his "antipsychiatry" writings, he, too, had once been on the fast track at the NIMH. After finishing his residency at a Harvard Medical School hospital, Breggin went to the NIMH in 1966 to work on developing community mental health centers. "I was still the young hotshot guy," he recalled, in an interview. "I thought
THE STORY THAT WAS . . . AND WASN'T TOLD • 305
I would be the youngest professor of psychiatry in the history of Harvard Medical School. That was the trajectory I was on."77 However, he saw that the future belonged to biological psychiatry, as opposed to the social psychiatry that interested him, and he left the NIMH to go into private practice. Soon he began writing about the hazards of electroshock and psychiatric drugs, which, he argued, "worked" by disabling the brain. After a number of heated battles with the APA's leaders, Breggin appeared in 1987 on Oprah Winfrey's television show, where he spoke about tardive dyskinesia and how that dysfunction was evidence that neuroleptics damaged the brain. His comments so infuriated the APA that it sent a transcript of the show to NAMI, which in turn filed a complaint with the Maryland State Commission on Medical Discipline, asking that it take away Breggin's medical license on the grounds that his statements had caused schizophrenia patients to stop taking their medications (and thus caused harm). Although the commission decided not to take any action, it did conduct an inquiry (rather than sum-marily dismissing NAMI's complaint), and the message to everyone in the field was, once again, quite clear.
"I think the interesting thing is that Loren [Mosher] and I took on scientifically the two sides of the issue," Breggin said. "Loren took on the issue that there is a better treatment than drugs for schizophrenia. I took on the treatments—the drugs, electroshock, and psychosurgery. And what this showed is that it didn't matter which end you wanted to take, they were willing to destroy your career. That is the lesson."
The career setback that Irish psychiatrist David Healy experienced was, in some ways, reminiscent of Mosher's fall from grace. During the 1990s, he earned a reputation as one of the field's leading historians, his writings focusing on the psychopharmacology era. He had served as secretary of the British Association for Psychopharmacology, and in early 2000, he accepted an offer from the University of Toronto's Centre for Addiction and Mental Health to head up its mood and anxiety program. Up until that moment, he was very much part of the psychiatric establishment, just as Mosher had been. However, for several years he had been interested in the question of whether SSRIs could stir suicide, and he had recently
306 • ANATOMY OF AN EPIDEMIC
completed a "healthy volunteers" study. Two of the twenty volunteers had become suicidal after they were exposed to an SSRI, which clearly showed that the drug could cause such thoughts. Not long after he accepted the Toronto job, he presented his results at a meeting of the British Association for Psychopharmacology. There, one of the most prominent figures in American psychiatry warned him to knock it off. "He told me that my career would be destroyed if I kept on showing results like the ones I'd just shown, that I had no right to bring out hazards of the pills like these," Healy said!'
In November of 2000, only a few months before he was scheduled to start his new job at the University of Toronto, Healy gave a talk on the history of psychopharmacology at a colloquium organized by the school. In his presentation, Healy spoke about problems that had arisen with neuroleptics since their introduction in the 1950s, briefly reviewed the data showing that Prozac and other SSRIs elevated the risk of suicide, and then observed in passing that outcomes for affective disorders are worse today than they were a century ago. This, he observed, shouldn't be happening if "our drugs really worked.""
Although the audience subsequently rated his talk as the colloquium's best for content, by the time Healy arrived back in Wales, the University of Toronto had rescinded the job offer. "While you are held in high regard as a scholar of the history of modern psychiatry, we do not feel your approach is compatible with the goals for development of the academic and clinical resources that we have," wrote the Centre's head psychiatrist, David Goldbloom, in an e-mail.8° Once more, others in the field could draw only one lesson. "The message is that it is a bad idea to speak out, and that the idea that treatments might not work or might not be best managed by being entrusted to doctors is beyond the pale," Healy said in an interview.81
Numerous others can attest to the fact that it is a "bad idea" to speak out. Nadine Lambert, a psychologist at the University of California at Berkeley, conducted a long-term study of children treated with Ritalin and found that, as young adults, they had elevated rates of cocaine abuse and cigarette smoking. After she reported her results at a 1998 NIH conference, the National Institute on Drug
THE STORY THAT WAS . . . AND WASN'T TOLD • 307
Abuse stopped funding her work. In 2000, when Joseph Glenmullen, a clinical instructor in psychiatry at Harvard Medical School, authored Prozac Backlash, which detailed the many problems associated with the use of SSRIs, Eli Lilly mounted a campaign to discredit him. A public-relations firm gathered critical comments from several prominent psychiatrists, who derided Glenmullen as a "nobody" in the field, and then it mailed these "reviews" to various newspapers. "It's a dishonest book, it's manipulative, it's mischie-vous," said Harvard Medical School psychiatrist Jerrold Rosenbaum, even though he was a colleague of Glenmullen's. The press release naturally did not mention that Rosenbaum was an Eli Lilly consultant.82 Next up on the chopping block: Gretchen LeFever, a psychologist at East Virginia Medical School. After she published research showing that an overly high number of children in Virginia schools were being diagnosed with ADHD, an anonymous "whistle-blower" charged her with scientific misconduct. Her federal research funds were cut off and her computers were seized, and while she was subsequently cleared of any misconduct, her career had still
been derailed.
Said Healy: "The thought-control aspect of things in psychiatry today is like old-style Eastern European social control."
Hiding the Evidence
The third aspect to the storytelling process that has led to our societal delusion about the merits of psychiatric drugs is easy to document. Imagine what our beliefs would be today if, over the past twenty years, we had opened our newspapers and read about the following findings, which represent but a sampling of the outcome -studies we reviewed earlier in the book:
1990: In a large, national depression study, the eighteen-month stay-well rate was highest for those treated with psychotherapy (30 percent) and lowest for those treated with an antidepressant (19 percent). (NIMH)
1992: Schizophrenia outcomes are much better in poor countries like India and Nigeria, where only 16 percent of patients are regularly maintained on antipsychotics, than in the United States and other rich countries, where continual drug usage is the standard of care. (World Health Organization)
1995: In a six-year study of 547 depressed patients, those who were treated for the disorder were nearly seven times more likely to become incapacitated than those who weren't, and three times more likely to suffer a "cessation" of their "principal social role." (NIMH)
1998: Antipsychotic drugs cause morphological changes in the brain that are associated with a worsening of schizophrenia symptoms. (University of Pennsylvania)
1998: In a World Health Organization study of the merits of screening for depression, those diagnosed and treated with psychiatric medications fared worse—in terms of their depressive symptoms and their general health—over a one-year period than those who weren't exposed to the drugs. (WHO)
1999: When long-term benzodiazepine users withdraw from the drugs, they become "more alert, more relaxed, and less anxious." (University of Pennsylvania)
2000: Epidemiological studies show that long-term outcomes for bipolar patients today are dramatically worse than they were in the pre-drug era, with this deterioration in modern outcomes likely due to the harmful effects of antidepressants and antipsychotics. (Eli Lilly; Harvard Medical School)
2001: In a study of 1,281 Canadians who went on short-term disability for depression, 19 percent of those who took an antidepressant ended up on long-term disability, versus 9 percent of those who didn't take the medication. (Canadian investigators)
2001: In the pre-drug era, bipolar patients did not suffer cognitive decline over the long term, but today they end up almost as cognitively impaired as schizophrenia patients. (Sheppard Pratt Health System in Baltimore)
2004: Long-term benzodiazepine users suffer cognitive deficits "moderate to large" in magnitude. (Australian scientists)
2005: Angel dust, amphetamines, and other drugs that induce psychosis all increase D2 HIGH receptors in the brain; antipsychotics cause this same change in the brain. (University of Toronto)
2005: In a five-year study of 9,508 depressed patients, those who took an antidepressant were, on average, symptomatic nineteen weeks a year, versus eleven weeks for those who didn't take any medication. (University of Calgary)
2007: In a fifteen-year study, 40 percent of schizophrenia patients off antipsychotics recovered, versus 5 percent of the medicated patients. (University of Illinois)
2007: Long-term users of benzodiazepines end up "markedly ill to extremely ill" and regularly suffer from symptoms of depression and anxiety. (French scientists)
2007: In a large study of children diagnosed with ADHD, by the end of the third year "medication use was a significant marker not of beneficial outcome, but of deterioration." The medicated children were also more likely to engage in delinquent behavior; they ended up slightly shorter, too. (NIMH)
2008: In a national study of bipolar patients, the major predictor of a poor outcome was exposure to an antidepressant. Those who took an antidepressant were nearly four times as likely to become rapid cyclers, which is associated with poor long-term outcome. (NIMH)
A check of newspaper archives reveals that the psychiatric establishment has thoroughly succeeded in keeping this information from the public. I searched for accounts of these studies in the New York Times archives and in the LexisNexis database, which covers most
308 • ANATOMY OF AN EPIDEMIC
310 • ANATOMY OF AN EPIDEMIC
U.S. newspapers, and I couldn't find a single instance where the results were accurately reported.
Newspapers, of course, would have been happy to publish these study results. However, medical news is typically generated in this way: The scientific journals, the NIH, medical schools, and pharmaceutical companies issue press releases touting certain findings as important, and reporters then sift through the releases to identify the ones they deem worthy of writing about. If no press releases are issued, or there is no other effort by the medical community to publicize the findings, then no stories appear. We can even document this blackout process at work in the NIMH's handling of Martin Harrow's outcomes study. In 2007, the year he published his results in the Journal of Nervous and Mental Disease, the NIMH issued eighty-nine press releases, many on inconsequential matters. But it did not issue one on Harrow's findings, even though his was arguably the best study of the long-term outcomes of schizophrenia patients that had ever been done in the United States." It's fair to say that if the results had been the reverse, the NIMH would have sounded the press-release gong and newspapers across the country would have touted the findings.
Although reports about most of the studies listed above simply never appeared in newspapers, there were a couple of instances when psychiatrists were forced to say something to reporters about one of the studies, and each time they spun the results. For example, when the NIMH announced the three-year results from its MTA study of ADHD treatments, it did not inform the public that stimulant usage during the third year was a "marker of deterioration." Instead, it put out a press release with this headline: IMPROVEMENT
* There were newspaper reviews of my book Mad in America that mentioned the WHO study of better schizophrenia outcomes in poor countries where patients were not regularly maintained on the drugs, and since then, this information has become somewhat known. In addition, I mentioned Martin Harrow's fifteen-year schizophrenia study in a talk I gave at Holy Cross College in February 2009, and that led to a February 8, 2009, article in the Worcester Telegram and Gazette (Mass.) that discussed Harrow's work. That was the first time that news of his study had appeared in any American newspaper.
THE STORY THAT WAS . . . AND WASN'T TOLD • 311
FOLLOWING ADHD TREATMENT SUSTAINED FOR MOST CHILDREN.
That headline told of drugs that had been beneficial, and while the text of the release did state that "continuing medication was no longer associated with better outcomes by the third year," it also included a canned quote from lead author Peter Jensen stating that there was still plenty of reason to keep children on Ritalin. "Our results suggest that medication can make a long-term difference for some children if it's continued with optimal intensity, and not started or added too late in a child's clinical course."84
If we want to get another look at this spinning process, we can turn to a 1998 New York Times article that briefly told of the WHO study on schizophrenia outcomes in rich and poor countries. After interviewing psychiatrists about the study, the Times reporter wrote that "schizophrenics generally responded better to treatment in less developed countries than in more technologically developed countries."" Responded better to treatment-,-readers could only assume that schizophrenia patients in India and Nigeria responded better to antipsychotics than patients in the United States and other rich countries did. They had no way to know that "treatment" for 84 percent of the schizophrenia patients in the poor countries consisted of being off the drugs.
In July 2009, I also searched the NIMH and NAMI websites for some mention of the studies listed above, and I found zilch. For instance, the NIMH website did not discuss the remarkable decline in bipolar outcomes in modern times, even though Carlos Zarate, who coauthored the 2000 article that documented this decline, was head of the NIMH's mood and anxiety disorders research unit in 2009. Similarly, NAMI's website didn't provide any information about Harrow's study, even though it provides reason for parents of schizophrenic children to be optimistic. Forty percent of those off medications recovered over the long term! But that finding directly contradicted the message that NAMI has promoted to the public for decades, and NAMI's website is sticking to that message. Antipsychotics, it informs the public, "correct an imbalance in the chemicals that enable brain cells to communicate with each other."86
Finally, the entire outcomes history documented in this book is missing from the 2008 edition of the APA's Textbook of Psychiatry, which means that medical students training to be psychiatrists are kept in the dark about this history." The book does not discuss "su-persensitivity psychosis." It does not mention that antidepressants may be depressogenic agents over the long term. It does not report that bipolar outcomes are much worse today than they were forty years ago. There is no discussion of rising disability rates. There is no talk about the cognitive impairment that is seen in longtime users of psychotropic drugs. The textbook authors are clearly familiar with many of the sixteen studies listed above, but, if they do mention them, they don't discuss the relevant facts about medication usage. The long-running study by Harrow, the textbook states, reveals that there are some schizophrenia patients who "are able to function without the benefit of continuous antipsychotic treatment." The authors of that sentence didn't mention the stunning difference in recovery rates for the unmedicated and medicated groups; instead they crafted a sentence that told of the benefit of continuous antipsychotic treatment. In a similar vein, while the textbook briefly discusses the WHO study on the better outcomes of schizophrenia patients in poor countries like India and Nigeria, it does not mention that patients in those countries weren't regularly maintained on antipsychotics. In a section on benzodiazepines, the authors acknowledge that there are concerns about their addictive properties, but then state that long-term outcomes for those who stay on benzodiazepines are generally good, as most patients "maintain their therapeutic gains."
There is a story that psychiatry doesn't dare tell, which shows that our societal delusion about the benefits of psychiatric drugs isn't entirely an innocent one. In order to sell our society on the soundness of this form of care, psychiatry has had to grossly exaggerate the value of its new drugs, silence critics, and keep the story of poor long-term outcomes hidden. That is a willful, conscious process, and the very fact that psychiatry has had to employ such storytelling methods reveals a great deal about the merits of this paradigm of care, much more than a single study ever could. p 312
5
Tallying Up the Profits
"Receiving $750 checks for chatting with some
doctors during a lunch break was such easy money
that it left me giddy."
-PSYCHIATRIST DANIEL CARLAT (2007)'
The walk from Jenna's group home in Montpelier, Vermont, to the town's Main Street is only two blocks long, and yet, on the late spring morning I visited, it took us twenty minutes to travel that distance, for Jenna had to stop every few steps and catch her balance, with her aide, Chris, constantly putting his hand up behind her in case she fell.* Jenna had first taken an antidepressant twelve years earlier, when she was fifteen years old, and now she was on a daily cocktail of eight drugs, including one for drug-induced Parkinsonian symptoms. As we sat outside a cafe, Jenna told me her story, although at times—because of her problems with motor control—it was difficult to understand her. Her tremors are so severe that when she dunked her pastry, the coffee spilled and she had trouble bringing the pastry to her lips.
"I'm s0000000 messed up," she says.
I had gone to the interview thinking that Jenna had been diagnosed with tardive dyskinesia, an antipsychotic side effect that can disable people. But it wasn't clear whether her motor impairments
* Although Jenna said that I could use her last name, her mother and stepfather, who have legal guardianship, requested that I use her first name only.
316 • ANATOMY OF AN EPIDEMIC
A Business Triumph
Jenna's perspective on her care was not an unusual one. Many of the people on SSI and SSDI that I interviewed spoke about how they felt they were caught in the tangles of a business enterprise. "There is a reason we are called consumers" was a comment I heard several times. They are right of course that the pharmaceutical companies want to build a market for their products, and when we view the psychopharmacology "revolution" through this prism, as a business enterprise first and a medical enterprise second, we can easily see why psychiatry and the pharmaceutical companies tell the stories they do, and why the studies detailing poor long-term outcomes have been kept from the public. That information would derail a business enterprise that brings profits to so many.
As we saw earlier, during the late 1970s psychiatry was worried about its survival. The public viewed its therapies as "low in efficacy," and sales of psychiatric drugs were in decline. Then, in what might be called a "rebranding" effort, psychiatry published DSMIII and began telling the public that mental disorders were "real" diseases, just like diabetes and cancer, and that their drugs were chemical antidotes to those diseases, just like "insulin for diabetes." That story, while it may have been false in kind, created a powerful conceptual framework for selling psychiatric medications of all types. Everyone could understand the chemical-imbalance metaphor, and once the public came to understand that notion, it became relatively simple for pharmaceutical companies and their storytelling allies to build markets for psychiatric drugs of various types. They ran "educational" campaigns to make the public more "aware" of the various disorders the drugs were approved to treat, and, at the same time, they expanded the diagnostic boundaries of mental disorders. p 316
After Prozac was introduced, NIMH's DART campaign informed the public that depression regularly went "undiagnosed and untreated." Upjohn partnered with the APA to tell the public that "panic disorder" was a common affliction. In 1990, the NIMH launched its "Decade of the Brain," telling the public that 20
TALLYING UP THE PROFITS • 317
percent of Americans suffered from mental disorders (and thus might be in need of psychiatric medications). Soon psychiatric groups and others were promoting "screening programs," which from a business perspective are best described as customer-recruitment efforts. NAMI, for its part, understood that its "educational" efforts served a commercial end, writing in a 2000 document filed with the government that "providers, health plans, and pharmaceutical companies want to grow their markets and to increase their share of the market. . . . NAMI will cooperate with these entities to grow the market by making persons aware of the issues involving severe brain disorders."2
The APA is in charge of defining diagnostic categories in our society, and DSM-IV, an 886-page tome published in 1994, listed 297 disorders, 32 more than DSM-III. New and expanded diagnoses invite more people into the psychiatric drugstore, and one of the best examples of this type of market-building- occurred in 1998, when GlaxoSmithKline got the FDA to approve Paxil for "social anxiety disorder." In the past, this might have been perceived as a character trait (shyness), but GlaxoSmithKline hired a PR firm, Cohn & Wolfe, to promote awareness of this newly recognized "disease," and soon newspapers and television shows were telling of how SAD afflicted 13 percent of the. American population, making it "the third most common psychiatric disorder in the United States, after depression and alcoholism." Those afflicted with this illness, the public learned, were in some ways biologically "allergic to people."3
Diagnostic changes lay behind the bipolar boom, too. In DSM-III (1980), bipolar illness was identified for the first time (the old manic-depressive cohort was splintered into different groups), and then psychiatry steadily loosened the diagnostic boundaries for this illness, such that today the field talks about bipolar I, bipolar II, and a "bipolarity intermediate between bipolar disorder and normality." This once rare disease is now said to afflict 1 to 2 percent of the adult population, and if the "intermediate" bipolar folk are counted, 6 percent. As this diagnostic expansion happened, pharmaceutical companies and their allies mounted their usual "educational" campaigns. Abbott Laboratories and NAMI teamed up to promote a "Bipolar Awareness Day"; in 2002, Eli Lilly joined with the De-
318 • ANATOMY OF AN EPIDEMIC
pression and Bipolar Support Alliance to launch a new online destination, bipolarawareness.com. Today many websites offer visitors a quick question-and-answer test to see if they have this illness.
Naturally, pharmaceutical-companies want to sell their drugs to people of all ages, and they built the pediatric market for psychotropics step by step. First, in the 1980s, the prescribing of Stimulants to "hyperactive" children took off. Next, in the early 1990s, psychiatrists began regularly prescribing SSRIs to teenagers. But that meant prepubertal children weren't being prescribed these new wonder drugs, and in 1997, the Wall Street Journal reported that the manufacturers of SSRIs were "taking aim at a controversial new market: children." The drug firms were "preparing their medications in easy-to-swallow forms that will be more palatable to even the youngest tykes," the newspaper said, with Eli Lilly formulating a "minty liquid" Prozac for the tots to down.4 The New York Times, in its coverage of this initiative, explained quite clearly what was driving it: "The adult market for [SSRIs] has become saturated. . . . The companies are looking for expanded markets. "5 Psychiatry quickly provided a medical cover for this marketing effort, with the American Academy of Child and Adolescent Psychiatry announcing that S percent of all children in the United States were clinically depressed. "Many of these young patients now are inadequately treated, experts say, often leading to long-term emotional and behavioral problems, drug abuse, or even suicide," the Wall Street Journal reported.6
The creation of the "juvenile bipolar" market was a bit more complicated. Prior to the 1990s, psychiatry thought that bipolar illness simply didn't occur in prepubertal children, or was extremely rare. But children and teenagers prescribed stimulants and anti-depressants often suffered manic episodes, and thus pediatricians and psychiatrists began to see more youth with "bipolar" symptoms. At the same time, once Janssen and Eli Lilly brought their atypical antipsychotics to market, they were looking for a way to sell those drugs to children, and during the mid-1990s, Joseph Biederman at Massachusetts General Hospital in Boston provided the diagnostic framework that made that possible. In 2009, while being deposed in a legal case, he explained his handiwork.
TALLYING UP THE PROFITS • 319
All psychiatric diagnoses, he said, "are subjective in children and
in adults." As such, he and his colleagues decided that children who
in the past had been seen as having pronounced behavioral prob-
lems should instead be diagnosed with juvenile bipolar illness. "The
conditions that we see in front of us are reconceptualized," Biederman testified. "These children have been called in the past conduct disorder, oppositional-defiant disorder. It's not that these children did not exist, they were just under different names."7 Biederman and his colleagues decided that "severe irritability" or "affective storms" would be the telltale signs of juvenile bipolar disorder, and with this new diagnostic criteria in hand, they announced in 1996 that many children diagnosed with ADHD were in fact "bipolar" or else "comorbid" for both illnesses.' The illness was a "much more common condition than was previously thought," often appearing when children were only four or five years old, Biederman said." Soon parents in the United States were reading newspaper articles about this newly recognized illness and buying The Bipolar Child, a book published by Random House in 2000. Child psychiatrists, meanwhile, began treating it with atypical antipsychotics.
That was the marketing machinery that lured more and more Americans into the psychiatric drugstore. As new drugs were brought to market, disease "awareness" campaigns were conducted and diagnostic categories were expanded. Now, once a business gets a customer into its store, it wants to keep that customer and get that customer to buy multiple products, and that's when the psychiatric "drug trap" kicks in.
The "broken brain" story helps with customer retention, of course, for if a person suffers a "chemical imbalance," then it makes sense that he or she will have to take the medication to correct it indefinitely, like "insulin for diabetes." But more important, the drugs create chemical imbalances in the brain, and this helps turn a first-time customer into a long-term user, and often into a buyer of multiple drugs. The patient's brain adapts to the first drug, and that
* During Biederman's February 26, 2009, deposition, an attorney asked him about his rank at Harvard Medical School. "Full professor," he replied. "What's above that?" the attorney asked. "God," Biederman replied.
320 • ANATOMY OF AN EPIDEMIC TALLYING UP THE PROFITS • 321 •
shows how crowded the drugstore has become—one in every eight Americans takes a psychiatric drug on a regular basis."
makes it difficult to go off the medication. The store's exit door is hard to squeeze through, so to speak. At the same time, since psychiatric drugs perturb normal function, they regularly cause physical and psychiatric problems, and this greases the path to polypharmacy. The hyperactive child is put on a stimulant that rouses him during the day; at night he needs a sleeping pill to go to sleep. An atypical causes people to feel depressed and lethargic; psychiatrists may prescribe an antidepressant to treat that problem. Conversely, an antidepressant may stir a bout of mania; in that case an atypical antipsychotic may be prescribed to tamp down the mania. The first drug triggers a need for a second, and so on.
Eli Lilly even capitalized on this fact when it brought Zyprexa to market. As it well knew, Prozac and other SSRIs could trigger manic episodes, and so it instructed its sales representatives to tell psychiatrists that Zyprexa "is a great mood stabilizer, especially for patients whose symptoms were aggravated by an SSRI."10 In essence, Eli Lilly was telling doctors to prescribe its second drug to fix the psychiatric problems caused by its first one. We can also see this cascading effect operating at a societal level. The SSRIs came to market and suddenly bipolar patients were cropping up everywhere, and then this new group of patients provided a market for the atypicals."
All of this has produced a growth industry of impressive dimensions. In 1985, outpatient sales of antidepressants and antipsychotics in the United States amounted to $503 million.11 Twenty-three years later, U.S. sales of antidepressants and antipsychotics reached $24.2 billion, nearly a fiftyfold increase. Antipsychotics—a class of drugs previously seen as extremely problematic in kind, useful only in severely ill patients—were the top revenue-producing class of drugs in 2008, ahead even of the cholesterol-lowering agents.12 Total sales of all psychotropic drugs in 2008 topped $40 billion. Today—and this
* In a similar vein, pharmaceutical companies have pounced on the fact that many of the drugs initially prescribed for a target symptom don't work very well. "Two out of three people treated for depression still have symptoms," a Bristol-Myers Squibb commercial informed television viewers in 2009. The solution? Add an atypical antipsychotic, Abilify, to the mix.
The Money Tree
Naturally, this flourishing business enterprise generates great personal wealth for executives at pharmaceutical companies, and money also flows in fairly copious amounts to the academic psychiatrists who tout their drugs. Indeed, the profits from this enterprise trickle down to nearly all of those who tell the "psychiatric drugs are good" story to our society. To get a sense of the amounts involved, we can look at the money that the different players in this enterprise receive.
We can start with Eli Lilly, as it serves, as a good example of the profits that go to a drug company's shareholders and its executives.
Eli Lilly
In 1987, Eli Lilly's pharmaceutical division generated $2.3 billion in revenues. The company did not have a central nervous system drug of any importance, as its three bestselling drugs were an oral antibiotic, a cardiovascular drug, and an insulin product. Eli Lilly began selling Prozac in 1988, and four years later it became the company's first billion-dollar drug. In 1996, Eli Lilly brought Zyprexa to market, and it became a billion-dollar drug in 1998. By 2000, these two drugs accounted for nearly half of the company's revenues of $10.8 billion.
Prozac soon after lost its patent protection, and thus the wealth-generating effects of the two drugs can best be assessed across a thirteen-year period, from 1987 to 2000. During this time, Eli Lilly's value on Wall Street rose from $10 billion to $90 billion. An investor who bought $10,000 of Eli Lilly stock in 1987 would have seen that investment grow to $96,850 in 2000, and along the way the investor would have received an additional $9,720 in dividends. At the same time, Eli Lilly's executives and employees, in addition
6
Blueprints for Reform
"I think it is time for another hunger strike."
-VINCE BOEHM, 2009
On July 28, 2003, six "psychiatric survivors" associated with MindFreedom International, a patients' rights organization, announced a "fast for freedom." David Oaks, Vince Boehm, and four others sent a letter to the American Psychiatric Association, NAMI, and the U.S. Office of the Surgeon General stating that they would begin a hunger strike unless one of the organizations provided "scientifically valid evidence" that the various stories they told to the public about mental disorders were true. Among other things, the MindFreedom group asked for evidence proving that major mental illness are "biologically-based brain diseases," and for evidence that "any psychiatric drug can correct a chemical imbalance" in the brain. The MindFreedom Six had put together a scientific panel to review the organizations' replies, an advisory group that included Loren Mosher, and they demanded that if the APA and the others couldn't provide such scientific evidence, "you publicly admit to media, government officials, and the general public that you are unable to do so,"1
Here's how the APA responded: "The answers to your questions are widely available in the scientific literature, and have been for years," wrote medical director James Scully. He suggested that they read the U.S. Surgeon General's 1999 Mental Health report, or an
332 • ANATOMY OF AN EPIDEMIC
APA textbook coedited by Nancy Andreasen. "This is a 'user-friendly' textbook for persons just being introduced to the field of psychiatry," he explained.2
Only the uneducated, it seemed, asked such dumb questions. But Scully had failed to list any citations, and so the six "psychiatric survivors" began their hunger strike, and when their scientific advisors reviewed the texts that Scully had referred them to, they found no citations there, either. Instead, the texts all grudgingly acknowledged the same bottom line. "The precise causes [etiology] of mental disorders are not known," U.S. surgeon general Satcher confessed in his 1999 report. MindFreedom's scientific panel, in its August 22 reply to Scully, observed that the strikers had asked "clear questions about the science of psychiatry," and yet the APA had brushed them off. "By not giving specific answers to the specific questions posed by the hunger strikers, you appear to be affirming the very reason for the hunger strike."3
The APA never answered that letter. Instead, after the Mind-Freedom group broke their fast (several started to have health problems), it issued a press release, stating that the APA, NAMI, and the rest of the psychiatric community "will not be distracted by those who would deny that serious mental disorders are real medical conditions that can be diagnosed accurately and treated effectively."4 But it was clear to all observers who had won this battle. The strikers had called the APA's bluff, and the APA had come up empty. It hadn't come up with a single citation that supported the "brain disease" story it told to the public. The MindFreedom Six, along with their scientific panel, then issued a clarion call for help:
We urge members of the public, journalists, advocates, and officials reading this exchange to ask for straightforward answers to our questions from the APA. We also ask Congress to investigate the mass deception that the "diagnosis and treatment of mental disorders," as promoted by bodies such as the APA and its powerful allies, represents in America today.s
The strike, noted MindFreedom executive director David Oaks, stirred articles in the Washington Post and the Los Angeles Times.
BLUEPRINTS FOR REFORM • 333
"The purpose of the strike was to educate the public. It was about empowering the public and getting them to talk about these issues, which affect everyone. It was about challenging the corporate bullying of the [public] mind."6
Lessons from a Hunger Strike
When I first thought about writing a "solutions" chapter, I figured that I would simply report on programs, both in the United States and abroad, that involve using psychiatric medications in a selective, cautious manner (or not at all), and are producing good results. But then I thought of the hunger strike, and I realized that the MindFreedom group had precisely identified the bigger issue at hand.
The real question regarding psychiatric medications is this: When and how should they be. used'? The drugs may alleviate symptoms over the short term, and there are some people who may stabilize well over the long term on them, and so clearly there is a place for the drugs in psychiatry's toolbox. However, a "best" use paradigm of care would require psychiatry, NAMI, and the rest of the psychiatric establishment to think about the medications in a scientifically honest way and to speak honestly about them to the public. Psychiatry would have to acknowledge that the biological causes of mental disorders remain unknown. It would have to admit that the drugs, rather than fix chemical imbalances in the brain, perturb the normal functioning of neurotransmitter pathways. It would have to stop hiding the results of long-term studies that reveal that the medications are worsening long-term outcomes. If psychiatry did that, it could figure out how to use the medications judiciously and wisely, and everyone in our society would understand the need for alternative therapies that don't rely on the medications or at least minimize their use.
In his 1992 book How to Become a Schizophrenic, John Modrow—who had been so diagnosed—wrote the following: "How then are we to help 'schizophrenics'? The answer is simple:
334 • ANATOMY OF AN EPIDEMIC
Stop the lies!"7 In essence, that's what the MindFreedom Six were demanding, and as their advisory panel observed, this is a perfectly rational request. And that, I think, sums up the challenge that we, as a society, now face. How do we break up the psychiatry-and-drugcompany partnership that, as we have seen, regularly does lie to us? How can we insist that our society's mental health system be driven by honest science rather than by a partnership that is constantly seeking to expand the market for psychiatric drugs?
There is no easy answer to that question. But clearly our society needs to have a conversation about it, and so I thought that the rest of this "solutions" chapter should be devoted to interviews and investigations of alternative programs that could help make that conversation a fruitful one.
An Artful Form of Care
David Healy is a professor of psychiatry at Cardiff University and tends to psychiatric patients at the District General Hospital in North Wales, where he has been since 1990. His office is located a few feet from a closed ward, and naturally, he regularly prescribes psychiatric medications. Indeed, although he has come to be perceived by many in psychiatry as a "maverick," he recoils at that word. In the 1980s, he notes, he researched serotonin reuptake in depressed patients. He participated as a clinical investigator in a trial of Paxil. He has authored more than a dozen books and published more than 120 articles, with much of his writing focusing on the history of psychiatry and the psychopharmacology era. His CV speaks of a psychiatrist and historian who, until he began writing about problems with the SSRIs, was embraced by the psychiatric es-tablishment. "I don't think I've changed much at all," he said. "I think the mainstream has left me."8
His thoughts on how psychiatric drugs should be used (and what they really do) have been deeply influenced both by his writings on the history of psychiatry and by a study he has conducted that
BLUEPRINTS FOR REFORM • 335
compares outcomes of the mentally ill in North Wales a century ago with outcomes in the region today. The population hasn't changed in this period, with around 240,000 in the area, and whereas all the seriously mentally were treated at the North Wales Asylum in Denbigh a century ago, today all psychiatric patients needing to be hospitalized are treated at the District General Hospital in Bangor. By poring over records of the two institutions, Healy and his assistants have been able to determine the number of people who were treated back then and the number treated today, as well as the frequency of their hospitalizations.
The common belief, Healy notes, is that the old asylums were bulging with lunatics. Yet from 1894 to 1896, there were only forty-five people per year admitted to the North Wales Asylum (for mental problems). Furthermore, as long as the patients didn't succumb to tuberculosis or some other infectious disease, they regularly got better over the course of three months to a year and went home. Fifty percent were discharged as "recovered" and another 30 percent as "relieved." In addition, the overwhelming majority of patients admitted for a first episode of illness were discharged and never again rehospitalized, and that was true even for psychotic patients. This latter group averaged only 1.23 hospitalizations in a ten-year period (that number includes the initial hospitalization).
Today, the assumption is that patients fare much better than they used to thanks to psychiatric medications. However, in 1996, there were 522 people admitted to the psychiatric ward at the District General Hospital in Bangor—nearly twelve times the number admitted to the Denbigh asylum a century earlier. Seventy-six percent of the 522 patients had been there before, part of a large group of patients in North Wales that cycle regularly through the hospital. Although the patients spent a shorter time in the hospital than they did in 1896, only 36 percent were discharged as recovered. Finally, the patients admitted for a first episode of psychosis in the 1990s averaged 3.96 hospitalizations over the course of ten years—more than three times the number a century earlier. Patients today are clearly more chronically ill than they were a century ago, with modern treatments apparently having set up a "revolving door."9
336 • ANATOMY OF AN EPIDEMIC
"We have been surprised by how poor the five-year outcomes are today," Healy said. "Each time we look at the current data, at the first batch of five-year outcomes [for a particular diagnostic group], we think, 'God, that can't be the case.' "
Their study sends a fairly clear message about how and when psychiatric medications should be used. "A bunch of people used to recover," Healy explained, but if you immediately put all patients on medications, you run the risk of "giving them a chronic problem they wouldn't have had in the old days." Healy now tries to "watch and wait" before giving psychiatric drugs to first-episode patients, as he wants to see if this type of natural recovery can take hold. "I try to use the drugs cautiously in reasonably low doses, and I tell the patient, 'If the drug isn't doing what we want it to do, we are going to halt it,' " he said. If psychiatrists listened to their patients about how the drugs were affecting them, he concluded, "we would have only a few patients on them long-term."
There it is: a simple prescription for using the medications judiciously. Once a physician realizes that many people who experience a bout of psychosis or a deep depression can recover naturally, and that long-term use of psychotropics is associated with increased chronicity, then it becomes apparent that the drugs need to be used in a selective, limited manner. Healy has seen this approach work with his patients, many of whom initially insist that they need the drugs. "I say to them, 'We can do more harm than good,' " he said. "They don't realize just how much harm we can do."
Healing the "In-Between"
For a long time, western Lapland in Finland had one of the highest rates of schizophrenia in Europe. There are about 70,000 people who live there, and during the 1970s and early 1980s, twenty-five or so new cases of schizophrenia appeared each year—an incidence rate double and even triple the norm for other parts of Finland and the rest of Europe. Furthermore, those patients regularly became
BLUEPRINTS FOR REFORM • 337
chronically ill. But today the long-term outcomes of psychotic patients in western Lapland are the best in the Western world, and this region now sees very few new cases of schizophrenia.
This is a medical success that has been decades in the making, and it began in 1969 when Yrjo Alanen, a Finnish psychiatrist who had psychoanalytic training, arrived at the psychiatric hospital in Turku, a port city in southwest Finland. At that time, few psychia-trists in the country thought that psychotherapy could help schizophrenics. However, Alanen believed that the hallucinations and paranoid utterances of schizophrenic patients, when carefully parsed, told meaningful stories. Hospital psychiatrists, nurses, and staff needed to listen to the patients. "It's almost impossible for anyone meeting with these patients' families to not understand that they have difficulties in life," Alanen explained in an interview at the psychiatric hospital in Turku. They are "not ready" to be adults, and "we can help with this development.r10
Over the next fifteen years, Alanen and a handful of other Turku psychiatrists, most notably Jukka Aaltonen and Viljo Rakkolainen, created what they called the "need-adapted" treatment of psychotic patients. Since psychotic patients are a very heterogeneous group, they decided that treatment needed to be "case specific." Some first-episode patients would need to be hospitalized, and others would not. Some would benefit from low doses of psychiatric medications (either benzos or neuroleptics), and others would not. Most important, the Turku psychiatrists settled on group family therapy—of a particularly collaborative type—as the core treatment. Psychiatrists, psychologists, nurses, and others trained in family therapy all served on two- and three-member "psychosis teams," which would meet regularly with the patient and his or her family. Decisions about the patient's treatment were made jointly at those meetings.
In those sessions, the therapists did not worry about getting the patient's psychotic symptoms to abate. Instead, they focused the conversation on the patient's past successes and achievements, with the thought that this would help strengthen his or her "grip on life." The hope, said Rakkolainen, "is that they haven't lost the idea that they can be like others." The patient might also receive individual
338 • ANATOMY OF AN EPIDEMIC
psychotherapy to help this process along, and eventually the patient would be encouraged to construct a new "self-narrative" for going forward, the patient imagining a future where he or she was integrated into society, rather than isolated from it. "With the biological conception of psychosis, you can't see the past achievements" or the future possibilities, Aaltonen said.
During the 1970s and 1980s, the outcomes for psychotic patients in the Turku system steadily improved. Many chronic patients were discharged from the hospital, and a study of first-episode schizophrenic-type patients treated from 1983 to 1984 found that 61 percent were asymptomatic at the end of five years and only 18 percent were on disability. This was a very good result, and from 1981 to 1987, Alanen coordinated the Finnish National Schizophrenia Project, which determined that the need-adapted model of care developed in Turku could be successfully introduced into other cities. Two decades after Alanen and the others had initiated their Turku project, Finland had decided that psychotherapy could indeed help psychotic patients.
However, the question of the best use of antipsychotics remained, and in 1992, Finland mounted a study of first-episode patients to answer it. All six sites in the study provided the newly diagnosed patients with need-adapted treatment, but in three of the centers, the patients were not put on antipsychotics during the first three weeks (benzos could be used), with drug therapy initiated only if the patient hadn't improved during this period. At the end of two years, 43 percent of the patients from the three "experimental" sites had never been exposed to neuroleptics, and overall outcomes at the experimental sites were "somewhat better" than they were at the centers where nearly all of the patients had been exposed to the drugs. Furthermore, among the patients at the three experimental sites, those who had never been exposed to neuroleptics had the best outcomes.11
"I would advise case-specific use [of the drugs]," Itakkolainen said. "Try without antipsychotics. You can treat them better without medication. They become more interactive. They become themselves." Added Aaltonen: "If you can postpone medication, that's important."
BLUEPRINTS FOR REFORM • 339
It might seem that Finnish psychiatry, given the outcomes of the study, would have then embraced—on a national level—this "no immediate use of neuroleptics" model of care. Instead, Alanen and the other creators of need-adapted treatment retired, and during the 1990s, Finland's treatment of psychosis became much more "biologically" oriented. Even in Turku, first-episode patients are regularly treated with antipsychotics today, and Finnish guidelines now call for the patients to be kept on the drugs for at least five years after a first episode. "I am a bit disappointed," Alanen confessed at the end of our interview.
Fortunately, one of the three "experimental" sites in the 19921993 study did take the results to heart. And that site was Tornio, in western Lapland.
On my way north to Tornio, I stopped to interview Jaakko Seikkula, a professor of psychotherapy at the University of Jyvaskyla. In addition to working at Keropudas Hospital in Tornio for nearly twenty years, he has been the lead author on several studies documenting the extraordinary outcomes of psychotic patients in western Lapland.
The transformation of care at Keropudas Hospital, from a system in which patients were regularly hospitalized and medicated to one in which patients are infrequently hospitalized and only occasionally medicated, began in 1984, when Rakkolainen visited and spoke about need-adapted treatment. The Keropudas staff, Seikkula recalled, immediately sensed that holding "open meetings," where every participant freely, shared his or her thoughts, would provide psychotic patients with a very different experience from conven-tional psychotherapy. "The language we use when the patient is sitting with us is so different from the language we use when we [therapists] are by ourselves and discussing the patient," he said. "We do not use the same words, and we have to listen more to the patient's ideas about what is going on, and listen more to the family."
Eventually, Seikkula and others in Tornio developed what they called open-dialogue therapy, which was a subtle variation of
340 • ANATOMY OF AN EPIDEMIC
Turku's need-adapted model. As was the case in Turku, patient outcomes in western Lapland improved during the 1980s, and then Tornio was selected to be one of the three experimental sites in Finland's 1992-93 first-episode study. Tornio enrolled thirty-four patients, and at the end of two years, twenty-five had never been exposed to neuroleptics. Nearly all of the never-medicated patients in the national study (twenty-five of twenty-nine) had actually come from this one site, and thus it was only here that hospital staff observed the longer-term course of unmedicated psychosis. And they found that while recovery from psychosis often proceeds at a fairly slow pace, it regularly happens. The patients, Seikkula said, "went back to their work, to their studies, to their families."12
Encouraged by the results, Keropudas Hospital immediately started a new study, charting the long-term outcomes of all first-episode psychotic patients in western Lapland from 1992 through 1997. At the end of five years, 79 percent of the patients were asymptomatic and 80 percent were working, in school, or looking for work. Only 20 percent were on government disability. Two-thirds
Five-Year Outcomes for First-Episode Psychotic Patients in Finnish Western Lapland Treated with Open-Dialogue Therapy
Patients (N=75)
Schizophrenia (N=30)
Other psychotic disorders (N=45)
Antipsychotic use
Never exposed to antipsychotics Occasional use during five years Ongoing use at end of five years 67%
33%
20%
Psychotic symptoms
Never relapsed during five years Asymptomatic at five-year follow-up 67%
79%
Functional outcomes at five years
Working or in school
Unemployed On disability 73% 7% 20%
Source: Seikkula, J. "Five-year experience of first-episode nonaffective psychosis in open-dialogue approach:' Psychotherapy Research 16 (2006): 214-28.
BLUEPRINTS FOR REFORM • 341
of the patients had never been exposed to antipsychotic medication, and only 20 percent took the drugs regularly." Western Lapland had discovered a successful formula for helping psychotic patients recover, with its policy of no immediate use of neuroleptics in first-episode patients critical to that success, as it provided an "escape valve" for those who could recover naturally.
"I am confident of this idea," Seikkula said. "There are patients who may be living in a quite peculiar way, and they may have psychotic ideas, but they still can hang on to an active life. But if they are medicated, because of the sedative action of the drugs, they lose this 'grip on life,' and that is so important. They become passive, and they no longer take care of themselves."
Today, the psychiatric facilities in western Lapland consist of the fifty-five-bed Keropudas Hospital, which is located on the outskirts of Tornio, and five mental-health outpatient clinics. There are around one hundred mental-health professionals in the district (psychiatrists, psychologists, nurses, and social workers), and most have completed a nine-hundred-hour, three-year course in family therapy. Many of the staff—including psychiatrist Birgitta Alakare and psychologists Tapio Salo and Kauko Haarakangas—have been there for decades, and today open-dialogue therapy is a well-polished form of care.
Their conception of psychosis is quite distinct in kind, as it doesn't really fit into either the biological or psychological category. Instead, they believe that psychosis arises from severely frayed social relationships. "Psychosis does not live in the head. It lives in the in-between of family members, and the in-between of people," Salo explained. "It is in the relationship, and the one who is psychotic makes the bad condition visible. He or she 'wears the symptoms' and has the burden to carry them."14
With most of the staff in the district trained in family therapy, the system is able to respond quickly to a psychotic crisis. Whoever is first contacted—by a parent, a patient seeking help, or perhaps a school administrator—is responsible for organizing a meeting within twenty-four hours, with the family and patient deciding where the meeting should be held. The patient's home is the preferred place. There must be at least two staff members present at the meeting, and preferably three, and this becomes a "team" that ideally will stay together during the patient's treatment. Everyone goes to that first meeting aware that they "know nothing," said nurse Mia Kurtti. Their job is to promote an "open dialogue" in which everybody's thoughts can become known, with the family members (and friends) viewed as coworkers. "We are specialists in saying that we are not specialists," Birgitta Alakare said.
The therapists consider themselves guests in the patient's home, and if an agitated patient runs off to his or her room, they simply ask the patient to leave the door open, so that he or she can listen to the conversation. "They hear voices; we meet them, and we try to reassure them," Salo said. "They are psychotic, but they are not violent at all." Indeed, most patients want to tell their story, and when they speak of hallucinations and paranoid thoughts, the therapists simply listen and reflect upon what they've heard. "I think [psychotic symptoms] are very interesting," Kurtti said. "What's the difference between voices and thoughts? We are having a conversation."
No mention is made of antipsychotics in the first few meetings. If the patient begins sleeping better and bathing regularly, and in other ways begins to reestablish societal connections, the therapists know that the patient's "grip on life" is strengthening, and that medication will not be needed. Now and then, Alakare may prescribe a benzodiazepine to help a person sleep or to dampen the patient's anxiety, and eventually she may prescribe a neuroleptic at a low dose. "Usually I suggest that the patient use it for some months," Alakare said. "But when the problems go away, after six months or a year, or maybe even after three years, we try to stop the medication."
From the outset, the therapists strive to give both the patient and family a sense of hope. "The message that we give is that we can manage this crisis. We have experience that people can get better, and we have trust in this kind of possibility," Alakare said. They have found that it can take a long time—two, three, or even five years—for a patient to recover. Although a patient's psychotic
BLUEPRINTS FOR REFORM • 343
symptoms may abate fairly quickly, they are focused on the patient's "grip on life" and repairing his or her relationship to society, and that is a much bigger task. The team continues to meet with the patient and family, and as this process unfolds, teachers and prospective employers are asked to attend too. "It's about restoring social connections," Salo said. "The 'in-between' starts working again, with family and with friends."
Over the past seventeen years, open-dialogue therapy has transformed "the picture of the psychotic population" in western Lapland. Since the 1992-93 study, not a single first-episode psychotic patient has ended up chronically hospitalized. Spending on psychiatric services in the region dropped 33 percent from the 1980s to the 1990s, and today the district's per-capita spending on mental-health services is the lowest among all health districts in Finland. Recovery rates have stayed high: From 2002 to 2006, Tornio par-ticipated in a multinational study by Nordic countries of first-episode psychosis, and at the end of two years, 84 percent of the patients had returned to work or school, and only 20 percent were taking antipsychotics. Most remarkable of all, schizophrenia is now disappearing from the region. Families in western Lapland have become so comfortable with this gentle form of care that they call the hospital (or one of the outpatient clinics) at the first sign of psychosis' in a loved one, with the result being that today first-episode patients typically have had psychotic symptoms for less than a month and, with treatment initiated at this early stage, very few go on to develop schizophrenia (the diagnosis is made after a patient has been psychotic for longer than six months). Only two or three new cases of schizophrenia appear each year in western Lapland, a 90 percent drOp since the early 1980s.15
Tornio's success has drawn the attention of mental-health-care providers in other European countries, and during the past twenty years, two or three other groups in Europe have reported that the combination of psychosocial care and limited use of neuroleptics has produced good outcomes.16 "This really happened," Seikkula said. "It's not just a theory."
344 • ANATOMY OF AN EPIDEMIC
On my way back to Helsinki, I kept puzzling over this one thought: Why are the group meetings in Tornio so therapeutic? Given the outcomes literature for neuroleptics, I could understand why selective use of the drugs had proven to be so helpful. But why did open-dialogue therapy help psychotic patients heal?
During my two days in Tornio, I sat in on three group sessions, and although I don't speak Finnish, it was nevertheless possible to gain a sense of the meetings' emotional tenor and to observe how the conversation flowed. Everyone sat in a circle, in a very relaxed and calm manner, and-before anyone spoke, there often was a split-second moment of silence, as if whoever was going to speak next was gathering his or her thoughts. Now and then someone laughed, and I couldn't identify a time when anyone was interrupted, and yet no individual seemed to -go on speaking too long, either. The conversation seemed graced by gentility and humility, and both family members and patients listened with rapt attention whenever the therapists turned and spoke to each other. "We like to know what they really think, rather than just have them give us advice," said the parents in one of the meetings.
But that was the sum of it. It was all a bit mystifying, and even the staff at Keropudas Hospital hadn't really been able to explain why these conversations were so therapeutic. "The severe symptoms begin to pass," Salo said with a shrug. "We don't know how it happens, but [open-dialogue therapy] must be doing something, because it works."
A Natural Antidepressant
In the early 1800s, Americans regularly turned to a book written by Scottish physician William Buchan for medical advice. In Domestic Medicine, Buchan prescribed this pithy remedy for melancholy:
“The patient ought to take as much exercise in the open air as he can bear ... A plan of this kind, with a strict attention to diet, is a much more rational method of cure, than confining the patient within doors, and plying him with medicines. fn 17
Two centuries later, British medical authorities rediscovered the wisdom of Buchan's advice. In 2004, the National Institute for Health and Clinical Excellence, which acts as an advisory panel to the country's National Health Service, decided that "antidepressants are not recommended for the initial treament of mild depression, because the risk-benefit ratio is poor." Instead, physicians should try non-drug alternatives and advise "patients of all ages with mild depression of the benefits of following a structured and supervised exercise programme."18
Today, general practitioners in the UK may write a prescription for exercise. "The evidence base for exercise as a treatment for depression is quite good," said Andrew McCulloch, executive director of the Mental Health Foundation, a London-based charity that has been promoting this alternative. "It also reduces anxiety. It's good for self-esteem, control of obesity, et cetera. It has a broad-spectrum effect." fn 19
In terms of its short-term efficacy as an antidepressant, studies have shown that exercise produces a "substantial improvement" within six weeks, that its effect size is "large,' and that 70 percent of all depressed patients respond to an exercise program. "These success rates are quite remarkable," German investigators wrote in 2008.20 In addition, over time, exercise produces a multitude of "side benefits." It enhances cardiovascular function, increases muscle strength, lowers blood pressure, and improves cognitive function. People sleep better, they function better sexually, and they also tend to become more socially engaged.
A 2000 study by James Blumenthal at Duke University also revealed that it is unwise to combine exercise with drug therapy. He randomized 156 older depressed patients into three groups—exercise, Zoloft, and Zoloft plus exercise—and at the end of sixteen weeks, those treated with exercise alone were doing as well as those in the other two groups.21 Blumenthal then tracked the patients for another six months, with the patients free to choose whatever
346 • ANATOMY OF AN EPIDEMIC
The Long-Term Benefit of Exercise for Depression
Treatment During
First Four Months Percentage of Patients in Remission at End of Four Months Percentage of Remitted Patients Who Relapsed in Six-Month Follow-up Percentage of Patients Depressed at End ofTen
Months
Zoloft alone 69% 38% 52%
Zoloft plus exercise therapy 66% 31% 55%
Exercise therapy alone 60% 8% 30%
In this study by Duke researchers, older patients with depression were treated for 16 weeks in one of three ways, and then followed for another six months. Patients treated with exercise alone had the lowest rates of relapse during the following six months, and as a group, they were much less likely to be suffering from depressive symptoms at the end of ten months. Source: Babyak, M. "Exercise treatment for major depression "Psychosomatic Medicine 62 (2000): 633-38. 100-11.
treatment they wanted during this period, and at the end the patients treated initially with exercise alone were doing the best. Only 8 percent of those who had been well at the end of sixteen weeks had relapsed during the follow-up, and by the end of ten months 70 percent of the exercise-only group were asymptomatic. In the two Zoloft-exposed groups, more than 30 percent of the patients who had been well at the end of sixteen weeks relapsed, and fewer than 50 percent were asymptomatic by the study's end. The "Zoloft plus exercise" group had fared no better than the "Zoloft alone" patients, which suggested that exposure to Zoloft negated the benefits of exercise. "This was an unexpected finding, because it was assumed that combining exercise with medication would have, if anything, an additive effect," Blumenthal wrote.22
In 2003, when Britain's Mental Health Foundation launched its exercise-for-depression campaign, it took advantage of the fact that general practitioners in Britain were already "prescribing" exercise to patients with diabetes, hypertension, osteoporosis, and other physical conditions. The delivery of this medical care requires physicians to collaborate with local YMCAs, gyms, and recreational facilities, with these collaborations known as "exercise-referral schemes," and thus the foundation simply needed to get the GPs to start prescribing exercise to their depressed patients too.
BLUEPRINTS FOR REFORM • 347
Today, more than 20 percent of the GPs in the UK prescribe exercise to depressed patients with some frequency, which is four times the percentage who did in 2004.
A "prescription" for exercise typically provides the patient with twenty-four weeks of treatment. An exercise professional assesses the patient's fitness and develops an appropriate "activity plan," with the patient then given discounted or free access to the collaborating YMCA or gym. Patients work out on exercise machines, swim, and take various exercise classes. In addition, many exercise-referral schemes provide access to "green gyms." The outdoor pro-
may
grams ay involve group walks, outdoor stretching classes, and volunteer environmental work (managing local woodlands, improving footpaths, creating community gardens, etc.). Throughout the six months of treatment, the exercise professional monitors the patient's health and progress.
As might be expected, patients have found "exercise-onprescription" treatment to be quite helpful. They told the Mental Health Foundation that exercise allowed them to "take control of their recovery" and to stop thinking of themselves as "victims" of a disease. Their confidence and self-esteem increased; they felt calmer and more energetic. Treatment was now focused on their "health," rather than on their "illness."
"The fathers of medicine wouldn't be surprised about what we are doing," McCulloch said. "They would say, 'Hasn't science gone any further? Diet and exercise? This is what is new?' If they could travel in a time machine, they would think we were mad, because people have been saying these things for thousands of years."
These Kids Are Awesome
The children who end up living at Seneca Center. in San Leandro, California, have come to the last stop for severely disturbed youth in the northern part of the state. The children, five to thirteen years old, have usually cycled through several foster homes and have had multiple hospitalizations, and their behavior has been so difficult
348 • ANATOMY OF AN EPIDEMIC
that there are no foster homes or hospitals left that want to see them again. In bureaucratic terms, they are "level-14" kids, which is the designation given to the most troubled kids in California, but since these children have flunked out of other level-14 facilities, they are better described as "level-14-plus-plus" youth. Counties pay Seneca Center $15,000 a month to shelter a child and, not surprisingly, when the children arrive at the center, most are on heavy-duty drug cocktails. "They are so drugged up that they are asleep most of the day," said Kim Wayne, director of the residence program.23
And then their lives begin to change dramatically.
I visited one of Seneca Center's two residences for younger children in the summer of 2009, and when I entered, here is what I saw: a young African American girl wearing headphones singing along to a Jordin Sparks song; a second slightly older African American girl sitting at the kitchen table, leafing through photos of their recent group trip to Disneyland; and two African American boys at the table goofing around with each other and racing to see who could drink a glass of water the fastest. A Caucasian girl sat on the couch, and the sixth resident of the house, I later learned, was off at a swimming lesson. Within a short while, the girl with the headphones was singing a cappella (and quite well), and the girl huddled over the photo album had started calling me Bob Marley, apparently because I knew who Jordin Sparks was. Now and then, one of the children erupted into laughter.
"The kids are so grateful to be off the drugs," said therapist Kari Sundstrom. "Their personalities come back. They are people again."
The two Seneca Center homes may be the last residential facilities in the United States where severely troubled children under county or state control are treated without psychiatric drugs. Indeed, M most child-psychiatry circles, this would be considered unethical. "I've been told, 'If your child had a disease, would you deny your child medication that helped him get better?' " said Seneca Center founder and CEO Ken Berrick. And even within the agency, which has a staff of around seven hundred and provides a variety of services to two thousand troubled children and youth in northern California, the residence program is an anomaly.
When the center opened in 1985, Berrick and others sought to
BLUEPRINTS FOR REFORM • 349
hire consulting psychiatrists who would use psychiatric medications in a "conservative" fashion and never for purposes of "behavioral control." Some used the drugs more than others, and then there was Tony Stanton, whom the agency hired in 1987 to oversee the children's residential program. In the 1960s, he had trained at Langley Porter Hospital in San Francisco, which at the time emphasized the "importance of environment" to a child's mental health. Stanton's own "attachment theory" convinced him of the importance of emotional relationships to a child's well-being. Then, in the late 1970s, while he was in charge of a psychiatric ward for children at a county hospital, he assigned a "mentor" to every child. The children weren't medicated, and he saw a number of them become at-tached to their mentors and "blossom."
"That experience allowed me to see this therapeutic principle in action," Stanton said. "You just can't organize yourself without a connection to another human being, and you can't make that connection if you embalm yourself with drugs."
When a child enters Seneca Center's residential program, Stanton does not ask "what's wrong" with the child, but rather "what happened to them." He gets the department of social services, schools, and other agencies to send him all of the records they have on the child, and then he spends eight to ten hours constructing a "life chart." As might be expected, the charts regularly tell of children who have been sexually abused, physically abused, and horribly neglected. p 349
But Stanton also tracks their medication history and how their behavior may have changed after they were put on a particular drug, and given that the children who arrive at Seneca Center are seriously disturbed, these medical histories regularly tell of psychiatric care that has worsened their behavior. "I'll have people say, 'We want to try the child on Risperdal now,' and I'll say, 'Let's take a look at the chart and see what happened before. I don't think it will be helpful,' " Stanton said.
The children regularly arrive at the center on drug cocktails, and thus it can take a month or two to withdraw the medications. Often the children, having been repeatedly told that they need the drugs, are nervous about this process—"One kid told me 'What do you mean you are taking me off my meds? I'll destroy your program,' "
35o • ANATOMY OF AN EPIDEMIC
Stanton said—and often they do become more aggressive for a time. Staff may have to use "physical restraints" more frequently (they have been trained to hold the kids in "safe" ways). However, these behavioral problems usually begin to abate and by the end of the withdrawal process, the child has "come alive."
"It's wonderful," Kim Wayne said. "Most times when the kids come in, they can't keep their heads up, they are lethargic, they are just a blank and there is minimal engagement. You just can't get through to them. But when they come off their meds, you can engage them and you get to see who they are. You get a sense of their personality, their sense of humor, and what kinds of things they like to do. You may have to use physical restraints for a time, but to me, it's worth it."
Once they are off meds, the children begin to think of themselves in a new way. They see that they can control their own behavior, and this gives them a sense of "agency," Stanton said. The Seneca Center uses behavior-modification techniques to promote this self-control, with the children constantly having to abide by a well-defined set of rules. They have to ask permission to go to the bathroom and enter bedrooms, and if they don't comply with the rules, they may be sent to a "time-out" or lose a privilege. But the staff tries to focus on reinforcing positive behaviors, offering words of praise and rewarding the kids in various ways. The children are required to keep their rooms clean and perform a daily chore, and at times they will help prepare the evening meal.
"The question of feeling in charge of yourself and being responsible for yourself is the central issue in their lives," Stanton said. "They may only partially get there while they are with us, but when we are really successful, we see them develop this sense of 'Oh, I can do this; I want to be in control of myself and my own life.' They see themselves as having that power."
Even more important, once the children are off the medications they are better able to form emotional bonds with the staff, and the staff with them. They have known rejection all their lives, and they need to form relationships that nurture a belief that they are worthy of being loved, and when that happens, their "internal narrative" can switch from "I'm a bad kid" to "I'm a good kid."
BLUEPRINTS FOR REFORM • 351
"They come in thinking, 'I'm crazy, you are going to hate me, you are going to get rid of me, I'm going to be the worst kid you have ever seen," said therapist Julie Kim. "But then they become willing to form [emotional] attachments, and that's such an amazing thing. You can see the power of a relationship to change a kid, and even the kids who seem the toughest when they come in here, who don't make any progress at first, eventually do."
Although Kim and others can tell anecdotal stories of children discharged from the residence program who have returned to ordinary schools and done well, the center has not done a long-term follow-up of the children that have gone through their residence program. The only statistical information the center has to show that its residence program works is this: 225 children lived at its residences from 1995 to 2006, and nearly all were discharged to lower-level group homes or to a foster home or to their biological families. Their time at Seneca Center at least turned their lives in a new direction. And yet, it is difficult to be optimistic that their lives continue down that path. Their emotional and behavioral problems do not completely go away, and so many of the discharged children—and perhaps most—are remedicated. They return to a world where that is the norm. Their time at Seneca Center may primarily provide them with a temporary oasis from a society prone to asking "what's wrong with them," and thus, if we want to assess whether the no-medication policy of the center's residence program is providing the children with a "benefit," instead of looking to the future, perhaps we should focus on the present and look at what it is like for the children to have this opportunity to "come alive" for a time and fully feel the world.
I spent two days at the center, and there were three children in particular I had a chance to interact with. One was a twelve-year-old boy I'll call Steve. When he'd arrived at Seneca Center a year earlier, he'd been so filled with suicidal and self-destructive habits that doctors thought he had suffered brain damage from all of his head-banging episodes. Since then he'd become very attached to Stacy, one of the male staff at his house, and during our interview, he flopped down into a chair, grinned, and immediately took over the conversation. "I hate taking medicine. It is real boring being on
356 • ANATOMY OF AN EPIDEMIC
that it's not necessarily good for the person and potentially very harmful, they would tend to honor a person's legal right to refuse treatment. In the same vein, if the public knew that there are other non-drug approaches like Soteria that work better, they would support alternatives, right?"
State case laws governing the forced treatment of psychiatric patients date back to the late 1970s. Although state supreme courts typically ruled that patients have a right to refuse treatment (in non-emergency situations), they nevertheless noted that antipsychotics were understood to be "a medically sound treatment of mental disease," and thus hospitals could apply to a court to sanction forced treatment. At such hearings, hospitals regularly argue that no competent person would refuse "medically sound treatment," and thus courts consistently order patients to be medicated.27 But in 2003, Gottstein initiated a forced-drugging lawsuit on behalf of a woman named Faith Myers, and he put the medication on trial, arguing that the state could not show that it was in her best medical interest to take an antipsychotic. He got Loren Mosher and a second psychiatrist who knows the outcomes literature well, Grace Jackson, to serve as his expert witnesses, and he also filed copies of the many research studies that tell of how neuroleptics can worsen long-term outcomes.
Having become versed in the scientific literature, the Alaska Supreme Court gave PsychRights a stunning legal victory in 2006. "Psychotropic medication can have profound and lasting negative effects on a patient's mind and body," the court wrote. These drugs "are known to cause a number of potentially devastating side effects." As such, it ruled in Myers v. Alaska Psychiatric Institute that a psychiatric patient could be forcibly medicated only if a court "expressly finds by clear and convincing evidence that the proposed treatment is in the patient's best interest and that no less intrusive alternative is available." fn 28 In Alaska case law, antipsychotics are no longer viewed as treatment that will necessarily help psychotic people.
In 2004, Gottstein launched an effort to get the Mental Health Trust Authority to fund a Soteria home in Anchorage, which would offer psychotic patients the type of care that Loren Mosher's Soteria
BLUEPRINTS FOR REFORM • 357
Project did in the 1970s. Once again, he relied on the persuasive powers of the scientific literature to carry his argument, and in the summer of 2009, a seven-bedroom Soteria home opened a few miles south of downtown. The director of the project, Susan Musante, formerly led a psychiatric rehabilitation program at the University of New Mexico Mental Health Center; the consulting psychiatrist, Aron Wolf, is a well-respected figure in Alaskan psychiatry.
"We want to work with younger people who have been on psychiatric medications for only a short time, and by getting them off the meds and helping them get better, we hope to keep them from going down the path of chronic illness," Musante said. "Our expec-tation is that people will recover. We expect them to go to work or to school, to return to age-appropriate behavior. We are here to help them to dream again and to pursue those dreams. We are not set up to funnel them onto SSI or SSDI."29
Gottstein now has his sights set on a legal challenge national in scope. He has been filing lawsuits that challenge the medicating of foster children and poor children in Alaska (the poor are covered by Medicaid), and ultimately he hopes to take one of these cases to the U.S. Supreme Court. He sees this as a 14th Amendment issue, with the children being deprived of their liberty without due process of law. At the heart of any such case would be a scientific question: Are the foster children being treated with medications that help, or are they being treated with tranquilizing drugs that cause long-term harm?
"I analogize it to Brown v. Board of Education," Gottstein said. "Before that decision, there was widespread acceptance in the United States that segregation is OK. The Supreme Court had previously said that segregation was OK. But then in Brown v. Board of Education, the court said it wasn't OK, and that really changed public opinion. Today you can't get anyone to say segregation is OK. And that's how I visualize this whole effort."
Epilogue
"Few dare to announce unwelcome truth."
-EDWIN PERCY WHIPPLE (1866)1
This book tells a history of science that leads readers to a socially awkward place. Our society believes that psychiatric medications have led to a "revolutionary" advance in the treatment of mental disorders, and yet these pages tell of a drug-induced epidemic of dis-abling mental illness. Society sees the beautiful woman, and this book directs the reader's gaze to the old woman.
It's never easy to hold a belief that is out of sync with what the rest of society believes, and in this instance, it's particularly difficult because the story of progress is told by figures of scientific authority—the APA, the NIMH, and psychiatrists at prestigious universities such as Harvard Medical School. Disagree with the common wisdom on this topic, and it seems that you must be a card-carrying member of the flat-Earth society. p 361
But for those readers still wondering about the history told here, I offer one last story. You can read it and decide for yourself whether you are now, metaphorically speaking, in the flat-Earth camp.
After I interviewed Jaakko Seikkula at the University of Jyvaskyla, he asked me to give a short talk on the history of antipsychotics to a few of his colleagues. Now, Seikkula and others at Keropudas Hospital in Tornio did not decide to use antipsychotics
362 • ANATOMY OF AN EPIDEMIC
in a selective manner because they thought that the drugs worsened psychotic symptoms over the long term. Instead, they observed that many people did better when off them. Thus, when I spoke to Seikkula's colleagues at the University of Jyvaskyla, this notion that antipsychotics can make people chronically ill was something they hadn't thought much about before, and at the end of my talk, one of the members of our circle asked if this could be true of antidepressants, too. He and others had been researching the long-term outcomes of depressed patients in Finland, and charting too whether they had used the drugs, and they had been startled by their results.
So, dear readers, ask yourself this: What do you think they found? And are you surprised?
NOTES
To read many of the source documents listed here, go to madinamerica.com or robertwhitaker.org
Chapter 1: A Modern Plague
1. J. Bronowski, The Ascent of Man (New York: Little, Brown & Co., 1973), 153.
2. IMS Health, "2007 top therapeutic classes by U.S. sales."
3. U.S. Department of Health and Human Services, Mental Health: A Report of the Surgeon General (1999), 3, 68, 78.
4. E. Shorter, A History of Psychiatry (New York: John Wiley & Sons, 1997), 255.
5. R. Friedman, "On the Horizon, Personalized Depression Drugs," New York Times, June 19, 2007.
6. Boston Globe editorial, "When Kids Need Meds," June 22, 2007.
7. Address by Carolyn Robinowitz, APA Annual Conference, Washington, D.C., May 4, 2008.
8. C. Silverman, The Epidemiology of Depression (Baltimore: Johns Hopkins Press, 1968), 139.
9. Social Security Administration, annual statistical reports on the SSDI and SSI pro-grams, 1987-2008. To calculate a total disability number for 1987 and 2007, I added the number of recipients under age sixty-five receiving an SSI payment that year and the number receiving an SSDI payment due to mental illness, and then I adjusted the total to reflect the fact that one in every six SSDI recipients also receives an SSI payment. Thus, mathematically speaking: SSI recipients + (.833 x SSDI recipients) = total number of disabled mentally ill.
10. Silverman, The Epidemiology of Depression, 139.
11. The annual Social Security Administration reports don't provide data on the specific
364 • NOTES
diagnoses of SSI and SSDI recipients disabled by mental illness. However, various re-searchers have reported that affective disorders now make up 37 percent (or more) of the disabled mentally ill. See, for instance, J. Cook, "Results of a multi-site clinical trials study of employment models for mental health consumers," available at: psych.uic.eduJEIDP/eidp-3-20-03.pdf.
12. U.S. Government Accountability Office, "Young adults with serious mental illness" (June 2008).
13. Social Security Administration, annual statistical reports on the SSI program, 19962008; and Social Security Bulletin, Annual Statistical Supplement, 1988-1992.
Chapter 2: Anecdotal Thoughts
1. Adlai Stevenson, speech at University of Wisconsin, October 8, 1952. As cited by L. Frank, Quotationary (New York: Random House, 2001), 430.
Chapter 3: The Roots of an Epidemic
1. J. Young, The Medical Messiahs (Princeton, NJ: Princeton University Press, 1967), 281.
2. Chemical Heritage Foundation, "Paul Ehrlich, Pharmaceutical Achiever," accessed at chemheritage.org.
3. P. de Kruif, Dr. Ehrlich's Magic Bullet (New York: Pocket Books, 1940), 387.
4. L. Sutherland, Magic Bullets (Boston: Little, Brown and Company, 1956), 127.
5. L. Garrett, The Coming Plague (New York: Penguin, 1995), 49.
6. T. Mahoney, The Merchants of Life (New York: Harper & Brothers, 1959), 14.
7. "Mind Is Mapped in Cure of Insane," New York Times, May 15, 1937.
8. "Surgery Used on the Soul-Sick," New York Times, June 7, 1937.
9. A. Deutsch, The Shame of the States (New York: Harcourt Brace, 1948), 41.
10. E. Torrey, The Invisible Plague (New Brunswick, NJ: Rutgers University Press, 2001), 295.
11. G. Grob, The Mad Among Us (Cambridge, MA: Harvard University Press, 1994), 189.
12. "Need for Public Education on Psychiatry Is Stressed," New York Times, November 16, 1947.
Chapter 4: Psychiatry's Magic Bullets
1. E. Valenstein, Blaming the Brain (New York: The Free Press, 1998), 38.
2. J. Swazey, Chlorpromazine in Psychiatry (Cambridge, MA: MIT Press, 1974), 78.
3. Ibid, 79.
4. Ibid, 105.
S. Ibid, 134-35.
6. F. Ayd Jr., Discoveries in Biological Psychiatry (Philadelphia: Lippincott, 1970), 160.
7. Symposium proceedings, Chlorpromazine and Mental Health (Philadelphia: Lea and Fabiger, 1955), 132.
8. Ayd, Discoveries in Biological Psychiatry, 121.
9. M. Smith, Small Comfort (New York: Praeger, 1985), 23. NOTES • 365
10. Ibid, 26.
11. Ibid, 72.
12. "TB and Hope," Time, March 3, 1952.
13. Valenstein, Blaming the Brain, 38.
14. "TB Drug Is Tried in Mental Cases," New York Times, April 7, 1957.
15. M. Mintz, The Therapeutic Nightmare (Boston: Houghton Mifflin, 1965), 166.
16. Ibid, 488.
17. Ibid, 481.
18. Ibid, 59, 62.
19. T. Mahoney, The Merchants of Life (New York: Harper & Brothers, 1959), 4, 16.
20. Mintz, The Therapeutic Nightmare, 83.
21. Swazey, Chlorpromazine in Psychiatry, 190.
22. "Wonder Drug of 1954?" Time, June 14, 1954.
23. "Pills for the Mind," Time, March 7, 1955.
24. "Wonder Drugs: New Cures for Mental Ills?" U.S. News and World Report, June 17, 1955.
25. "Pills for the Mind," Time, March 7, 1955.
26. "Don't-Give-a-Damn Pills," Time, February 27, 1956.
27. Smith, Small Comfort, 67-69.
28. "To Nirvana with Miltown," Time, July 7, 1958.
29. "Wonder Drug of 1954?" Time, June 14, 1954.
30. "TB Drug Is Tried in Mental Cases," New York Times, April 7, 1957.
31. Smith, Small Comfort, 70.
32. "Science Notes: Mental Drug Shows Promise," New York Times, April 7, 1957.
33. "Drugs and Depression," New York Times, September 6, 1959.
34. H. Himwich, "Psychopharmacologic drugs," Science 127 (1958): 59-72.
35. Smith, Small Comfort, 110.
36. Ibid, 104.
37. The NIMH Psychopharmacology Service Center Collaborative Study Group, "Phe-nothiazine treatment in acute schizophrenia," Archives of General Psychiatry 10 (1964): 246-61.
38. Valenstein, Blaming the Brain, 70-79. Also see David Healy, The Creation of Psychopharmacology (Cambridge, MA: Harvard University Press, 2002), 106, 205206.
39. J. Schildkraut, "The catecholamine hypothesis of affective disorders," American Journal of Psychiatry 122 (1965): 509-22.
40. Valenstein, Blaming the Brain, 82.
41. A. Baumeister, "Historical development of the dopamine hypothesis of schizophrenia," Journal of the History of the Neurosciences 11 (2002): 265-77.
42. Swazey, Chlorpromazine in Psychiatry, 4.
43. Ibid, 8.
44. Ayd, Discoveries in Biological Psychiatry, 215-16.
45. Ibid, 127.
46. Ibid, 195.
366 • NOTES
Chapter 5: The Hunt for Chemical Imbalances
1. T. H. Huxley, Critiques and Addresses (London: Macmillan & Co., 1873), 229.
2. E. Azmitia, "Awakening the sleeping giant," Journal of Clinical Psychiatry 52 (1991), suppl. 12: 4-16.
3. M. Bowers, "Cerebrospinal fluid 5-hydroxyindoleacetic acid and homovanillic acid in psychiatric patients," International Journal of Neuropharmacology 8 (1969): 255-62.
4. R. Papeschi, "Homovanillic and 5-hydroxyindoleacetic acid in cerebrospinal fluid of depressed patients," Archives of General Psychiatry 25 (1971): 354-58.
5. M. Bowers, "Lumbar CSF 5-hydroxyindoleacetic acid and homovanillic acid in af-fective syndromes," Journal of Nervous and Mental Disease 158 (1974): 325-30.
6. D. L. Davies, "Reserpine in the treatment of anxious and depressed patients," Lancet 2 (1955): 117-20.
7. J. Mendels, "Brain biogenic amine depletion and mood," Archives of General Psy-chiatry 30 (1974): 447-51.
8. M. Asberg, "Serotonin depression: A biochemical subgroup within the affective dis-orders?" Science 191 (1976): 478-80; M. Asberg, "5-HIAA in the cerebrospinal fluid," Archives of General Psychiatry 33 (1976): 1193-97.
9. H. Nagayama, "Postsynaptic action by four antidepressive drugs in an animal model of depression," Pharmacology Biochemistry and Behavior 15 (1981): 12530. Also see H. Nagayama, "Action of chronically administered antidepressants on the serotonergic postsynapse in a model of depression," Pharmacology Biochemistry and Behavior 25 (1986): 805-11.
10. J. Maas, "Pretreatment neurotransmitter metabolite levels and response to tricyclic antidepressant drugs," American Journal of Psychiatry 141 (1984): 1159-71.
11. J. Lacasse, "Serotonin and depression: a disconnect between the advertisements and the scientific literature," PloS Medicine 2 (2005): 1211-16.
12. C. Ross, Pseudoscience in Biological Psychiatry (New York: John Wiley & Sons, 1995), 111.
13. Lacasse, "Serotonin and depression."
14. D. Healy, "Ads for SSRI antidepressants are misleading," PloS Medicine news release, November 2005.
15. I. Creese, "Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs," Science 192 (1976): 481-83; P. Seeman, "Antipsychotic drug doses and neuroleptic/dopamine receptors," Nature 261 (19761: 177-79.
16. "Schizophrenia: Vast effort focuses on four areas," New York Times, November 13, 1979.
17. M. Bowers, "Central dopamine turnover in schizophrenic syndromes," Archives of General Psychiatry 31 (1974): 50-54.
18. R. Post, "Cerebrospinal fluid amine metabolites in acute schizophrenia," Archives of General Psychiatry 32 (1975): 1063-68.
19. J. Haracz, "The dopamine hypothesis: an overview of studies with schizophrenic patients," Schizophrenia Bulletin 8 (1982): 438-58.
NOTES • 367
20. T. Lee, "Binding of 31-1-neuroleptics and 3H-apomorphine in schizophrenic brains," Nature 374 (1978): 897-900.
21. D. Burt, "Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain," Science 196 (1977): 326-27.
22. M. Porceddu, "[3H]SCH 23390 binding sites increase after chronic blockade of d-1 dopamine receptors," European Journal of Pharmacology 118 (1985): 367-70.
23. A. MacKay, "Increased brain dopamine and dopamine receptors in schizophrenia," Archives of General Psychiatry 39 (1982): 991-97.
24. J. Kornhuber, "3H-spiperone binding sites in post-mortem brains from schizophrenic patients," Journal of Neural Transmission 75 (1989): 1-10.
25. J. Martinot, "Striatal D2 dopaminergic receptors assessed with positron emission tomography and bromospiperone in untreated schizophrenic patients," American Journal of Psychiatry 147 (1990): 44-50; L. Farde, "D2 dopamine receptors in neuroleptic-naive schizophrenic patients," Archives of General Psychiatry 47 (1990): 213-19; J. Hietala, "Striatal D2 dopamine receptor characteristics in neurolepticnaïve schizophrenic patients studied with positron emission tomography," Archives of General Psychiatry 51 (1994): 116-23.
26. P. Deniker, "The neuroleptics: a historical survey," Acta Psychiatrica Scandinavica 82, suppl. 358 (1990): 83-87. Also: "From chloipromazine to tardive dyskinesia," Psychiatric Journal of the University of Ottawa 14 (1989): 253-59.
27. J. Kane, "Towards more effective antipsychotic treatment," British Journal of Psy-chiatry 165, suppl. 25 (1994): 22-31.
28. E. Nestler and S. Hyman, Molecular Neuropharmacology (New York: McGraw Hill, 2002), 392.
29. J. Mendels, "Brain biogenic amine depletion and mood," Archives of General Psy-chiatry 30 (1974): 447-51.
30. P. Deniker, "The neuroleptics: a historical survey," Acta Psychiatrica Scandinavica 82, suppl. 358(1990): 83-87. Also: "From chlorpromazine to tardive dyskinesia," Psychiatric Journal of the University of Ottawa 14 (1989): 253-59.
31. D. Healy, The Creation of Psychopharmacology (Cambridge, MA: Harvard University Press, 2002), 217.
32. E. Valenstein, Blaming the Brain (New York: The Free Press, 1998), 96.
33. U.S. Department of Health and Human Services, Mental Health: A Report of the Surgeon General (1999), 3, 68, 78.
34. J. Glenmullen, Prozac Backlash (New York: Simon & Schuster, 2000), 196.
35. Lacasse, "Serotonin and depression."
36. R. Fuller, "Effect of an uptake inhibitor on serotonin metabolism in rat brain," Life Sciences 15 (1974): 1161-71.
37. D. Wong, "Subsensitivity of serotonin receptors after long-term treatment of rats with fluoxetine," Research Communications in Chemical Pathology and Pharmacology 32 (1981): 41-51.
38. J. Wamsley, "Receptor alterations associated with serotonergic agents," Journal of Clinical Psychiatry 48, suppl. (1987): 19-25.
368 • NOTES
39. A. Schatzberg, Textbook of Psychopharmacology (Washington, DC: American Psychiatric Press, 1995), 8.
40. C. Montigny, "Modification of serotonergic neuron properties by long-term treatment with serotonin reuptake blockers," Journal of Clinical Psychiatry 51, suppl. B (1990): 4-8.
41. D. Wong, "Subsensitivity of serotonin receptors after long-term treatment of rats with fluoxetine," Research Communications in Chemical Pathology and Pharmacology 32 (1981): 41-51.
42. C. Montigny, "Modification of serotonergic neuron properties by long-term treatment with serotonin reuptake blockers," Journal of Clinical Psychiatry 51, suppl. B (1990): 4-8.
43. R. Fuller, "Inhibition of serotonin reuptake," Federation Proceedings 36 (1977): 2154-58.
44. B. Jacobs, "Serotonin and behavior," Journal of Clinical Psychiatry 52, suppl. (1991): 151-62.
45. Schatzberg, Textbook of Psychopharmacology, 619.
46. S. Hyman, "Initiation and adaptation: A paradigm for understanding psychotropic drug action," American Journal of Psychiatry 153 (1996): 151-61.
Chapter 6: A Paradox Revealed
1. E. Stip, "Happy birthday neuroleptics!" European Psychiatry 17 (2002): 115-19.
2. M. Boyle, "Is schizophrenia what it was?" Journal of the History of Behavioral Science 26 (1990): 323-33; M. Boyle, Schizophrenia: A Scientific Delusion? (New York: Routledge, 1990).
3. P. Popenoe, "In the melting pot," Journal of Heredity 14 (1923): 223.
4. J. Cole, editor, Psychopharmacology (Washington, DC: National Academy of Sciences, 1959), 142.
5. Ibid, 386-87.
6. N. Lehrman, "Follow-up of brief and prolonged psychiatric hospitalization," Com-prehensive Psychiatry 2 (1961): 227-40.
7. R. Warner, Recovery from Schizophrenia (Boston: Routledge & Kegan Paul, 1985), 74.
8. L. Epstein, "An approach to the effect of ataraxic drugs on hospital release rates," American Journal of Psychiatry 119 (1962): 246-61.
9. C. Silverman, The Epidemiology of Depression (Baltimore: Johns Hopkins Press, 1968), 139.
10. J. Swazey, Chlorpromazine in Psychiatry (Cambridge, MA: MIT Press, 1974), 247.
11. Cole, Psychopharmacology, 144,285.
12. Ibid, 285.
13. Ibid, 347.
14. R. Baldessarini, Chemotherapy in Psychiatry (Cambridge, MA: Harvard University Press, 1977), 29.
15. A. Schatzberg, editor, Textbook of Psychopharmacology (Washington, DC: American Psychiatric Press, 1995), 624.
NOTES • 369
16. P. Gilbert, "Neuroleptic withdrawal in schizophrenic patients," Archives of General Psychiatry 52 (1995): 173-88.
17. J. Geddes, "Prevention of relapse," New England Journal of Medicine 346 (2002): 56-58.
18. L. Dixon, "Conventional antipsychotic medications for schizophrenia." Schizophre-nia Bulletin 21 (1995): 567-77.
19. Stip, "Happy birthday, neuroleptics!"
20. N. Schooler, "One year after discharge," American Journal of Psychiatry 123 (1967): 986-95.
21. R. Prien, "Discontinuation of chemotherapy for chronic schizophrenics," Hospital and Community Psychiatry 22 (1971): 20-23.
22. G. Gardos and J. Cole, "Maintenance antipsychotic therapy: is the cure worse than the disease?" American Journal of Psychiatry 133 (1977): 32-36.
23. G. Gardos and J. Cole, "Withdrawal syndromes associated with antipsychotic drugs," American Journal of Psychiatry 135 (1978): 1321-24. Also see Gardos and-Cole, "Maintenance antipsychotic therapy."
24. J. Bockoven, "Comparison of two five-year follow-up studies," American Journal of Psychiatry 132 (1975): 796-801.
25. W. Carpenter, "The treatment of acute schizophrenia without drugs," American Journal of Psychiatry 134 (1977): 14-20.
26. M. Rappaport, "Are there schizophrenics for whom drugs may be unnecessary or contraindicated?" International Pharmacopsychiatry 13 (1978): 100-11.
27. S. Mathews, "A non-neuroleptic treatment for schizophrenia," Schizophrenia Bul-letin 5 (1979): 322-32.
28. J. Bola, "Treatment of acute psychosis without neuroleptics," Journal of Nervous and Mental Disease 191 (2003): 219-29.
29. Carpenter, "The treatment of acute schizophrenia."
30. G. Paul, "Maintenance psychotropic drugs in the presence of active treatment pro-grams," Archives of General Psychiatry 27 (1972): 106-14.
31. T. Van Putten, "The board and care home: does it deserve a bad press?" Hospital and Community Psychiatry 30 (1979): 461-64.
32. Gardos and Cole, "Maintenance antipsychotic therapy."
33. P. Deniker, "Are the antipsychotic drugs to be withdrawn?" in C. Shagass, editor, Biological Psychiatry (New York: Elsevier, 1986), 1-9.
34. G. Chouinard, "Neuroleptic-induced supersensitivity psychosis," American Journal of Psychiatry 135 (1978): 1409-10.
35. G. Chouinard, "Neuroleptic-induced supersensitivity psychosis: Clinical and phar-macologic characteristics," American Journal of Psychiatry 137 (1980): 16-20.
36. G. Chouinard, "Neuroleptic-induced supersensitivity psychosis, the 'Hump Course,' and tardive dyskinesia," Journal of Clinical Psychopharmacology 2 (1982): 143-44.
37. G. Chouinard, "Severe cases of neuroleptic-induced supersensitivity psychosis," Schizophrenia Research 5 (1991): 21-33.
38. P. Muller, "Dopaminergic supersensitivity after neuroleptics," Psychopharmacology 60 (1978): 1-11.
37o • NOTES
39. L. Martensson, "Should neuroleptic drugs be banned?" Proceedings of the World Federation of Mental Health Conference in Copenhagen, 1984, accessed via www.larsmartensson.com, 10/30/08.
40. P. Breggin, Brain Disabling Treatments in Psychiatry (New York: Springer Publishing Company, 1997), 60.
41. S. Snyder, Drugs and the Brain (New York: Scientific American Library, 1986), 88.
42. C. Harding, "The Vermont longitudinal study of persons with severe mental ill-ness," American Journal of Psychiatry 144 (1987): 727-34; C. Harding, "The Vermont longitudinal study of persons with severe mental illness, II," American Journal of Psychiatry 144 (1987): 727-35.
43. P. McGuire, "New hope for people with schizophrenia," APA Monitor 31 (February 2000).
44. C. Harding, "Empirical correction of seven myths about schizophrenia with implications for treatment," Acta Psychiatrica Scandinavica 384, suppl. (1994): 14-16.
45. A. Jablensky, "Schizophrenia: manifestations, incidence and course in different cultures," Psychological Medicine 20, monograph (1992): 1-95.
46. Ibid. See tables on page 60 for medication usage by individual centers; see table on page 64 for medication usage by developing and developed countries.
47. K. Hopper, "Revisiting the developed versus developing country distinction in course and outcome in schizophrenia," Schizophrenia Bulletin 26 (2000): 835-46.
48. J. Wade, "Tardive dyskinesia and cognitive impairment," Biological Psychiatry 22 (1987): 393-95.
49. M. Myslobodsky, "Central determinants of attention and mood disorder in tardive dyskinesia," Brain and Cognition 23 (1993): 56-70.
50. H. Wisniewski, "Neiirofibrillary pathology in brains of elderly schizophrenics treated with neuroleptics," Alzheimer Disease and Associated Disorders 8 (1994): 211-27.
51. M. Chakos, "Increase in caudate nuclei volumes of first-episode schizophrenic pa-tients taking antipsychotic drugs," American Journal of Psychiatry 151 (1994): 1430-36; A. Madsen, "Neuroleptics in progressive structural brain abnormalities in psychiatric illness," Lancet 352 (1998): 784-85; R. Gur, "A follow-up of magnetic resonance imaging study of schizophrenia," Archives of General Psychiatry 55 (1998): 145-52.
52. R. Gur, "Subcortical MRI volumes in neuroleptic-naive and treated patients with schizophrenia," American Journal of Psychiatry 155 (1998): 1711-17.
53. P. Seeman, "Dopamine supersensitivity correlates with D2 HIGH states, implying many paths to psychosis," Proceedings of the National Academy of Science 102 (2005): 3513-18.
54. B. Ho, "Progressive structural brain abnormalities and their relationship to clinical outcome," Archives of General Psychiatry 60 (2003): 585-94.
55. N. Andreasen, "Longitudinal changes in neurocognition during the first decade of schizophrenia illness," International Congress on Schizophrenia Research (2005): 348.
NOTES • 371
56. C. Dreifus, "Using imaging to look at changes in the brain," New York Times,
September 16,2008.
57. T. McGlashan, "Rationale and parameters for medication-free research in psy-chosis," Schizophrenia Bulletin 32 (2006): 300-302.
58. M. Harrow, "Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications," Journal of Nervous and Mental Disease 195
(2007): 406-14.
59. National Institute of Mental Health, "The Numbers Count," accessed at
www.nimh.nih.gov on 3/7/2008.
Chapter 7: The Benzo Trap
1. S. Garfield, "Valium's 40th Birthday," Observer, February 2,2003.
2. E. Shorter, A History of Psychiatry (New York: John Wiley & Sons, 1997), 161,
181.
3. A. Tone, The Age of Anxiety (New York: Basic Books, 2009), 15.
4. American Psychiatry Association, Diagnostic and Statistical Manual of Mental Disorders (1952), 31.
5. C. Silverman, The Epidemiology of Depression (Baltimore: Johns Hopkins Press,
1968), 139.
6. L. Hollister, "Drugs for emotional disorders," Journal of the American Medical As-sociation 234 (1975): 942-47.
7. E Ayd Jr., Discoveries in Biological Psychiatry (Philadelphia: Lippincott, 1970), 127.
8. D. Greenblatt, "Meprobamate: a study of irrational drug use," American Journal of Psychiatry 127 (1971): 33-39.
9. C. Essig, "Addiction to nonbarbiturate sedative and tranquillizing drugs," Clinical Pharmacology & Therapeutics 5 (1964): 334-43.
10. "Letdown for Miltown," Time, April 30,1965.
11. Tone, The Age of Anxiety, 171.
12. M. Smith, Small Comfort (New York: Praeger, 1985), 78.
13. Tone, The Age of Anxiety, 172.
14. G. Cant, "Valiumania," New York Times, February 1,1976.
15. R. Hughes, The Tranquilizing of America (New York: Harcourt Brace Jovanovich,
1979), 8.
16. Tone, The Age of Anxiety, 176.
17. Committee on the Review of Medicines, "Systematic review of the benzodiazepines," British Medical Journal 280 (1980): 910-12.
18. Editorial, "Benzodiazepines on trial," British Medical Journal 288 (1984): 1101-12.
19. Smith, Small Comfort, 32.
20. S. Stahl, "Don't ask, don't tell, but benzodiazepines are still the leading treatments for anxiety disorder," Journal of Clinical Psychiatry 63 (2002): 756-67.
21. IMS Health, "Top therapeutic classes by U.S. dispensed prescriptions," 2006 and 2007 reports.
22. K. Solomon, "Pitfalls and prospects in clinical research on antianxiety drugs," Journal of Clinical Psychiatry 39 (1978): 823-31.
372 • NOTES
23. A. Shapiro, "Diazepam: how much better than placebo?" Journal of Psychiatric Re-search 17 (1983): 51-73.
24. C. Gudex, "Adverse effects of benzodiazepines," Social Science & Medicine 33 (1991): 587-96.
25. J. Martin, "Benzodiazepines in generalized anxiety disorder," Journal of Psy-chopharmacology 21 (2007): 774-82.
26. Malcolm Lader interview, January 12, 2009.
27. B. Maletzky, "Addiction to diazepam," International Journal of Addictions 11 (1976): 95-115.
28. A. Kales, "Rebound insomnia," Science 201 (1978): 1039-40.
29. H. Petursson, "Withdrawal from long-term benzodiazepine treatment," British Medical Journal 283 (1981): 643-35.
30. H. Ashton, "Benzodiazepine withdrawal," British Medical Journal 288 (1984): 1135-40.
31. H. Ashton, "Protracted withdrawal syndromes from benzodiazepines," Journal of Substance Abuse Treatment 9 (1991): 19-28.
32. P. Cowen, "Abstinence symptoms after withdrawal of tranquillising drugs," Lancet 2, 8294 (1982): 360-62.
33. H. Ashton, "Benzodiazepine withdrawal," British Medical Journal 288 (1984): 1135-40.
34. H. Ashton, Benzodiazepines: How They Work and How to Withdraw (Newcastle upon Tyne: University of Newcastle, 2000), 42.
35. H. Ashton, "Protracted withdrawal syndromes from benzodiazepines," Journal of Substance Abuse Treatment 9 (1991): 19-28.
36. K. Rickels, "Long-term benzodiazepine users 3 years after participation in a discontinuation program," American Journal of Psychiatry 148 (1991): 757-61.
37. K. Rickels, "Psychomotor performance of long-term benzodiazepine users before, during, and after benzodiazepine discontinuation," Journal of Clinical Psychophar-macology 19 (1999): 107-13.
38. S. Patten, "Self-reported depressive symptoms following treatment with cortico-steroids and sedative-hypnotics," International Journal of Psychiatry in Medicine 26 (1995): 15-24.
39. Ashton, Benzodiazepines, 8.
40. A. Pelissolo, "Anxiety and depressive disorders in 4,425 long term benzodiazepine users in general practice," Encephale 33 (2007): 32-38.
41. Hughes, The Tranquilizing of America, 17.
42. S. Golombok, "Cognitive impairment in long-term benzodiazepine users," Psycho-logical Medicine 18 (1988): 365-74.
43. M. Barker, "Cognitive effects of long-term benzodiazepine use," CNS Drugs 18 (2004): 37-48.
44. WHO Review Group, "Use and abuse of benzodiazepines," Bulletin of the World Health Organization 61 (1983): 551-62.
45. Maletzky, "Addiction to diazepam." NOTES • 373
46. R. Caplan, "Social effects of diazepam use," Social Science & Medicine 21 (1985): 887-98.
47. H. Ashton, "Tranquillisers," British Journal of Addiction 84 (1989): 541-46.
48. Ashton, Benzodiazepines, 12.
49. Stevan Gressitt interview, January 9, 2009.
SO. U.S. Department of Health & Human Services, SAMHSA, Mental Health, United States (2002).
S1. Government Accountability Office, Young Adults with Serious Mental Illness, June 2008.
52. R. Vasile, "Results of a naturalistic longitudinal study of benzodiazepine and SSRI use in the treatment of generalized anxiety disorder and social phobia," Depression and Anxiety 22 (2005): 59-67.
53. Malcolm Lader interview, January 12, 2009.
Chapter 8: An Episodic Illness Turns Chronic
1. C. Dewa, "Depression in the workplace," A Report to the Ontario Roundtable on Appropriate Prescribing, November 2001.
2. A. Solomon, The Noonday Demon (New York: Simon & Schuster, 2001), 289.
3. C. Goshen, editor, Documentary History of Psychiatry (New York: Philosophical Library, 1967), 118-20.
4. Solomon, The Noonday Demon, 286.
5. E. Wolpert, editor, Manic-Depressive Illness (New York: International Universities Press, 1997), 34.
6. C. Silverman, The Epidemiology of Depression (Baltimore: Johns Hopkins Press, 1968), 44, 139. The first-admission and residence data in Silverman's book is for all manic-depressive patients; the unipolar patients comprised about 75 percent of that total.
7. Ibid, 79, 142.
8. F. Ayd, Recognizing the Depressed Patient (New York: Grune & Stratton, 1961), 13.
9. A. Zis, "Major affective disorder as a recurrent illness," Archives of General Psychiatry 36 (1979): 835-39.
10. G. Winokur, Manic Depressive Illness (St. Louis: The C.V. Mosby Company, 1969), 19-20.
11. T. Rennie, "Prognosis in manic-depressive psychoses," American Journal of Psychi-atry 98 (1941): 801-14. See table on page 811.
12. G. Lundquist, "Prognosis and course in manic-depressive psychoses," Acta Psychi-atrica Scandinavica, suppl. 35 (1945): 7-93.
13. D. Schuyler, The Depressive Spectrum (New York: Jason Aronson, 1974), 49.
14. J. Cole, "Therapeutic efficacy of antidepressant drugs," Journal of the American Medical Association 190 (1964): 448-55.
15. N. Kline, "The practical management of depression," Journal of the American Medical Association 190 (1964): 122-30.
374 • NOTES
16. Winokur, Manic Depressive Illness, 19.
17. Schuyler, The Depressive Spectrum, 47.
18. Medical Research Council, "Clinical trial of the treatment of depressive illness," British Medical Journal 1 (1965): 881-86.
19. A. Smith, "Studies on the effectiveness of antidepressant drugs," Psychopharmacology Bulletin S (1969): 1-53.
20. A. Raskin, "Differential response to chlorpromazine, imipramine, and placebo," Archives of General Psychiatry 23 (1970): 164-73.
21. R. Thomson, "Side effects and placebo amplification," British Journal of Psychiatry 140 (1982): 64-68.
22. I. Elkin, "NIMH treatment of depression collaborative research program," Archives of General Psychiatry 47 (1990): 682-88.
23. A. Khan, "Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials," Archives of General Psychiatry 57 (2000): 311-17.
24. E. Turner, "Selective publication of antidepressant trials and its influence on apparent efficacy," New England Journal of Medicine 358 (2008): 252-60.
25. I. Kirsch, "Initial severity and antidepressant benefits," PLoS Medicine 5 (2008): 260-68.
26. G. Parker, "Antidepressants on trial," British Journal of Psychiatry 194 (2009): 1-3.
27. C. Barbui, "Effectiveness of paroxetine in the treatment of acute major depression in adults," Canadian Medical Association Journal 178 (2008): 296-305.
28. J. Ioannidis, "Effectiveness of antidepressants," Philosophy, Ethics, and Humanities in Medicine 3 (2008): 14.
29. Hypericum Trial Study Group, "Effect of Hypericum perforatum in major depressive disorder," Journal of the American Medical Association 287 (2002): 1807-14.
30. J.D. Van Scheyen, "Recurrent vital depressions," Psychiatria, Neurologia, Neuro-chirurgia 76 (1973): 93-112.
31. Ibid.
32. R. Mindham, "An evaluation of continuation therapy with tricyclic antidepressants in depressive illness," Psychological Medicine 3 (1973): 5-17.
33. M. Stein, "Maintenance therapy with amitriptyline," American Journal of Psychiatry 137 (1980): 370-71.
34. R. Prien, "Drug therapy in the prevention of recurrences in unipolar and bipolar af-fective disorders," Archives of General Psychiatry 41 (1984): 1096-1104. See table 6 and figure 2.
35. M. Shea, "Course of depressive symptoms over follow-up," Archives of General Psychiatry 49 (1992): 782-87.
36. A. Viguera, "Discontinuing antidepressant treatment in major depression," Harvard Review of Psychiatry 5 (1998): 293-305.
37. P. Haddad, "Antidepressant discontinuation reactions," British Medical Journal 316 (1998): 1105-6.
38. G. Fava, "Do antidepressant and antianxiety drugs increase chronicity in affective disorders?" Psychotherapy and Psychosomatics 61 (1994): 125-31.
NOTES • 375
39. G. Fava, "Can long-term treatment with antidepressant drugs worsen the course of depression?" Journal of Clinical Psychiatry 64 (2003): 123-33.
40. Ibid.
41. G. Fava, "Holding on: depression, sensitization by antidepressant drugs, and the prodigal experts," Psychotherapy and Psychosomatics 64 (1995): 57-61; G. Fava, "Potential sensitizing effects of antidepressant drugs on depression," CNS Drugs 12
(1999): 247-56.
42. R. Baldessarini, "Risks and implications of interrupting maintenance psychotropic drug therapy," Psychotherapy and Psychosomatics 63 (1995): 137-41.
43. R. EI-Mallakh, "Can long-term antidepressant use be depressogenic?" Journal of Clinical Psychiatry 60 (1999): 263.
44. "Editorial sparks debate on effects of psychoactive drugs," Psychiatric News, May
20,1994.
45. Consensus Development Panel, "Mood disorders," American Journal of Psychiatry
142 (1985): 469-76.
46. R. Hales, editor, Textbook of Psychiatry (Washington, DC: American Psychiatric
Press, 1999), 525.
47. J. Geddes, "Relapse prevention with antidepressant drug treatment in depressive disorders," Lancet 361 (2003): 653-61.
48. L. Judd, "Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness?" American Journal of Psychiatry 157 (2000): 1501-4.
49. R. Tranter, "Prevalence and outcome of partial remission in depression," Journal of Psychiatry and Neuroscience 27 (2002): 241-47.
50. Hales, Textbook of Psychiatry, 547.
Si. J. Rush, "One-year clinical outcomes of depressed public sector outpatients," Biological Psychiatry 56 (2004): 46-53.
52. Ibid.
53. D. Warden, "The star*d project results," Current Psychiatry Reports 9 (2007):
449-59.
54. NIMH, Depression (2007): 3. (NIH Publication 07-3561.)
55. D. Deshauer, "Selective serotonin reuptake inhibitors for unipolar depression," Canadian Medical Association Journal 178 (2008): 1293-1301.
56. C. Ronalds, "Outcome of anxiety and depressive disorders in primary care," British Journal of Psychiatry 171 (1997): 427-33.
57. E. Weel-Baumgarten, "Treatment of depression related to recurrence," Journal of Clinical Pharmacy and Therapeutics 25 (2000): 61-66.
58. S. Patten, "The impact of antidepressant treatment on population health," Population Health Metrics 2 (2004): 9.
59. D. Goldberg, "The effect of detection and treatment on the outcome of major de-pression in primary care," British Journal of General Practice 48 (1998): 1840-44.
60. Dewa, "Depression in the workplace."
61. W. Coryell, "Characteristics and significance of untreated major depressive disorder," American Journal of Psychiatry 152 (1995): 1124-29.
376 • NOTES
62. J. Moncrieff, "Trends in sickness benefits in Great Britain and the contribution of mental disorders," Journal of Public Health Medicine 22 (2000): 59-67.
63. T. Helgason, "Antidepressants and public health in Iceland," British Journal of Psychiatry 184 (2004): 157-62.
64. R. Rosenheck, "The growth of psychopharmacology in the 1990s," International Journal of Law and Psychiatry 28 (2005): 467-83.
65. M. Posternak, "The naturalistic course of unipolar major depression in the absence of somatic therapy," Journal of Nervous and Mental Disease 194 (2006): 324-49.
66. Ibid. Also see M. Posternak, "Untreated short-term course of major depression," Journal of Affective Disorders 66 (2001): 139-46.
67. J. Cole, editor, Psychopharmacology (Washington, DC: National Academy of Sci-ences, 1959), 347.
68. NIMH, "The numbers count," accessed at www.nimh.nih.gov on 3/7/2008; W. Eaton, "The burden of mental disorders," Epidemiologic Reviews 30 (2008): 1-14.
69. M. Fava, "A cross-sectional study of the prevalence of cognitive and physical symptoms during long-term antidepressant treatment," Journal of Clinical Psychiatry 67 (2006): 1754-59.
70. M. Kalia, "Comparative study of fluoxetine, sibutramine, sertraline and defenflu-ramine on the morphology of serotonergic nerve terminals using serotonin immuno-histochemistry," Brain Research 858 (2000): 92-105. Also see press release by Thomas Jefferson University Hospital, "Jefferson scientists show several serotoninboosting drugs cause changes in some brain cells," 2/29/2000.
Chapter 9: The Bipolar Boom
1. D. Healy, Mania (Baltimore: Johns Hopkins University Press, 2008), 16,41,43.
2. I calculated these estimates by applying the 25 percent figure to the 1955 data on patients in state and county mental hospitals with a diagnosis of manic-depressive illness.
3. C. Silverman, The Epidemiology of Depression (Baltimore: Johns Hopkins University Press, 1968), 139.
4. G. Winokur, Manic Depressive Illness (St. Louis: The C.V. Mosby Company, 1969), 19.
S. F. Wertham, "A group of benign chronic psychoses," American Journal of Psychiatry 9 (1929): 17-78.
6. G. Lundquist, "Prognosis and course in manic-depressive psychoses," Acta Psychiatrica Scandinavica, suppl. 35 (1945): 7-93.
7. M. Tsuang, "Long-term outcome of major psychoses," Archives of General Psychiatry 36 (1979): 1295-1301.
8. Winokur, Manic Depressive Illness, 21.
9. NIMH, The Numbers Count: Mental Disorders in America, accessed at www.nimh.nih.gov on 3/7/2008.
10. C. Baethge, "Substance abuse in first-episode bipolar I disorder," American Journal of Psychiatry 162 (2005): 1008-10; E. Frank, "Association between illicit drug and
NOTES • 377
alcohol use and first manic episode," Pharmacology Biochemistry and Behavior 86 (2007): 395-400.
11. S. Strakowski, "The effects of antecedent substance abuse on the development of first-episode psychotic mania," Journal of Psychiatric Research 30 (1996): 59-68.
12. J. Goldberg, "Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability," Journal of Clinical Psychiatry 69 (2008): 1751-57.
13. M. Van Laar, "Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population?" Addiction 102 (2007): 1251-60.
14. G. Crane, "The psychiatric side effects of iproniazid," American Journal of Psychiatry 112 (1956): 494-501.
15. J. Angst, "Switch from depression to mania," Psychopathology 18 (1985): 140-54.
16. American Psychiatric Association, Practice Guidelines for Major Depressive Disor-der in Adults (Washington, DC: APA, 1993), 22.
17. A. Martin, "Age effects on antidepressant-induced manic conversion," Archives of Pediatrics & Adolescent Medicine 158 (2004): 773-80.
18. J. Goldberg, "Risk for bipolar illness in patients initially hospitalized for unipolar depression," American Journal of Psychiatry 158 (2001): 1265-70.
19. R. El-Mallakh, "Use of antidepressants to treat depression in bipolar disorder," Psy-chiatric Services 53 (2002): 58-84.
20. Interview with Fred Goodwin, "Advances in the diagnosis and treatment of bipolar disorder," Primary Psychiatry, accessed via Internet on 3/6/09 at primarypsychiatry.com.
21. G. Fava, "Can long-term treatment with antidepressant drugs worsen the course of depression?" Journal of Clinical Psychiatry 64 (2003): 123-33.
22. L. Judd, "The prevalence and disability of bipolar spectrum disorders in the US pop-ulation," Journal of Affective Disorders 73 (2003): 123-31.
23. J. Angst, "Toward a re-definition of subthreshold bipolarity," Journal of Affective Disorders 73 (2003): 133-46.
24. Ibid; Judd, "The prevalence and disability."
25. R. Fieve, Moodswing (New York: William Morrow and Company, 1975), 13.
26. For a history of lithium, see Healy, Mania, and J. Moncrieff, The Myth of the Chem-ical Cure (New York: Palgrave MacMillan, 2008).
27. S. Tyrer, "Lithium in the treatment of mania," Journal of Affective Disorders 8 (1985): 251-57.
28. J. Baker, "Outcomes of lithium discontinuation," Lithium 5 (1994): 187-92.
29. R. Baldessarini, "Discontinuing lithium maintenance treatment in bipolar disorders," Bipolar Disorders 1 (1999): 17-24.
30. G. Faedda, "Outcome after rapid v. gradual discontinuation of lithium treatment in bipolar disorders," Archives of General Psychiatry 50 (1993): 448-55.
31. J. Himmelhoch, "On the failure to recognize lithium failure," Psychiatric Annals 24 (1994): 241-50.
32. J. Moncrieff, The Myth of the Chemical Cure (London: Palgrave Macmillan, 2008), 199.
378 • NOTES
33. G. Goodwin, "Recurrence of mania after lithium withdrawal," British Journal of Psychiatry 164 (1994): 149-52.
34. H. Markar, "Efficacy of lithium prophylaxis in clinical practice," British Journal of Psychiatry 155 (1989): 496-500; J. Moncrieff, "Lithium revisited," British Journal of Psychiatry 167 (1995): 569-74.
35. J. Goldberg, "Lithium treatment of bipolar affective disorders under naturalistic fol-lowup conditions," Psychopharmacology Bulletin 32 (1996): 47-54.
36. M. Gitlin, "Relapse and impairment in bipolar disorder," American Journal of Psy-chiatry 152 (199S): 1635-40.
37. J. Moncrieff, "Lithium: evidence reconsidered," British Journal of Psychiatry 171 (1997): 113-19.
38. F. Goodwin, Manic-Depressive Illness (New York: Oxford University Press, 1990), 647.
39. A. Zis, "Major affective disorder as a recurrent illness," Archives of General Psychiatry 36 (1979): 835-39.
40. A. Koukopoulos, "Rapid cyclers, temperament, and antidepressants," Comprehensive Psychiatry 24 (1983): 249-58.
41. N. Ghaemi, "Diagnosing bipolar disorder and the effect of antidepressants," Journal of Clinical Psychiatry 61 (2000): 804-809.
42. N. Ghaemi, "Antidepressants in bipolar disorder," Bipolar Disorders 5 (2003): 421-33.
43. R. El-Mallakh, "Use of antidepressants to treat depression in bipolar disorder," Psy-chiatric Services 53 (2002): 580-84.
44. A. Koukopoulos, "Duration and stability of the rapid-cycling course," Journal of Affective Disorders 72 (2003): 75-85.
45. R. El-Mallakh, "Antidepressant-associated chronic irritable dysphoria in bipolar disorder," Journal of Affective Disorders 84 (2005): 267-72.
46. N. Ghaemi, "Treatment of rapid-cycling bipolar disorder," American Journal of Psychiatry 165 (2008): 300-301.
47. C. Schneck, "The prospective course of rapid-cycling bipolar disorder," American Journal of Psychiatry 165 (2008): 370-77.
48. L. Judd, "The long-term natural history of the weekly symptomatic status of bipolar
I disorder," Archives of General Psychiatry 59 (2002): 530-37.
49. L. Judd, "A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder," Archives of General Psychiatry 60 (2003): 261-69.
50. R. Joffe, "A prospective, longitudinal study of percentage of time spent ill in patients with bipolar I or bipolar II disorders," Bipolar Disorders 6 (2004): 62-66.
51. R. Post, "Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method," Journal of Clinical Psychiatry 64 (2003): 680-90.
52. L. Judd, "Residual symptom recovery from major affective episodes in bipolar dis-orders and rapid episode relapse/recurrence," Archives of General Psychiatry 65 (2008): 386-94.
NOTES • 379
53. C. Zarate, "Functional impairment and cognition in bipolar disorder," Psychiatric Quarterly 71 (2000): 309-29.
54. Gitlin, "Relapse and impairment."
55. P. Keck, "12-month outcome of patients with bipolar disorder following hospital-ization for a manic or a mixed episode," American Journal of Psychiatry 155
(1998): 646-52.
56. D. Kupfer, "Demographic and clinical characteristics of individuals in a bipolar disorder case registry," Journal of Clinical Psychiatry 63 (2002): 120-25.
57. N. Huxley, "Disability and its treatment in bipolar disorder patients," Bipolar Dis-
orders 9 (2007): 183-96.
58. T. Goldberg, "Contrasts between patients with affective disorders and patients with schizophrenia on a neuropsychological test battery," American Journal of Psychia-
try 150 (1993): 1355-62.
59. J. Zihl, "Cognitive deficits in schizophrenia and affective disorders," Acta Psychiatrica Scandinavica 97 (1998): 351-57.
60. F. Dickerson, "Outpatients with schizophrenia and bipolar I disorder," Psychiatry Research 102 (2001): 21-27.
61. G. Malhi, "Neuropsychological deficits and functional impairment in bipolar de-pression, hypomania and euthymia," Bipolar Disorders 9 (2007): 114-25.
62. V. Balanza-Martinez, "Persistent cognitive dysfunctions in bipolar I disorder and schizophrenic patients," Psychotherapy and Psychosomatics 74 (2005): 113-19; A Martinez-Aran, "Functional outcome in bipolar disorder," Bipolar Disorders 9
(2007): 103-13.
63. M. Pope, "Determinants of social functioning in bipolar disorder," Bipolar Disor-
ders 9 (2007): 38-44.
64. C. Zarate, "Antipsychotic drug side effect issues in bipolar manic patients," Journal of Clinical Psychiatry 61, suppl. 8 (2000): 52-61.
65. C. Zarate, "Functional impairment and cognition in bipolar disorder," Psychiatric Quarterly 71 (2000): 309-29.
66. D. Kupfer, "The increasing medical burden in bipolar disorder," Journal of the American Medical Association 293 (2005): 2528-30.
67. L. Citrome, "Toward convergence in the medication treatment of bipolar disorder and schizophrenia," Harvard Review of Psychiatry 13 (2005): 28-42.
68. Huxley, "Disability and its treatment."
69. M. Harrow, "Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications," Journal of Nervous and Mental Disorders 195
(2007): 406-14.
70. W. Eaton, "The burden of mental disorders," Epidemiology Review 30 (2008):
1-14.
Chapter 10: An Epidemic Explained
1. Interview with Amy Upham, June 14, 2009.
2. M. Morgan, "Prospective analysis of premature mortality in schizophrenia in relation to health service engagement," Psychiatry Research 117 (2003): 127-35;
380 • NOTES
C. Colton, "Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states," Preventing Chronic Disease 3 (April 2006).
3. S. Saha, "A systematic review of mortality in schizophrenia," Archives of General Psychiatry 64 (2007): 1123-31; L. Appleby, "Sudden unexplained death in psychiatric in-patients," British Journal of Psychiatry 176 (2000): 405-406; M. Joukamaa, "Schizophrenia, neuroleptic medication, and mortality," British Journal of Psychiatry 188 (2006): 122-27.
Chapter 11: The Epidemic Spreads to Children
1. B. Carey, "What's wrong with a child? Psychiatrists often disagree," New York Times, November 11,2006.
2. R. Kessler, "Mood disorders in children and adolescents," Biological Psychiatry 49 (2001): 1002-14.
3. J. O'Neal, Child and Adolescent Psychopharmacology Made Simple (Oakland, CA: New Harbinger Publications, 2006), 6.
4. R. Mayes, Medicating Children (Cambridge, MA: Harvard University Press, 2009), 46.
5. G. Jackson, "Postmodern psychiatry," unpublished paper, September 2,2002.
6. Mayes, Medicating Children, 54.
7. Ibid, 61.
8. R. Mayes, "ADHD and the rise in stimulant use among children," Harvard Review of Psychiatry 16 (2008): 151-66.
9. G. Golden, "Role of attention deficit hyperactivity disorder in learning disabilities," Seminars in Neurology 11 (1991): 35-41.
10. NIH Consensus Development Conference statement, "Diagnosis and treatment of attention deficit hyperactivity disorder," November 16-18,1998.
11. P. Breggin, Talking Back to Ritalin (Cambridge, MA: Perseus Publishing, 2001), 180.
12. S. Hyman, "Initiation and adaptation: a paradigm for understanding psychotropic drug action," American Journal of Psychiatry 153 (1996): 151-61.
13. Breggin, Talking Back to Ritalin, 83.
14. H. Rie, "Effects of methylphenidate on underachieving children," Journal of Con-sulting and Clinical Psychology 44 (1976): 250-60.
15. C. Cunningham, "The effects of methylphenidate on the mother-child interactions of hyperactive identical twins," Developmental Medicine & Child Neurology 20 (1978): 634-42.
16. N. Fiedler, "The effects of stimulant drugs on curiosity behaviors of hyperactive boys," Journal of Abnormal Child Psychology 11 (1983): 193-206.
17. T. Davy, "Stimulant medication and short attention span," Journal of Developmental & Behavioral Pediatrics 10 (1989): 313-18.
18. D. Granger, "Perceptions of methylphenidate effects on hyperactive children's peer interactions," Journal of Abnormal Child Psychology 21 (1993): 535-49.
NOTES • 381
19. J. Swanson, "Effects of stimulant medication on learning in children with ADHD," Journal of Learning Disabilities 24 (1991): 219-30.
20. Breggin, Talking Back to Ritalin, 92.
21. J. Richters, "NIMH Collaborative Multisite Multimodal Treatment Study of Children with ADHD," Journal of the American Academy of Child & Adolescent Psychiatry 34 (1995): 987-1000.
22. T. Spencer, "Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle," Journal of the American Academy of Child & Adolescent Psychiatry 35 (1996): 409-32.
23. E. Sleator, "How do hyperactive children feel about taking stimulants and will they tell the doctor?" Clinical Pediatrics 21 (1982): 474-79.
24. D. Jacobvitz, "Treatment of attentional and hyperactivity problems in children with sympathomimetic drugs," Journal of the American Academy of Child & Adolescent Psychiatry 29 (1990): 677-88.
25. A. Sroufe, "Treating problem children with stimulant drugs," New England Journal of Medicine 289 (1973): 407-13.
26. Ibid.
27. Rie, "Effects of methylphenidate."
28. R. Barkley, "Do stimulant drugs improve the academic performance of hyperkinetic children?" Clinical Pediatrics 8 (1978): 137-46.
29. Swanson, "Effects of stimulant medication."
30. C. Whalen, "Stimulant pharmacotherapy for attention-deficit hyperactivity disorders," in S. Fishberg and R. Greenberg, eds., From Placebo to Panacea (New York: John Wiley & Sons, 1997), 329.
31. R. Schachar, "Attention-deficit hyperactivity disorder," Canadian Journal of Psychi-atry 47 (2002): 337-48.
32. Whalen, "Stimulant pharmacotherapy," 327.
33. P. Breggin, "Psychostimulants in the treatment of children diagnosed with ADHD," International Journal of Risk & Safety in Medicine 12 (1993): 3-35.
34. Ibid.
35. Richters, "NIMH Collaborative Multisite."
36. P. Jensen, "3-year follow-up of the NIMH MTA study," Journal of the American Academy of Child & Adolescent Psychiatry 46 (2007): 989-1002. See chart on page 997 for medication use.
37. The MTA Cooperative Group, "A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder," Archives of General Psychiatry 56 (1999): 1073-86.
38. Jensen, "3-year follow-up."
39. B. Molina, "Delinquent behavior and emerging substance use in the MTA at 36 months," Journal of the American Academy of Child & Adolescent Psychiatry 46 (2007): 1028-39.
40. B. Molina, "MTA at 8 years," Journal of the American Academy of Child & Ado-lescent Psychiatry 48 (2009): 484-500.
382 • NOTES
41. C. Miranda, "ADHD drugs could stunt growth," Daily Telegraph (UK), November 12,2007.
42. Breggin, Talking Back to Ritalin; K. Bolla, "The neuropsychiatry of chronic cocaine abuse," Journal of Neuropsychiatry and Clinical Neurosciences 10 (1998): 280-89.
43. S. Castner, "Long-lasting psychotomimetic consequences of repeated low-dose amphetamine exposure in rhesus monkeys," Neuropsychopharmacology 20 (1999): 10-28.
44. W. Carlezon, "Enduring behavioral effects of early exposure to methylphenidate in rats," Biological Psychiatry 54 (2003): 1330-37.
45. C. Bolanos, "Methylphenidate treatment during pre- and periadolescence alters be-havioral responses to emotional stimuli at adulthood," Biological Psychiatry 54 (2003): 1317-29.
46. J. Zito, "Rising prevalence of antidepressants among US youths," Pediatrics 109 (2002): 721-27.
47. R. Fisher, From Placebo to Panacea (New York: John Wiley & Sons, 1997), 309.
48. T. Delate, "Trends in the use of antidepressants in a national sample of commercially insured pediatric patients, 1998 to 2002," Psychiatric Services 55 (2004): 387-91.
49. Editorial, "Depressing research," Lancet 363 (2004): 1335.
50. T. Laughren, Memorandum, "Background comments for Feb. 2,2004 meeting of psychopharmacological drugs advisory committee," January 5,2004. Accessed at fda.gov.
Si. J. Leo, "The SSRI trials in children," Ethical Human Psychology and Psychiatry 8 (2006): 29-41.
52. C. Whittington, "Selective serotonin reuptake inhibitors in childhood depression," Lancet 363 (2004): 1341-45.
53. Editorial, "Depressing research," Lancet 363 (2004): 1335.
54. J. Jureidini, "Efficacy and safety of antidepressants for children and adolescents," British Medical Journal (2004): 879-83.
55. T. Wilens, "A systematic chart review of the nature of psychiatric adverse events in children and adolescents treated with selective serotonin reuptake inhibitors," Journal of Child and Adolescent Psychopharmacology 13 (2003): 143-52.
56. T. Gualtieri, "Antidepressant side effects in children and adolescents," Journal of Child and Adolescent Psychopharmacology 16 (2006): 147-57.
57. P. Breggin, Brain-Disabling Treatments in Psychiatry (New York: Springer Publishing Company, 2008), 153.
58; D. Papolos, The Bipolar Child (New York: Broadway Books, 2000), xiv.
59. C. Moreno, "National trends in the outpatient diagnosis and treatment of bipolar disorder in youth," Archives of General Psychiatry 64 (2007): 1032-39.
60. J. Kluger, "Young and Bipolar," Time, August 19,2002.
61. L. Lurie, "Psychoses in children," Journal of Pediatrics 36 (1950): 801-9.
62. Ibid.
63. B. Hall, "Our present knowledge about manic-depressive states in childhood," Ner-vous Child 9 (1952): 319-25.
NOTES • 383
64. J. Anthony, "Manic-depressive psychosis in childhood," Journal of Child Psychol-ogy and Psychiatry 1 (1960): 53-72.
65. W. Weinberg, "Mania in childhood," American Journal of Diseases of Childhood 130 (1976): 380-85.
66. R. DeLong, "Lithium carbonate treatment of select behavior disorders in children suggesting manic-depressive illness," Journal of Pediatrics 93 (1978): 689-94.
67. M. Strober, "Bipolar illness in adolescents with major depression," Archives of General Psychiatry 39 (1982): 549-55.
68. P. Lewinsohn, "Bipolar disorders in a community sample of older adolescents," Journal of the American Academy of Child & Adolescent Psychiatry 34 (1995): 454-63.
69. G. Carlson, "Manic symptoms in psychiatrically hospitalized children-what do they mean?" Journal of Affective Disorders 51 (1998): 123-35.
70. J. Kluger, "Young and Bipolar."
71. D. Janowsky, "Proceedings: effect of intravenous d-amphetamine, 1-amphetamine and methylphenidate in schizophrenics," Psychopharmacology Bulletin 19 (1974): 15-24.
72. E. Cherland, "Psychotic side effects of psychostimulants," Canadian Journal of Psychiatry 44 (1999): 811-13.
73. K. Gelperin, "Psychiatric adverse events associafed with drug treatment of ADHD," FDA, Center for Drug Evaluation and Research, March 3,2006.
74. D. Papolos, "Bipolar disorder, co-occuring conditions, and the need for extreme caution before initiating drug treatment," Bipolar Child Newsletter 1 (November 1999).
75. M. DelBello, "Prior stimulant treatment in adolescents with bipolar disorder," Bipolar Disorders 3 (2001): 53-57.
76. J. Biederman, "Attention-deficit hyperactivity disorder and juvenile mania," Journal of the American Academy of Child & Adolescent Psychiatry 35 (1996): 997-1008.
77. J. Jain, "Fluoxetine in children and adolescents with mood disorders," Journal of Child & Adolescent Psychopharmacology 2 (1992): 259-65.
78. G. Emslie, "A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression," Archives of General Psychiatry 54 (1997): 1031-37.
79. P. Breggin, The Anti-Depressant Fact Book (Cambridge, MA: Perseus Publishing, 2001), 116.
80. A. Martin, "Age effects on antidepressant-induced manic conversion," Archives of Pediatrics & Adolescent Medicine 158 (2004): 773-80.
81. G. Faedda, "Pediatric onset bipolar disorder," Harvard Review of Psychiatry 3 (1995): 171-95.
82. B. Geller, "Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder," American Journal of Psychiatry 158 (2001): 125-27.
83. D. Cicero, "Antidepressant exposure in bipolar children," Psychiatry 66 (2003): 317-22.
84. D. Papolos, "Antidepressant-induced adverse effects in juvenile-onset bipolar
384 • NOTES
disorder," paper presented at the Fifth International Conference on Bipolar Disorder, June 12-14, 2003, Pittsburgh, PA.
85. G. Faedda, "Pediatric bipolar disorder," Bipolar Disorders 6 (2004): 305-13.
86. M. Hellander, "Children with bipolar disorder," Journal of the American Academy of Child & Adolescent Psychiatry 38 (1999): 495.
87. H. Marano, "Crisis on the campus," Psychology Today, May 2, 2002.
88. C. Reichart, "Earlier onset of bipolar disorder in children by antidepressants or stimulants," Journal of Affective Disorders 78 (2004): 81-84. Also see abstracts presented at the Fourth International Conference on Bipolar Disorder in Pittsburgh, June 2001.
89. B. Geller, "Child and adolescent bipolar disorder," Journal of the American Academy of Child & Adolescent Psychiatry 36 (1997): 1168-76.
90. Papolos, "Antidepressant-induced adverse effects."
91. G. Faedda, "Treatment-emergent mania in pediatric bipolar disorder," Journal of Affective Disorders (82): 149-58.
92. R. Perlis, "Long-term implications of early onset in bipolar disorder," Biological Psychiatry 55 (2004): 875-81.
93. B. Birmaher, "Course and outcome of bipolar spectrum disorder in children and adolescents," Development and Psychopathology 18 (2006): 1023-35.
94. M. DelBello, "Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode," American Journal of Psychiatry 164 (2007): 582-90.
95. T. Goldstein, "Psychosocial functioning among bipolar youth," Journal of Affective Disorders 114 (2009): 174-83.
96. B. Geller, "Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype," American Journal of Psychiatry 159 (2002): 927-33.
97. "Hayes says new treatments for pediatric bipolar disorder not ready for prime time" (December 3, 2008 press release), accessed at hayesinc.com, August 2, 2009.
98. Social Security Administration, annual statistical reports on the SSI program, 1996-2008; Social Security Bulletin, Annual Statistical Supplement, 1988-1992.
99. Pediatric Academic Societies, "Pediatric psychiatry admissions on the rise," May 16, 2000, press release.
100. D. Satcher, Report of Surgeon General's Conference on Children's Mental Health (U.S. Dept. of Health and Human Services, 2001).
101. B. Whitford, "Depression, eating disorders and other mental illnesses are on the rise," Newsweek, August 27, 2008.
102. U.S. Government Accountability Office, "Young adults with serious mental illness" (June 2008).
Chapter 12: Suffer the Children
1. J. Zito, "Psychotropic medication patterns among youth in foster care," Pediatrics 121 (2008): 157-63.
NOTES • 385
Chapter 13: The Rise of an Ideology
1. C. Ross, Pseudoscience in Psychiatry (New York: John Wiley & Sons, 1995).
2. G. Klerman, "A debate on DSM-III," American Journal of Psychiatry 141 (1984): 539-42.
3. M. Sabshin, "Report of the medical director," American Journal of Psychiatry 137 (1980): 1308.
4. See blurbs for second edition of The Myth of Mental Illness, published by Harper & Row in 1974.
5. B. Nelson, "Psychiatry's anxious years," New York Times, November 2, 1982.
6. D. Adler, "The medical model and psychiatry's tasks," Hospital and Community Psychiatry 32 (1981): 387-92.
7. Sabshin, "Report of the medical director."
8. Nelson, "Psychiatry's anxious years."
9. Copy from a Smith Kline and French advertisement that ran monthly in Mental Hospitals in 1962.
10. L. Thorne, "Inside Russia's psychiatric jails," New York Times Magazine, June 12, 1977.
11. U.S. Senate, Committee on the Judiciary, Subcommittee to Investigate Juvenile Delinquency, Drugs in Institutions, 94th Cong., 1st sess., 1975.
12. A. Tone, The Age of Anxiety (New York: Basic Books, 2009), 176.
13. M. Smith, Small Comfort (New York: Praeger, 1985), 32.
14. Interview with Arthur Platt, June 8, 2009.
15. M. Sabshin, "On remedicalization and holism in psychiatry," Psychosomatics 18 (1977): 7-8.
16. A. Ludwig, "The medical basis of psychiatry," American Journal of Psychiatry 134 (1977): 1087-92.
17. P. Blaney, "Implications of the medical model and its alternatives," American Journal of Psychiatry 132 (1975): 911-14.
18. S. Guze, "Nature of psychiatric illness," Comprehensive Psychiatry 19 (1978): 295-307.
19. Adler, "The medical model."
20. M. Wilson, "DSM-III and the transformation of American psychiatry," American Journal of Psychiatry 150 (1993): 399-410.
21. S. Kirk, The Selling of DSM (New York: Aldine de Gruyter, 1992), 114.
22. Ibid, 134.
23. M. Sabshin, "Turning points in twentieth-century American psychiatry," American Journal of Psychiatry (1990): 1267-74.
24. Klerman, "A debate on DSM-III."
25. J. Maxmen, The New Psychiatrists (New York: New American Library, 1985), 35, 31.
26. H. Kutchins, Making Us Crazy (New York: The Free Press, 1997), 248.
27. Kirk, The Selling of DSM, 115.
28. M. Sabshin, "Report of the medical director" (1980), 1308.
386 • NOTES
29. L. Havens, "Twentieth-century psychiatry," American Journal of Psychiatry 138 (1981): 1279-87.
30. B. Bursten, "Rallying 'round the medical model," Hospital and Community Psychiatry 32 (1981): 371.
31. Sources for this political battle include reviews by NIMH's "Clinical Programs Projects Research Review Committee" on April 27, 1970; April 1-2, 1973; April 1974; April 21, 1975; June 27, 1977; December 1, 1977; February 17-18, 1978; and June 26-27, 1978.
32. Interview with Loren Mosher, December 1, 2000.
33. M. Sabshin, "Report of the medical director," American Journal of Psychiatry 138 (1981): 1418-21.
34. P. Breggin, Toxic Psychiatry (New York: St. Martin's Press, 1991), 360.
35. Sabshin, "Report of the medical director" (1981).
36. M. Sabshin, "Report of the medical director," American Journal of Psychiatry 140 (1983): 1398-1403.
37. R. Peele, "Report of the speaker-elect," American Journal of Psychiatry 143 (1986): 1348-50.
38. M. Sabshin, "Report of the medical director," American Journal of Psychiatry 143 (1986): 1342-46.
39. M. Sabshin, "Report of the medical director," American Journal of Psychiatry 145 (1988): 1338-42.
40. Sabshin, "Report of the medical director" (1981).
41. M. Sabshin, Changing American Psychiatry (Washington, DC: American Psychiatric Publishing, Inc., 2008), 78.
42. Sabshin, "Report of the medical director" (1983).
43. Sabshin, "Report of the medical director" (1986).
44. New York Times, November 26, 1981; September 7, 1982; July 29, 1984.
45. J. Franklin, "The Mind-Fixers," Baltimore Evening Sun, July 1984.
46. M. Gold, The Good News About Depression (New York: Villard Books, 1987), xi-xiii.
47. N. Andreasen, The Broken Brain (New York: Harper & Row, 1984), 29-30.
48. Ibid, 138.
49. Franklin, "The Mind-Fixers."
50. Sabshin, Changing American Psychiatry, 194.
51. M. Dumont, "In bed together at the market," American Journal of Orthopsychiatry 60 (1990):. 484-85.
52. F. Gottlieb, "Report of the speaker," American Journal of Psychiatry 142 (1985): 1246-49.
53. Breggin, Toxic Psychiatry, 46, 357.
54. P. Breggin, Medication Madness (New York: St. Martin's Press, 2008), 150.
55. S. Boseley, "Scandal of scientists who take money for papers ghostwritten by drug companies," Guardian, February 7, 2002.
56. M. Angel, "Is academic medicine for sale?" New England Journal of Medicine 342 (2000): 1516-18.
NOTES • 387
57. D. Regier, "The NIMH depression awareness, recognition, and treatment program," American Journal of Psychiatry 145 (1988): 1351-57.
58. Breggin, Toxic Psychiatry, 14.
59. E. Foulks, "Advocating for persons who are mentally ill," Administration and Policy in Mental Health and Mental Health Services Research 27 (2000): 353-67.
60. A. Hatfield, "The National Alliance for the Mentally Ill," Community Mental Health Journal 27 (1991): 95-103.
61. E. Benedek, "Report of the secretary," American Journal of Psychiatry 144 (1987): 1381-88.
62. Breggin, Toxic Psychiatry, 363.
63. Foulks, "Advocating for persons."
64. K. Silverstein, "Prozac.org," Mother Jones, November/December 1999.
65. R. Behar, "The thriving cult of greed and power," Time, May 6, 1991.
Chapter 14: The Story That Was ... and Wasn't Told
1. D. Healy, Mania (Baltimore: Johns Hopkins University Press, 2008), 132.
2. G. Carson, The Roguish World of Doctor Brinkley (New York: Rinehart & Co., 1960).
3. P. Breggin, Brain-Disabling Treatments in Psychiatry (New York: Springer Publishing Co., 2008), 390.
4. "Fluoxetine project team meeting," July 31, 1978, accessed at healyprozac.com. S. "Fluoxetine project team meeting," July 23, 1979, accessed at healyprozac.com.
6. J. Cornwell, The Power to Harm (New York: Viking, 1996), 147-48.
7. D. Healy, Let Them Eat Prozac (New York: New York University Press, 2004), 39.
8. Ibid, 128.
9. Ibid, 249,
10. BGA letter to Eli Lilly, May 25, 1984, Forsyth v. Eli Lilly trial documents, exhibit 42. See baumhedlundlaw.com/media/timeline.
11. Forsyth v. Eli Lilly trial documents, exhibit 58.
12. Cornwell, The Power to Harm, 198.
13. Healy, Let Them Eat Prozac, 35.
14. P. Breggin, Talking Back to Prozac (New York: St. Martin's Press, 1994), 41.
15. Ibid, 46.
16. Ibid, 90. Also see P. Breggin, Brain-Disabling Treatments in Psychiatry, 79, 86, 91.
17. D. Graham, "Sponsor's ADR submission on fluoxetine dated July 17, 1990," FDA document, September 1990.
18. T. Moore, "Hard to Swallow," Washingtonian, December 1997.
19. D. Kessler, "Introducing MEDWatch," Journal of the American Medical Association 269 (1993): 2765-68.
20. J. Bremner, "Fluoxetine in depressed patients," Journal of Clinical Psychiatry 45 (1984): 414-19.
21. J. Feigner, "A comparative trial of fluoxetine and amitriptyline in patients with major depressive disorder," Journal of Clinical Psychiatry 46 (1985): 369-72.
388 • NOTES
22. J. Cohn, "A comparison of fluoxetine, imipramine, and placebo in patients with major depressive disorder," Journal of Clinical Psychiatry 46 (1985): 26-31.
23. J. Wernicke, "The side effect profile and safety of fluoxetine," Journal of Clinical Psychiatry 46 (1985): 59-67.
24. P. Stark, "A review of multicenter controlled studies of fluoxetine vs. imipramine and placebo in outpatients with major depressive disorder," Journal of Clinical Psychiatry 46 (1985): 53-58.
25. S. Levine, "A comparative trial of a new antidepressant, fluoxetine," British Journal of Psychiatry 150 (1987): 653-55.
26. R. Pary, "Fluoxetine: prescribing guidelines for the newest antidepressant," South-ern Medical Journal 82 (1989): 1005-9.
27. D. Regier, "The NIMH depression awareness, recognition and treatment program," American Journal of Psychiatry 145 (1988): 1351-57.
28. Healy, Let Them Eat Prozac, 9.
29. F. Schumer, "Bye-Bye, Blues," New York, December 18, 1989.
30. G. Cowley, "Prozac: A Breakthrough Drug for Depression," Newsweek, March 26, 1990.
31. N. Angier, "New antidepressant is acclaimed but not perfect," New York Times, March 29, 1990.
32. B. Duncan, "Exposing the mythmakers," Psychotherapy Networker, March/April 2000.
33. M. Waldholz, "Prozac said to spur idea of suicide," Wall Street Journal, July 18, 1990.
34. Ibid. Also see S. Shellenbarger, "Eli Lilly stock plunges $4.375 on news of another lawsuit over Prozac drug," Wall Street Journal, July 27, 1990.
35. Memo from Leigh Thompson to Allan Weinstein, February 7, 1990, accessed at healyprozac.com
36. Memo from Mitch Daniels to Leigh Thompson, "Upcoming TV appearance," April 15, 1991, accessed at healyprozac.com.
37. Ibid.
38. T. Burton, "Medical flap: Anti-depression drug of Eli Lilly loses sales after attack by sect," Wall Street Journal, April 19, 1991.
39. L. Garnett, "Prozac revisited," Boston Globe, May 7, 2000.
40. R. Behar, "The Thriving Cult of Greed and Power," Time, May 6, 1991.
41. T. Burton, "Panel finds no credible evidence to tie Prozac to suicides and violent behavior," Wall Street Journal, September 23, 1991.
42. S. Begley, "Beyond Prozac," Newsweek, February 7, 1994.
43. P. Breggin, Toxic Psychiatry (New York: St. Martin's Press, 1991), 348-50. In this book, Breggin detailed the bad science involved in the Xanax trials, the co-opting of academic psychiatry, and the involvement of the APA in marketing the drug.
44. "High Anxiety," Consumer Reports, January 1993.
45. C. Ballenger, "Alprazolam in panic disorder and agoraphobia," Archives of General Psychiatry 45 (1988): 413-22.
NOTES • 389
46. R. Noyes, "Alprazolam in panic disorder and agoraphobia," Archives of General Psychiatry 45 (1988): 423-28.
47. J. Pecknold, "Alprazolam in panic disorder and agoraphobia," Archives of General Psychiatry 45 (1988): 429-36.
48. Ballenger, "Alprazolam in panic disorder."
49. Noyes, "Alprazolam in panic disorder."
50. Pecknold, "Alprazolam in panic disorder."
51. I. Marks, "The 'efficacy' of alprazolam in panic disorder and agoraphobia," Archives of General Psychiatry 46 (1989): 668-72.
52. I. Marks, "Reply to comment on the London/Toronto study," British Journal of Psychiatry 162 (1993): 790-94.
53. Breggin, Toxic Psychiatry, 344-53.
54. E Pollner, "Don't overlook panic disorder," Medical World News, October 1, 1991.
55. J. Randal, "In a panic?" St. Louis Post-Dispatch, October 7, 1990.
56. H. Brown, "Panic attacks keeps thousands from malls, off roads," Associated Press, November 19, 1990.
57. R. Davis, "When panic is disabling," Chicago Sun-Times, June 29, 1992.
58. "High Anxiety," Consumer Reports.
59. FDA reviews of risperidone data included the following written commentaries: reviews by Andrew Mosholder, May 11, 1993, and November 7, 1993; David Hoberman, April 20, 1993; and Thomas Laughren, December 20, 1993.
60. Approval letter from Robert Temple to Janssen Research Foundation, December 29, 1993.
61. S. Marder, "The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis," Journal of Clinical Psychiatry 58 (1997): 538-46.
62. "New hope for schizophrenia," Washington Post, February 16, 1993.
63. "Seeking safer treatments for schizophrenia," New York Times, January 15, 1992.
64. FDA reviews of olanzapine data included the following written commentaries: reviews by Thomas Laughren on September 27, 1996; by Paul Andreason on July 29 and September 26, 1996; and by Paul Leber on August 18 and August 30, 1996.
65. C. Beasley, "Efficacy of olanzapine," Journal of Clinical Psychiatry 58, suppl. 10 (1997): 7-12.
66. "Psychosis drug from Eli Lilly racks up gains," Wall Street Journal, April 14, 1998.
67. "A new drug for schizophrenia wins approval from the FDA," New York Times, October 2, 1996.
68. "Schizophrenia, close-up of the troubled brain," Parade, November 21, 1999.
69. "Mental illness aid," Chicago Tribune, June 4, 1999.
70. "Lives recovered," Los Angeles Times, January 30, 1996.
71. P. Weiden, Breakthroughs in Antipsychotic Medications (New York: W.W. Norton, 1999), 26
72. Wall Street Journal, "Psychosis drug from Eli Lilly."
73. "High Anxiety," Consumer Reports.
390 • NOTES
74. J. Lieberman, "Effectiveness of antipsychotic drugs in patients with schizophrenia," New England Journal of Medicine (2005): 1209-33.
75. L. Davies, "Cost-effectiveness of first- v. second-generation antipsychotic drugs." British Journal of Psychiatry 191 (2007): 14-22.
76. P. Tyrer, "The spurious advance of antipsychotic drug therapy," Lancet 373 (2009): 4-5.
77. Interview with Peter Breggin, October 10, 2008.
78. Healy interview on CBS News and Current Affairs, June 12, 2001.
79. D. Healy, "Psychopharmacology and the government of the self," talk given November 30, 2000, at the University of Toronto.
80. E-mail from David Goldbloom to David Healy, December 7, 2000.
81. Interview with Healy by e-mail, July 4, 2009.
82. Memo from Larry Carpman to Steve Kurkjian, April 11, 2000.
83. "Science News from 2007," NIMH website, accessed on July 2, 2009.
84. NIMH press release, July 20, 2007.
85. J. Sharkey, "Delusions; paranoia is universal," New York Times, August 2, 1998.
86. Search of NAMI website on July 7, 2009.
87. R. Hales, The American Psychiatric Publishing Textbook of Psychiatry (Arlington, VA: American Psychiatric Publishing, 2008).
Chapter 15: Tallying Up the Profits
1. D. Carlat, "Dr. Drug Rep," New York Times, November 25, 2007.
2. NAMI IRS 990 Form, 2000.
3. B. Koerner, "First you market the disesase, then you push the pills to treat it," Guardian, July 30, 2002.
4. E. Tanouye, "Antidepressant makers study kids' market," Wall Street Journal, April 4, 1997.
5. B. Strauch, "Use of antidepression medicine for young patients has soared," New York Times, August 10, 1997.
6. Tanouye, "Antidepressant makers."
7. Deposition of Joseph Biederman in legal case of Avila v. Johnson & Johnson Co., February 26, 2009, pages 139, 231, 232, 237.
8. J. Biederman, "Attention-deficit hyperactivity disorder and juvenile mania," Journal of the American Academy of Child & Adolescent Psychiatry 35 (1996): 997-1008.
9. Deposition of Joseph Biederman, p. 158.
10. Margaret Williams, report on a sales call, May 17, 2002.
11. J. J. Zorc, "Expenditures for psychotropic medications in the United States in 1985," American Journal of Psychiatry 148 (1991): 644-47
12. "Top therapeutic classes by U.S. sales, 2008," IMS Health.
13. S. Giled, "Better but not best," Health Affairs 28 (2009): 637-48.
14. These calculations are based on Eli Lilly's annual 10-K reports filed with the SEC from 1987 to 2000. Capitalization figures for 1987 and 2000 are based on prices in the fourth quarter of each year.
15. J. Pereira, "Emory professor steps down," Wall Street Journal, December 23, 2008. NOTES • 391
16. C. Schneider, "Emory psychiatrist reprimanded over outside work," Atlanta Journal-Constitution, June 11, 2009.
17. G. Harris, "Radio host has drug company ties," New York Times, November 22, 2008.
18. GlaxoSmithKline internal memo, "Seroxat/Paxil adolescent depression. Position piece on the phase III studies," October 1998.
19. M. Keller, "Efficacy of paroxetine in the treatment of adolescent major depression," Journal of the American Academy of Child & Adolescent Psychiatry 40 (2001): 762-72.
20. E. Ramshaw, "Senator questions doctors' ties to drug companies," Dallas Morning News, September 24, 2008.
21. L. Kowalczyk, "US cites Boston psychiatrist in case vs. drug firm," Boston Globe, March 6, 2009.
22. G. Harris, "Lawmaker calls for registry of drug firms paying doctors," New York Times, August 4, 2007.
23. G. Harris, "Researchers fail to reveal full drug pay," New York Times, June 8, 2008.
24. Avila v. Johnson & Johnson, deposition of Joseph Biederman, February 26, 2009, 119.
25. J. Biederman, Annual Report 2002: The Johnson & Johnson Center for Pediatric Psychopathology at the Massachusetts General Hospital.
26. J. Olson, "Drug makers step up giving to Minnesota psychiatrists," Pioneer Press, August 27, 2007.
27. Margaret Williams, reports on sales calls, April 20, 2001, and April 8, 2002.
28. Eli Lilly grant registry, 2009, 1st quarter.
29. E. Mundell, "U.S. spending on mental health care soaring," HealthDay, August 6, 2009.
30. T. Mark, "Mental health treatment expenditure trends, 1986-2003," Psychiatric Services 58 (2007): 1041-48. Seven percent of national health expenditures in 2008 went to mental health services; by 2015, this figure is expected to rise to 8 percent. Data on national health expenditures in 2008, and projected expenditures in 2015, are from the U.S. Department of Health and Human Services.
Chapter 16: Blueprints for Reform
1. MindFreedom, "Original statement by the fast for freedom in mental health," July 28, 2003.
2. Letter from James Scully to David Oaks, August 12, 2003.
3. Letter from MindFreedom scientific panel to James Scully, August 22, 2003.
4. APA statement on "diagnosis and treatment of mental disorders," September 26, 2003.
S. Letter from MindFreedom scientific panel to James Scully, December 15, 2003.
6. Interview with David Oaks, October 4, 2009.
7. J. Modrow, How to Become a Schizophrenic (Seattle: Apollyon Press, 1992), ix.
8. Interview with David Healy in Bangor, Wales, September 4, 2009.
9. D. Healy, "Psychiatric bed utilization," Psychological Medicine 31 (2001): 779-90;
392 • NOTES
D. Healy, "Service utilization in 1896 and 1996," History of Psychiatry 16 (2005): 37-41. Also, Healy, unpublished data on readmission rates for first-episode psychosis, 1875-1924, and 1994-2003.
10. Interviews with Yrjo Alanen, Jukka Aaltonen, and Viljo Rakkolainen in Turku, Finland, September 7,2009.
11. V. Lehtinen, "Two-year outcome in first-episode psychosis treated according to an integrated model," European Psychiatry 15 (2000): 312-20.
12. Interview with Jaakko Seikkula in Jyvaskyla, Finland, September 9,2009.
13. J. Seikkula, "Five year experience of first-episode nonaffective psychosis in open-dialogue approach," Psychotherapy Research 16 (2006): 214-28. Also see: J. Seikkula, "A two-year follow-up on open dialogue treatment in first episode psychosis," Society of Clinical Psychology 10 (2000): 20-29; J. Seikkula, "Open dialogue, good and poor outcome," Journal of Constructivist Psychology 14 (2002): 267-86; J. Seikkula, "Open dialogue approach: treatment principles and preliminary results of a two-year follow-up on first episode schizophrenia," Ethical Human Sciences Services 5 (2003): 163-82.
14. Interviews with staff at Keropudas Hospital in Tornio, Finland, September 10 and 11,2009.
15. Outcomes for 2002-2006 study and for spending in western Lapland on psychiatric services from interviews with Jaakko Seikkula and Birgitta Alakare. See also the published papers by Seikkula, op. cit.
16. J. Cullberg, "Integrating intensive psychosocial therapy and low dose medical treat-ment in a total material of first episode psychotic patients compared to treatment as usual," Medical Archives 53 (1999): 167-70.
17. W. Buchan, Domestic Medicine (Boston: Otis, Broaders, and Co., 1846), 307.
18. National Institute for Health and Clinical Excellence, "Depression," December 2004.
19. Interview with Andrew McCulloch in London, September 3,2009.
20. F. Dimeo, "Benefits from aerobic exercise in patients with major depression," British Journal of Sports Medicine 35 (2001): 114-17; K. Knubben, "A randomized, controlled study on the effects of a short-term endurance training programme in patients with major depression," British Journal of Sports Medicine 41 (2007): 29-33; A. Strohle, "Physical activity, exercise, depression and anxiety disorders," Journal of Neural Transmission 116 (2009): 777-84.
21. J. Blumenthal, "Effects of exercise training on older patients with major depression," Archives of Internal Medicine 159 (1999): 2349-56.
22. Ibid.
23. Interviews with Tony Stanton and staff at Seneca Center in San Leandro, California, July 13 and 14,2009.
24. Interviews with Keith Scott and Chris Gordon, Framingham, Massachusetts, October 1,2009.
25. Ibid.
26. Interview with Jim Gottstein in Anchorage, Alaska, May 10,2009. NOTES • 393
27. M. Ford; "The psychiatrist's double bind," American Journal of Psychiatry 137
(1980): 332-39.
28. Myers v. Alaska Psychiatric Institute, Alaska Supreme Court No. S-11021.
29. Interview with Susan Musante in Anchorage, Alaska, May 10,2009.
Epilogue
1. E. Whipple, Character and Characteristic Men (Boston: Ticknor & Fields, 1866), 1.
By Steve Rudd: Contact the author for comments, input or corrections.
Send us your story about your experience with modern Psychiatry